Jaundice in the Healthy Newborn
Cord Bilirubin Levels
Normal Serum Bilirubin Levels and the Natural History of Neonatal Jaundice
It is difficult to agree on what represents a “normal bilirubin level” in the term and near-term infant. TSB levels vary considerably, depending on the racial composition of the population, the incidence of breast-feeding, and other genetic and epidemiologic factors (see Table 35-13 and Fig. 35-15). An additional important factor is the large variation found in the laboratory measurements of serum bilirubin, a problem that has been recognized for four decades and currently is unresolved (282,283,284) (see Laboratory Measurements of Bilirubin below).
Reference to Fig. 35-15 gives some idea of the range of mean bilirubin values found in different populations and the natural history of neonatal jaundice. Since the advent of exchange transfusion and, more recently, phototherapy, it has been impossible to obtain a true picture of the natural history of neonatal bilirubinemia because we treat some infants with rising TSB levels in the first 72 to 96 hours so that what we see is, ultimately, a “damped” picture. Recognizing these limitations, however, some recent studies have helped to clarify the picture (285,286).
An important change in the United States population has been the dramatic increase in breast-feeding at hospital discharge, from 30% in the 1960s to 65% in 2001 (287). In some hospitals, 85% or more of mothers are nursing their
infants on discharge from the hospital. Data from the CPP conducted from 1955 to 1961 (when 30% or fewer mothers breast-fed their infants) and more recent studies (254) found that approximately 95% of all infants had a TSB concentration that did not exceed 12.9 mg/dL (215 μmol/L), and this (95th percentile) became the accepted upper limit of “physiologic jaundice” (205).
infants on discharge from the hospital. Data from the CPP conducted from 1955 to 1961 (when 30% or fewer mothers breast-fed their infants) and more recent studies (254) found that approximately 95% of all infants had a TSB concentration that did not exceed 12.9 mg/dL (215 μmol/L), and this (95th percentile) became the accepted upper limit of “physiologic jaundice” (205).
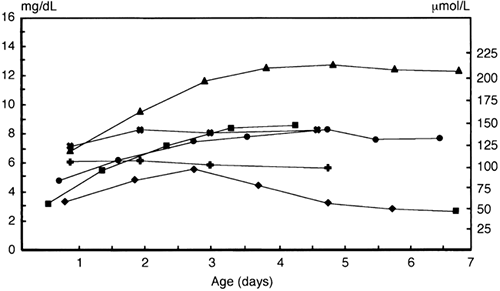 Figure 35-15 Mean total daily bilirubin concentrations in normal full-term and near-term infants. ▼, Fifty healthy Japanese newborn infants, 37 to 42 weeks of gestation, all breast-fed. Excludes Rh and ABO incompatibility (292). ˆ, One hundred seventy-six term breast-fed Canadian infants. Excludes Rh hemolytic disease, but includes nine ABO incompatible infants with positive Coombs tests. Seventeen infants received phototherapy. ˆ, One hundred sixty-four Canadian term formula-fed infants, seven ABO incompatible with positive Coombs tests, and three who received phototherapy (280). ◊, One thousand eighty-seven term Israeli infants, 78% fully or partially breast-fed (Siedman D, personal communication, 1998) ˆ, Fifty-six Nigerian term appropriate for gestational age infants. Excludes ABO or Rh incompatibility and G6PD deficiency. Infants were “largely breast-fed” (291). (◊), Twenty-nine full-term American infants, all formula-fed, approximately 50% African American and 50% white (30).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|