Materials and Methods
Sources
Literature searches were conducted in databases to include MEDLINE, Embase, ClinicalTrials.gov , and the Cochrane Library to retrieve randomized controlled trials on any postoperative preventative measures on intrauterine adhesions formation after hysteroscopy. The searches were not limited by language, with dates included from 1990 to 2014 to give a broad review of 25 years of published literature and include studies that were likely to reflect relatively modern surgical techniques. One study from 1989 returned in the search and was included in the review . Key words and search strategy are in the Supplemental Addendum .
Study selection
Inclusion criteria were established prior to performing the literature search, and the systematic review was not registered in PROSPERO, the international prospective register of systematic reviews. Inclusion criteria were published randomized controlled trials evaluating intrauterine adhesions prevention with any postoperative intervention. Postoperative hysteroscopic evaluation of adhesion formation was required for inclusion. There were no other inclusion criteria based on age, subject population, or surgical indication. Exclusion criteria included publications of abstracts only, nonrandomized controlled trials or failure to report randomization, duplicate publications, review articles, or book chapters.
There were 2 authors (M.W.H. and M.J.H.) who independently screened the studies with 1 disagreement noted in the included studies. A third author (M.T.C.) assisted in the discrepancy decision for included studies, and the 1 study was ultimately excluded because it contained a preoperative and not a postoperative intervention for adhesion prevention.
The search yielded 73 total publications. The 73 abstracts were reviewed and 54 were excluded based on clear failure to meet inclusion criteria. There were 19 full-text articles that were evaluated for inclusion and exclusion criteria. Of these, 7 full-text articles were further excluded for not meeting inclusion criteria. Furthermore, 12 studies were chosen for inclusion in the systematic review and 8 studies in the meta-analysis. Only studies that were similar in methodology or clinical outcomes were included in the meta-analysis.
The 2 authors (M.W.H. and M.J.H.) also evaluated study quality as well as potential for bias. Specifically, attention was placed on randomization methods, concealment of allocation, double blinding of providers and patients, treatment, outcomes, data reporting, and declaration of conflicts of interest.
Data collection
Data were extrapolated separately by 2 authors (M.W.H. and M.T.C.) and further confirmed with a third author (B.S.). Data to include the type of surgical instruments used during the initial operative hysteroscopy, therapy type, and time to follow-up hysteroscopy to evaluate for formation of intrauterine adhesions were extracted from the source articles. Severity of adhesions was based on intrauterine adhesions staging, according to the American Fertility Society. Furthermore, data on fertility outcomes were extracted to include pregnancy rates and miscarriage.
Data synthesis
Outcomes were evaluated for the presence or absence of postoperative adhesion formation (dichotomous), postoperative adhesion scores based on the American Fertility Society scoring system (continuous), pregnancy, and miscarriage. Heterogeneity was evaluated for each outcome and reported as a P value using the Q test and as percentages using the I 2 index values.
Random-effects models were used for meta-analysis if the I 2 index was >50% or if clinical heterogeneity was noted in patient indication for surgery or methodology between studies. Fixed-effects models were used for meta-analysis if the I 2 index was <50% and studies had clinical homogeneity in patient indication for surgery or methodology between studies.
The meta-analysis was not performed when study methodology or clinical outcomes demonstrated extreme heterogeneity because such studies likely represent data inappropriate for statistical synthesis. The risk of bias was evaluated using qualitative assessments of study quality. Dichotomous outcomes were reported as relative risks with 95% confidence intervals and continuous data reported as weighted means with 95% confidence intervals.
Data collection was performed in Excel (Microsoft Office; Microsoft Inc, Richmond, WA) and statistical analysis was performed using Mix Pro 2.0. P values for dichotomous outcomes in the source studies were calculated using vassarstats.net when not provided in the original papers.
This study was instituional review board exempt because of the systematic review and meta-analysis nature of the paper.
Results
Selection of studies for meta-analysis
Abstracts from 73 papers were reviewed, of which 19 papers were further evaluated in detail ( Supplemental Figure 1 ). There were 7 studies that were excluded after review of the full text articles: 1 study evaluated adhesions with hysterosalpingogram only in patients not pregnant 8 months postoperatively, 3 were not randomized controlled trials, 1 was a duplicate from a prior publication included in the review, 1 was published only as an abstract, and 1 study included a randomized and nonrandomized arm and evaluated presurgical danazole for adhesion prevention. Thus, 12 randomized controlled trials met inclusion criteria and were included in the systematic review. Furthermore, 8 studies compared similar preventative intrauterine adhesions methods and were included in the meta-analysis.
There was a lack of similar trials comparing the use of an intrauterine balloon, an intrauterine device, or other adhesions prevention barriers. Thus, these therapies were included in the systematic review but were not included in the meta-analysis data synthesis. There were 3 studies that evaluated hyaluronic acid gel, 3 studies that evaluated estradiol valerate, and 2 studies that evaluated polyethylene oxide-sodium carboxymethylcellulose gel.
Assessment of bias
Of all the studies, 5 failed to report on allocation concealment and may have been at risk for participation bias ( Supplemental Table 1 ). There were 8 studies that did not blind investigators to subject group assignment and may have been at risk for performance and ascertainment bias. Furthermore, 5 studies did not have complete data reporting of patient dropout or loss to follow-up.
There were 2 trials that reported their outcomes on an intent-to-treat basis, and both had no patients lost to follow-up. There were 2 studies that had a 21% patient dropout and may have been at risk for attrition bias. Fuchs et al had a similar dropout between the groups, making it unlikely that retention bias affected the results. Tonguc et al had dropout rates from 0% to 44% in the various arms of the study, placing it at risk for retention bias. The remaining studies that had complete data reporting had between 0% and 9% subject dropout. The majority of subject dropout across all studies was due to failure to follow up for a second-look hysteroscopy.
Hyaluronic acid gel
There were 3 studies that evaluated hyaluronic acid gel for adhesion prevention ( Supplemental Table 2 ). Guida et al evaluated the prevention after polypectomy, myomectomy, or septum resection; Acunzo et al evaluated the prevention after septum resection; and De Iaco et al incorporated all of these same procedures. The incidence of postoperative adhesion formation ranged from 22% to 32% in the control groups and from 10% to 18% in the treatment groups ( Table 1 ). Of these studies, 2 reported a significant reduction in the presence of intrauterine adhesions with the intrauterine application of hyaluronic acid.
| Study | Therapy type | Control, n, % adhesions | Treatment, n, % adhesions | P value | ||
|---|---|---|---|---|---|---|
| Acunzo et al, 2003 | Hyaluronic acid | 41 | 31.7% | 43 | 13.95% | < .05 |
| Amer et al, 2010 | Intrauterine balloon vs plus fresh amnion graft vs plus dry amnion graft | 15 | 14.0% | Fresh amnion, 15 dry amnion, 5 | 10.7% 13.3% | .27 |
| Dabirashrafi et al, 1995 | Conjugated estrogen | 23 | 0% | 23 | 0% | NS |
| Fuchs et al, 2014 | Oxiplex/AP gel | 26 | 14.0% | 26 | 4% | .30 |
| Guida et al, 2004 | Hyaluronic acid | 69 | 26.15% | 69 | 10.44% | < .05 |
| De Iaco et al, 2003 | Hyaluronic acid | 22 | 21.8% | 18 | 17.8% | .78 |
| Kim et al, 2012 | Carboxymethylcellulose hyaluronic acid gel | 95 | 17.9% | 92 | 9.1 | .18 |
| Pabuccu et al, 1997 | Intrauterine device | 35 | 82.8% | 36 | 8.3% | < .05 |
| Roy et al, 2014 | Estradiol valerate | 45 | 6.9% | 45 | 0% | .24 |
| Sardo et al, 2011 | Oxiplex/AP gel | 55 | 22.0% | 55 | 6% | < .05 |
| Tonguc et al, 2010 | Estrogen therapy intrauterine device | 25 | 5.3% | Estrogen, 16 IUD, 19 Estrogen plus IUD, 25 | 0% 10.5% 12% | .50 |
| Vercellini et al, 1989 | Estrogen and intrauterine device | 10 | 0% | 10 | 0% | 1.0 |
Guida et al reported a 10% rate of intrauterine adhesions in the treatment group compared with 26% in the control group ( P < .05). Acunzo et al reported a 14% rate of intrauterine adhesions in the treatment group compared with 32% in the control group. The reported P value was P < .05; however, with a 2 tail test, this comparison is not statistically significant ( P = .06). De Iaco et al reported similar rates of intrauterine adhesions in the control group (22%) compared with the hyaluronic treatment group (18%).
A meta-analysis with a random-effects model demonstrated a significant decrease in intrauterine adhesions when using hyaluronic acid gel (relative risk, 0.44, 95% confidence interval, 0.22–0.77). Minimal heterogeneity was suggested by the result of the Q test (Q = 1.3, P = .52) and the I 2 index (I 2 value = 0%, 95% confidence interval, 0–90%).
In these studies looking at hyaluronic acid gel for adhesion prevention, 2 studies also evaluated postoperative adhesion scores. Guida et al reported a lower mean adhesion score of 2.4 in the hyaluronic acid group compared with a score of 3.8 in the treatment group ( P < .05). Acunzo et al reported a lower mean adhesion score of 2.0 in the hyaluronic acid group compared with a score of 6.2 in the treatment group ( P < .05). A meta-analysis was not performed in these studies because of the extremely high heterogeneity (I 2 value = 98%, 95% confidence interval, 0–100%).
The 3 studies evaluating hyaluronic acid did not follow up patients for pregnancy or miscarriage outcomes.
The 2 studies demonstrating benefit of hyaluronic acid gel for adhesion prevention were performed by the same investigator group of authors at the University of Naples (Naples, Italy). The study that showed no benefit was performed by a different research group at the University of Bologna (Bologna, Italy). A sensitivity analysis removing the studies from the Naples group leaves a single study that demonstrates no benefit of hyaluronic acid gel for adhesion prevention.
There is a lack of reproducible evidence that hyaluronic acid may decrease the incidence and severity of postoperative intrauterine adhesions. The impact of its use on pregnancy outcomes has not been evaluated. The data are inconsistent across 3 studies including 252 subjects. All 3 studies were between unclear to high risk of bias because of the lack of outcomes blinding. There were no low-risk studies for bias stratification.
Polyethylene oxide-sodium carboxymethylcellulose gel
There were 2 studies that evaluated polyethylene oxide-sodium carboxymethylcellulose gel for adhesion prevention. Di Spiezio Sardo et al evaluated prevention in patients with polypectomy, myomectomy, septum resection, and endometrial ablation. Fuchs et al evaluated adhesion prevention in patients, with missed abortion being managed with hysteroscopic resection. Di Spiezio Sardo et al reported a significant reduction in the incidence of postoperative intrauterine adhesions with the treatment group with 6% postoperative intrauterine adhesions compared with 22% in the no treatment group ( P < .05). However, Fuchs et al found no significant difference between the treatment group with 4% and the control group with 14% ( P = .80).
A meta-analysis with a random-effects model demonstrated a significant reduction of intrauterine adhesions when polyethylene oxide-sodium carboxymethylcellulose was used as the primary preventative method in 2 studies (relative risk, 0.26, 95% confidence interval, 0.09–0.76). Minimal heterogeneity was suggested by the result of the Q test (Q = 0.1, P = .89) and the I 2 index (I 2 value = 0%, 95% confidence interval, 0–100%).
Both studies reported the incidence of moderate to severe formation of intrauterine adhesions but did not report adhesion scores. Di Spiezio Sardo et al reported a significant reduction in the severity of postoperative intrauterine adhesions with the treatment group, with only 2% having moderate to severe adhesions compared with 20% in the control group ( P < .001). However, Fuchs et al found no significant difference between their treatment group with 4% and the control group with 14% ( P = .80).
Fuchs et al reported a 14% pregnancy rate in the control group and 27% in the treatment group ( P = .66) over a 20 month follow-up period ( Table 2 ). Miscarriage rates were not reported in either study and Di Spiezio Sardo et al did not report pregnancy rates.
| Study | Therapy type | Control, n, % pregnancy | Treatment n % pregnancy | P value | Miscarriage % control vs. treatment | P value | ||
|---|---|---|---|---|---|---|---|---|
| Amer et al, 2010 | Intrauterine balloon vs plus fresh amnion graft vs plus dry amnion graft | 15 | 14.3% | Fresh amnion, 15 dry amnion, 5 | 28.6% 26.7% | .95 | — | — |
| Fuchs et al, 20134 10 | Oxiplex/AP gel | 26 | 14.0% | 26 | 27.0% | .66 | — | — |
| Pabuccu et al, 1997 | Intrauterine device | 35 | 30.0% | 36 | 47.2% | .22 | — | — |
| Roy et al, 2014 | Estradiol valerate | 45 | 40.5% | 45 | 36.6% | .82 | 18.7% vs. 14.2% | .82 |
| Tonguc et al, 2010 | Estrogen therapy Intrauterine device | 25 | 47.7% | Estrogen, 16 IUD, 19 Estrogen plus IUD, 25 | 31.5% 31.6% 32.0% | .49 | 5.2% vs estrogen, 6.2% IUD, 10.5% Estrogen plus IUD, 12% | .76 |
The study demonstrating benefit of polyethylene oxide-sodium carboxymethylcellulose for adhesion prevention came from the same group at the University of Naples, who demonstrated the benefit of hyaluronic acid. The study that showed no benefit was performed by a different research group at Tel-Aviv University (Tel-Aviv, Israel). The sensitivity analysis removing the studies from the Naples group demonstrates no benefit of using polyethylene oxide-sodium carboxymethylcellulose gel for adhesion prevention.
There is a lack of reproducible evidence that polyethylene oxide-sodium carboxymethylcellulose gel may decrease the incidence and severity of postoperative intrauterine adhesions. There is no evidence that its use affects pregnancy outcomes. The data are inconsistent across 2 studies and is limited to 162 subjects. Both studies were between unclear to high risk of bias because of the lack of outcomes blinding ( Supplemental Table 1 ). There were no low-risk studies for bias stratification.
Comparison of estrogen therapy
There were 3 studies that evaluated postoperative estrogen therapy for adhesion prevention, none of which demonstrated benefit. All 3 studies evaluated patients with septum resection. Postoperative adhesion rates were consistently low across the studies, ranging from 0% to 6.9%.
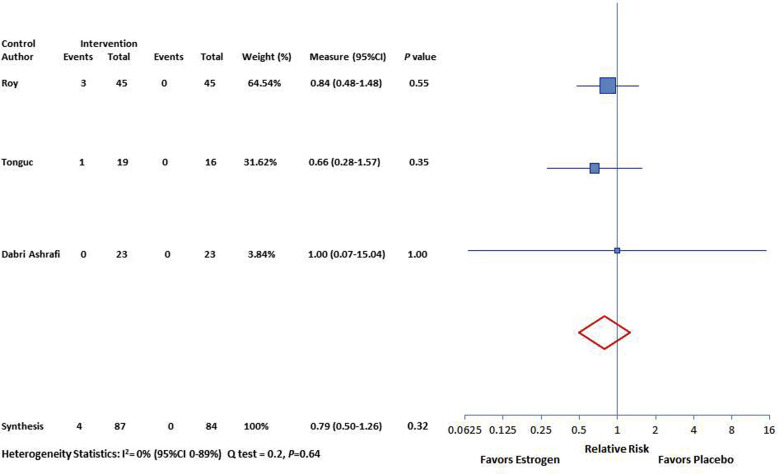
Roy et al reported postoperative intrauterine adhesions in 6.9% of patients in the control group compared with 0% in the estrogen group ( P = .24). Tonguc et al found intrauterine adhesions in 5.3% in the control group compared with 0% in the estrogen group ( P = 1.0). Dabirashrafi et al found intrauterine adhesions in 0% in both the control group and estrogen group. A meta-analysis with a fixed-effects model demonstrated no reduction of adhesions with the use of oral estrogen (relative risk, 0.78, 95% confidence interval, 0.49–1.25) ( Figure ). Minimal heterogeneity was suggested by the result of the Q test (Q = 0.2, P = .64) and the I 2 index (I 2 value = 0%, 95% confidence interval, 0–89%).
None of the estrogen treatment studies reported severity scores for postoperative adhesion formation.
Dabirashrafi et al did not report pregnancy outcomes. The other 2 studies reported no difference in postoperative pregnancy rates between the treatment and control groups ( Table 2 ). Roy et al reported pregnancy rates of 40.5% of patients in the control group compared with 36.6% in the estrogen group ( P = .82) over a 23 month follow-up period. Similarly, Tonguc et al reported pregnancy rates of 47.7% in the control group compared with 31.5% in the estrogen group ( P = .66) over a 1 month follow-up period.
A meta-analysis with a fixed-effects model demonstrated no difference in pregnancy with the use of oral estrogen (relative risk, 0.78, 95% confidence interval, 0.28–1.25) ( Supplemental Figure 2 ). Minimal heterogeneity was suggested by the result of the Q test (Q = 0.2, P = .62) and the I 2 index (I 2 value = 0%, 95% confidence interval, 0–100%).
Both studies reported no difference in postoperative miscarriage rates between the treatment and control groups. Roy et al reported miscarriage rates of 18.7% in the control group compared with 14.2% in the estrogen group ( P = .82). Similarly, Tonguc et al reported pregnancy rates of 5% in the control group compared with 6.2% in the estrogen group ( P = 1.0). A meta-analysis with a fixed-effects model demonstrated no difference in pregnancy with the use of oral estrogen (relative risk, 0.87, 95% confidence interval, 0.21–3.49). Minimal heterogeneity was suggested by the result of the Q test (Q = 0.1, P = .77) and the I 2 index (I 2 value = 0%, 95% confidence interval, 0-100%).
There is no evidence that estrogen use decreases intrauterine adhesion formation or improves subsequent pregnancy outcomes. The data are consistent across 3 individual studies but is limited to 171 subjects. The study by Tonguc et al was at low risk of bias and the other 2 studies at unclear risk of bias because of unclear allocation concealment ( Supplemental Table 1 ). Bias stratification of only the low-risk trial did not change the outcome.
Human amnion
There was 1 study that evaluated fresh and dried human amnion for the prevention of intrauterine adhesions. Amer et al evaluated patients with severe synechiae and postoperative treatment with an intrauterine balloon, fresh amnion, and dried amnion. The amnion was applied into the uterus around an intrauterine balloon. Postoperative adhesion scores were similar in the 3 groups: 2 in the intrauterine balloon group, 1.5 in the fresh amnion group, and 2 in the dried amnion group ( P = .27). Although postoperative adhesion scores were similar between the groups, the authors reported that the fresh amnion group had a great reduction in adhesion scores compared with the balloon only and the dried amnion groups. Pregnancy rates were similar in the 3 groups: 14.3% in the balloon group, 28.6 in the fresh amnion group, and 26.7% in the dried amnion group ( P = .95). The study did not report on the rate of adhesion reformation or miscarriage rates in the 3 groups.
There is no evidence that human amnion is superior to placebo for the prevention of intrauterine adhesions. There is no evidence that the use of human amnion improves pregnancy outcomes. The data are limited to a single study with 43 subjects.
Alginate carboxymethylcellulose hyaluronic acid gel and carboxymethylcellulose hyaluronic acid gel
There was 1 study that evaluated alginate carboxymethylcellulose hyaluronic acid gel and carboxymethylcellulose hyaluronic acid gel for the prevention of intrauterine adhesions. Kim et al evaluated patients with hysteroscopy for polypectomy, myomectomy, septum resection, adhesion resection, and abnormal uterine bleeding treated with alginate carboxymethylcellulose hyaluronic acid gel or carboxymethylcellulose hyaluronic acid gel. The presence of postoperative adhesions was similar in the 2 groups: alginate carboxymethylcellulose hyaluronic acid gel, 9.1%, vs carboxymethylcellulose hyaluronic acid gel, 17.9% ( P = .21). Postoperative adhesion scores were similar in the 2 groups: alginate carboxymethylcellulose hyaluronic acid gel, 2.8, v carboxymethylcellulose hyaluronic acid gel, 1.9 ( P = .21). The study did not report on pregnancy or miscarriage outcomes.
There is no evidence to support a difference between alginate carboxymethylcellulose hyaluronic acid gel and carboxymethylcellulose hyaluronic acid gel. The data are limited to a single study with 187 subjects.
Repeat hysteroscopy at 1 week
Pabuccu et al evaluated the use of an intrauterine device and guided hysteroscopy 1 week after the initial surgery in patients treated for severe synechiae. Both groups received intrauterine device placement and 2 months of estrogen and progesterone treatment. The study divided the groups in which 1 group received a hysteroscopy 1 week after the initial surgery with further lysis of new adhesions, whereas the other group did not. The repeat hysteroscopy group had a lower rate of adhesions at 2 months compared with the control group (10.9% vs 82.9%, P < .05). Pregnancy rates were similar in the repeat hysteroscopy group (47.2%) and the control group (30%) ( P = .22).
There is evidence to suggest repeat hysteroscopy at 1 week decreases intrauterine adhesion formation when combined with estrogen, progesterone, and intrauterine device use. However, there was no demonstrable effect on pregnancy outcomes. Additionally, the intervention (repeat operative hysteroscopy at 1 week) is the same ultimate intervention needed if adhesions form postoperatively. The data are limited to a single study of 71 subjects.
Intrauterine device
Tonguc et al had study arms comparing estrogen with a copper intrauterine device and an intrauterine device alone in addition to the control and estrogen-only arms already discussed. They demonstrated similar rates of postoperative intrauterine adhesions in all groups: control, 5.3%; intrauterine device, 10.5%; and intrauterine device with estrogen, 12% ( P = .50). The investigators did not evaluate the severity of the postoperative adhesions.
They also demonstrated similar pregnancy rates in the study arms: control, 47.4%; intrauterine device, 31.6%; and intrauterine device with estrogen, 32% ( P = .49). Similarly, miscarriage rates were similar in the 3 arms: control, 5.2%; intrauterine device, 10.5%; and intrauterine device with estrogen, 12% ( P = .76).
Vercellini et al also evaluated a copper intrauterine device with estrogen vs no treatment. The study of 20 women had no postoperative intrauterine adhesions in either group. The study did not report on pregnancy outcomes following the treatment. These studies were not included in the meta-analysis because of the usage of different formulations of estrogen therapy in addition to small sample sizes with no difference in the results.
There is no evidence to suggest that copper intrauterine device use prevents postoperative adhesions or improves pregnancy outcomes. The data are limited to 2 studies of only 83 subjects. The study by Tonguc et al was at low risk of bias and the study by Vercellini et al at unclear risk of bias because of unclear allocation concealment and blinding ( Supplemental Table 1 ). Bias stratification of only the low-risk trial did not change the outcome.
Results
Selection of studies for meta-analysis
Abstracts from 73 papers were reviewed, of which 19 papers were further evaluated in detail ( Supplemental Figure 1 ). There were 7 studies that were excluded after review of the full text articles: 1 study evaluated adhesions with hysterosalpingogram only in patients not pregnant 8 months postoperatively, 3 were not randomized controlled trials, 1 was a duplicate from a prior publication included in the review, 1 was published only as an abstract, and 1 study included a randomized and nonrandomized arm and evaluated presurgical danazole for adhesion prevention. Thus, 12 randomized controlled trials met inclusion criteria and were included in the systematic review. Furthermore, 8 studies compared similar preventative intrauterine adhesions methods and were included in the meta-analysis.
There was a lack of similar trials comparing the use of an intrauterine balloon, an intrauterine device, or other adhesions prevention barriers. Thus, these therapies were included in the systematic review but were not included in the meta-analysis data synthesis. There were 3 studies that evaluated hyaluronic acid gel, 3 studies that evaluated estradiol valerate, and 2 studies that evaluated polyethylene oxide-sodium carboxymethylcellulose gel.
Assessment of bias
Of all the studies, 5 failed to report on allocation concealment and may have been at risk for participation bias ( Supplemental Table 1 ). There were 8 studies that did not blind investigators to subject group assignment and may have been at risk for performance and ascertainment bias. Furthermore, 5 studies did not have complete data reporting of patient dropout or loss to follow-up.
There were 2 trials that reported their outcomes on an intent-to-treat basis, and both had no patients lost to follow-up. There were 2 studies that had a 21% patient dropout and may have been at risk for attrition bias. Fuchs et al had a similar dropout between the groups, making it unlikely that retention bias affected the results. Tonguc et al had dropout rates from 0% to 44% in the various arms of the study, placing it at risk for retention bias. The remaining studies that had complete data reporting had between 0% and 9% subject dropout. The majority of subject dropout across all studies was due to failure to follow up for a second-look hysteroscopy.
Hyaluronic acid gel
There were 3 studies that evaluated hyaluronic acid gel for adhesion prevention ( Supplemental Table 2 ). Guida et al evaluated the prevention after polypectomy, myomectomy, or septum resection; Acunzo et al evaluated the prevention after septum resection; and De Iaco et al incorporated all of these same procedures. The incidence of postoperative adhesion formation ranged from 22% to 32% in the control groups and from 10% to 18% in the treatment groups ( Table 1 ). Of these studies, 2 reported a significant reduction in the presence of intrauterine adhesions with the intrauterine application of hyaluronic acid.



