Background
Long-acting reversible contraception is more effective for pregnancy prevention than shorter-acting contraceptive methods and has the potential to reduce healthcare disparities and costs. However, long-acting reversible contraception is underused in the United States. One population of interest is beneficiaries of the United States military healthcare system who have access to universal healthcare, including no-cost, no-copay contraception with unlimited method switching, and comprise a large, actual use cohort. Efforts to increase long-acting reversible contraception initiation and continuation in this population may improve health outcomes and mitigate the profound consequences of unintended or mistimed pregnancy on readiness and cost to the military.
Objective
We aimed to determine long-acting reversible contraception initiation and continuation rates among the diverse population with universal healthcare who are enrolled in the US military healthcare system.
Study Design
This study is a retrospective cohort of >1.7 million women, aged 14–40 years, who were enrolled in the US military healthcare system, TRICARE Prime, between October 2009 and September 2014. Individuals were assessed for long-acting reversible contraception initiation and continuation with the use of medical billing records. Method continuation and factors that were associated with early method discontinuation were evaluated with the Kaplan-Meier estimator and Cox proportional hazard models.
Results
During the study dates, 188,533 women initiated long-acting reversible contraception. Of these, 74.6% women selected intrauterine contraceptives. Method initiation rates remained relatively stable (41.7–50.1/1000 women/year) for intrauterine methods, although the rate for subdermal implants increased from 6.1–23.0/1000 women/year. In analysis of women who selected intrauterine contraceptives, 61.2% continued their method at 36 months, and 48.8% continued at 60 months. Among women who selected the implant, 32.0% continued their method at 36 months; however, 45.8% continued until 33 months (ie, 3 months before the currently recommended expiration date). Compared with intrauterine contraceptive users, implant users were more likely to discontinue their method during the 36 months after insertion (hazard ratio, 1.59; 95% confidence interval, 1.56–1.62; P < .001). Adolescents aged 14-19 years were the least likely age group to discontinue the implant before 36 months; women aged 35-40 years were the least likely to discontinue an intrauterine contraceptive before 60 months. In multivariable analysis that controlled for demographic factors and contraceptive type, early contraceptive method discontinuation was most likely among women aged 20-24 years, implant users, and women with method initiation in military clinics.
Conclusion
In the US military healthcare system, TRICARE Prime, the initiation of long-acting reversible contraception is low but increasing, and continuation rates are high. This evidence supports long-acting reversible contraception as first-line recommendations for women of all ages who seek contraception.
Forty-five percent of pregnancies in the United States are unintended; of these, 42% will result in elective termination. Unintended pregnancy is associated with adverse health outcomes for mother and child and lower socioeconomic and educational achievement. In recent years, major medical societies and the Centers for Disease Control and Prevention have endorsed the provision of long-acting reversible contraception (LARC) as potential means to safely and effectively prevent unplanned pregnancies, reduce healthcare disparities, and control costs for women of reproductive age.
LARC methods, which include the levonorgestrel-releasing intrauterine system (LNG-IUS), the copper-containing intrauterine device (Cu-IUD), and the etonogestrel-releasing implant (implant), offer advantages over other reversible contraceptive methods because of their superior efficacy. Moreover, in a recent analysis of 4708 participants in the prospective cohort study The Contraceptive CHOICE Project (CHOICE), the 36-month continuation rate of LARC was 67% compared with 31% using non–LARC hormonal methods. Despite the high efficacy and reliability of these methods, LARC options account for approximately 12% of the contraceptives used by women aged 15–44 years in the United States. Recent prospective data suggest that easily accessible and affordable LARC can reduce rates of abortion, unintended pregnancy (including teenage pregnancy), and healthcare-associated costs.
LARC generally is continued by at least 80% of users by 12 months; however, data in the United States regarding current LARC methods are limited beyond this duration. By 3 years, in combination with international data, intrauterine contraceptives appear to be continued by 49–80% of users and the implant by 30–56% of users. At 5 years, intrauterine contraceptives appear to be continued by 33–55% of users. The wide ranges may be due to significant differences in study methods and sample populations.
The extent to which members of the US military, military retirees, and their family members initiate and continue LARC is largely unknown. Approximately 350,000 women of reproductive age currently serve in the US military’s active duty or selected reserve force, and 1 million others have a parent or spouse currently serving in one of these capacities. These women have access to universal healthcare, including no-cost contraception with unlimited method switching. Despite these advantages, >7 unintended pregnancies a year occur for every 100 active-duty service women, and more than one-half of all pregnancies among active-duty service women are unintended. These unintended pregnancies have a physical and emotional impact on both the mother and infant and degrade military readiness. Efforts to increase LARC initiation may improve health outcomes for this population and mitigate the profound consequences on readiness and cost to the military.
Previous studies on long-term continuation of LARC are limited in that they entailed regional sampling, random assignment of participants into contraceptive method types, or continuation rates of ≤1 year. This study was designed to avoid these limitations and provide additional evidence on long-term continuation of LARC. The primary objectives of this study were to (1) determine initiation and long-term continuation rates of LARC in a large, diverse population with universal healthcare and (2) understand LARC usage patterns in the US military healthcare system.
Materials and Methods
This study is a retrospective cohort of >1.7 million women, ages 14–40 years, who were enrolled in the military healthcare insurance program, TRICARE Prime, between October 1, 2009 and September 30, 2014. TRICARE Prime covers medical care that is provided at military treatment facilities or contracted through civilian providers for all active-duty service members, military retirees under the age of 65 years, and members of the national guard and reserve who have been called up to active duty. Family members of these individuals, which include spouses and dependent children under the age of 26 years, are also eligible for care in this healthcare plan. We used the Military Health System Management Analysis and Reporting Tool (M2) to review medical and pharmacy billing records of enrolled women during the study time period. Records were entered into this data repository monthly and reflect enrollment status and healthcare use during the previous month. Billing records from military clinics were drawn directly from the military’s electronic medical record; information from civilian network clinics and pharmacies was collected from billing statements. The institutional review board of Brooke Army Medical Center, Fort Sam Houston, Texas, approved this study.
The primary outcome of interest was time from insertion to discontinuation of individual LARC methods, which included the Cu-IUD, the 52-mg LNG-IUS, and the implant. Of note, the 13.5-mg, 3-year LNG-IUS was approved for use in 2013 and was used infrequently in military treatment facilities in 2014; therefore, cases were not distinguished from the 52 mg model and were excluded from analysis of continuation beyond 36 months.
Records were assessed for initiation and discontinuation of LARC methods using Current Procedural Terminology (CPT) codes. We identified episodes of LARC insertion using the following CPT codes: 11981, 11983, 11975, and 11977 for the implant, and 58300 insertion of an intrauterine contraceptive. Episodes of LARC discontinuation were identified by the use of CPT codes 11976, 11982, or 58301. We attempted to identify the specific type of intrauterine contraceptive inserted using pharmacy records and associated Healthcare Common Procedure Codes (J7300, J7302, and S4981). If we were unable to determine the specific intrauterine method used (LNG-IUS or Cu-IUD), the type was noted as “unknown.”
Only the first instance of a CPT insertion code was captured per participant. Women who had subsequent CPT codes that documented a removal and insertion of the same LARC method during that month were counted as a method continuation. Women who had CPT code 11983, which documented implant removal and replacement and appeared as the first episode of LARC insertion during the study period, were counted as a first insertion. Subsequent occurrences of this or another implant insertion code after an initial episode of implant insertion were counted as a method continuation.
LARC continuation rates were assessed by Kaplan-Meier analysis, which measured the time in months between initiation and discontinuation. Participants were followed until they reached 1 of 3 endpoints: method discontinuation, disenrollment from TRICARE Prime, or the end of the study period. Continuation rates were calculated over the first 36 months for all methods and over the first 60 months for intrauterine contraceptives, and were further characterized by examination of demographic characteristics at the time of insertion, which included age, military duty status, type of clinic where the method was inserted, and method type. The 36- and 60-month analyses represents the Federal Drug Administration’s approved duration of use for the implant and the 52-mg LNG-IUS, respectively. In addition, both study durations allow for comparisons with previously established benchmarks for method continuation.
Statistical analyses were conducted with SPSS software (version 22; IBM Corporation, Armonk, NY). Descriptive statistics were used for demographic characteristics at the time of LARC initiation: age (14–19, 20–24, 25–29, 30–34, and 35–40 years), eligibility status (service members vs family members and retirees), and clinic type used. The chi-square test and independent samples t -tests were used to assess the relationship between the subject demographics and LARC type selected. The Kaplan-Meier estimator was used to estimate survival duration (ie, continuation duration) of each LARC type over the study timeframe and for the different demographic groups. The generalized Wilcoxon test was used to compare the survival distributions of the different groups, including censored observations. Cox proportional hazard models were used to assess the independent association of the demographic characteristics and LARC type with early discontinuation. An alpha level of .05 was set for all comparisons.
Results
On average, there were 887,646 (standard deviation [SD]=23,006) enrolled women in our inclusive age range per month; the average length of TRICARE enrollment was 36.1 months. Our analytic sample consisted of 188,533 initiators of LARC, which included 140,553 women who initiated intrauterine contraceptives and 47,980 women who initiated a subdermal implant. Women were followed for an average of 14.7 (SD = 13.8) months after LARC insertion before achieving one of the study endpoints (range, 1–60 months). At the time of LARC initiation, the average age of the women in our sample was 25.9 (SD = 5.5) years; 75.8% were family members, and 31.8% had the insertion at a civilian network clinics ( Table 1 ).
| Demographic group | Total (n = 188,533), n (%) | Intrauterine contraceptive (n = 140,553), n (%) | Etonogestrel implant (n = 47,980), n (%) | P value |
|---|---|---|---|---|
| Age group, y | <.001 | |||
| 14–19 | 18,371 (9.7%) | 7,690 (5.5%) | 10,681 (22.3%) | |
| 20–24 | 69,007 (36.6%) | 46,418 (33.0%) | 22,589 (47.1%) | |
| 25–29 | 54,337 (28.8%) | 44,346 (31.6%) | 9,991 (20.8%) | |
| 30–34 | 30,042 (15.9%) | 26,635 (19.0%) | 3,407 (7.1%) | |
| 35–40 | 16,776 (8.9%) | 15,464 (11.0%) | 1,312 (2.7%) | |
| Military duty status | <.001 | |||
| Servicewomen on active duty | 45,695 (24.2%) | 30,334 (21.6%) | 15,361 (32.0%) | |
| Family members and retirees | 142,774 (75.8%) | 11,0157 (78.4%) | 32,617 (68.0%) | |
| Clinic type | <.001 | |||
| Military clinic | 128,522 (68.2%) | 90,342 (64.3%) | 38,180 (79.6%) | |
| Civilian Network clinic | 59,999 (31.8%) | 50,199 (35.7%) | 9,800 (20.4%) | |
| Contraceptive type | ||||
| Levonorgestrel intrauterine system | 51,470 (36.6%) | |||
| Copper intrauterine device | 5,983 (4.3%) | |||
| Unknown | 83,100 (59.1%) |
Of all women who initiated LARC, 74.6% selected intrauterine contraceptives. Among women seen in military clinics for intrauterine contraception, 56.1% definitively initiated the LNG-IUS, and 6.5% initiated the Cu-IUD. We generally were unable to categorize the intrauterine contraceptive type among individuals who received insertions in network clinics. The implant was initiated in 25.4% of women. Intrauterine contraceptive users were significantly older than implant users (26.9 years old [SD = 5.4] vs 23.0 [SD = 4.7]; P < .001). Family members of military service members were more likely than servicewomen on active duty to select intrauterine contraceptives. Furthermore, women who were seen for LARC placement in civilian network clinics were more likely than those who were seen in military clinics to select intrauterine contraceptives ( Table 1 ).
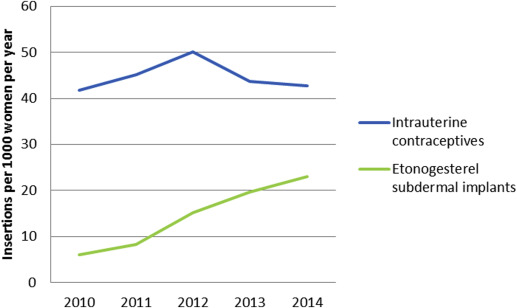
The intrauterine contraception insertion rate remained relatively stable during the study interval, with a range of 41.7–50.1 insertions per 1000 enrolled women per year; the implant insertion rate increased from 6.1 insertions per 1000 women per year in 2010 to 23.0 insertions per 1000 women per year in 2014 ( Figure 1 ).
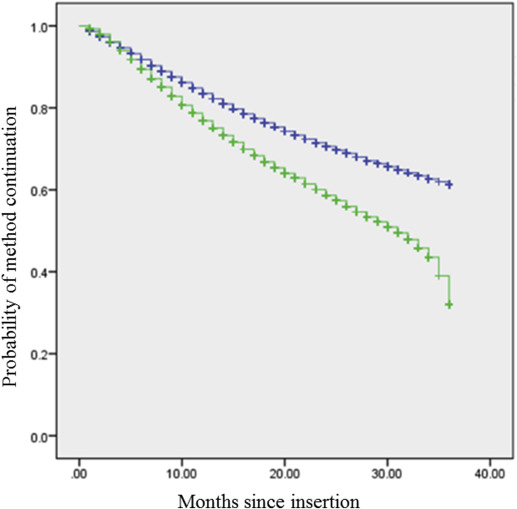
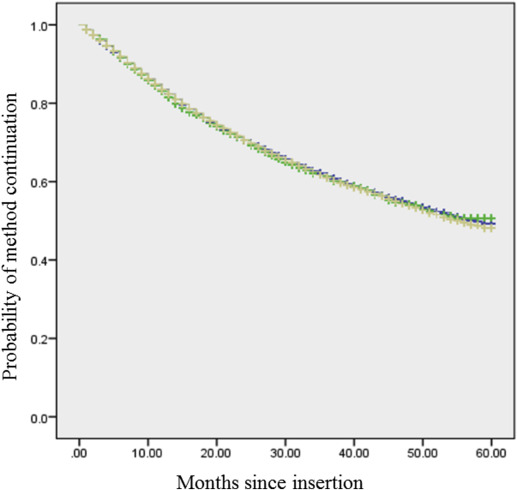
Implant continuation rates were 76.8% at 12 months, 58.6% at 24 months, 45.8% at 33 months, and 32.0% at 36 months ( Figure 2 ; Table 2 ). Intrauterine contraceptive continuation rates were 83.5% at 12 months, 70.6% at 24 months, 61.2% at 36 months, 54.1% at 48 months, and 48.8% at 60 months ( Figure 2 ; Table 2 ). Continuation rates of intrauterine contraception did not differ by device type (excluding unknown types [ P = .461]; including unknown types, [ P = .644]; Figure 3 ). Overall, the implant was more likely than intrauterine contraceptives to be discontinued at <36 months (hazard ratio, 1.59; 95% confidence interval, 1.56–1.62; P < .001; Figure 2 ).
| Method | Months a | |||||
|---|---|---|---|---|---|---|
| 12 | 24 | 33 | 36 | 48 | 60 | |
| Intrauterine contraceptive | 83.5 (83.3–83.7) | 70.6 (70.2–71.0) | 63.4 (63.0–63.8) | 61.2 (60.8–61.6) | 54.1 (53.5–54.6) | 48.8 (48.0–49.6) |
| Etonogestrel implant | 76.8 (76.4–77.2) | 58.6 (57.8–59.4) | 45.8 (44.8–46.8) | 32.0 (31.0–33.0) | ||
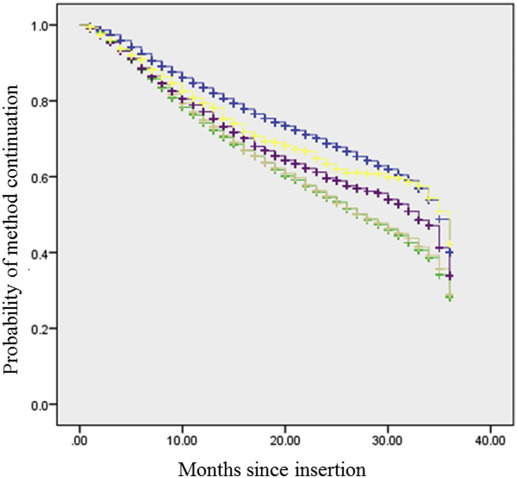
In a univariable analysis that was stratified by contraceptive type, adolescents had the highest implant continuation rates over the first 36 months ( P < .001), whereas 35- to 40-year-old women had the highest intrauterine contraceptive continuation rates of any age group ( Figures 4 and 5 ; Table 3 ). In multivariable analyses that controlled for demographic factors and contraceptive type, the likelihood of early LARC discontinuation was highest among women who were 20–24 years old at the time of insertion, who were seen in a military clinic rather than a network clinic for method insertion, and who selected an implant for contraception rather than an intrauterine contraceptive ( Table 4 ).