Inflammatory Bowel Disease
Robert Wyllie
Inflammatory bowel disease (IBD) is a general term referring to two chronic conditions of the gastrointestinal tract: Crohn disease (CD) and ulcerative colitis (UC). Although the clinical spectrum of symptoms may be similar in both diseases, the clinical differentiation of CD from UC has important therapeutic implications.
EPIDEMIOLOGY OF INFLAMMATORY BOWEL DISEASE
Forty-five hundred children are diagnosed with IBD every year, and there are approximately 1 million people in the United States who have either CD or UC. The peak incidence is between 15 and 25 years of age, and 25% of the newly diagnosed cases occur in the childhood and adolescent age group. In the pediatric age group CD is more common than UC, accounting for 60% versus 20% to 30%. Approximately 10% to 20% of the children diagnosed with IBD can not definitively be classified as having CD or UC and are placed in a category called Indeterminate Colitis.
CROHN DISEASE
CD may involve any portion of the gastrointestinal tract from the mouth to the anus, but it most often affects the terminal ileum. The terminal ileum and colon are involved in approximately 50% of patients, and 40% have isolated small bowel disease. In patients with small bowel disease, the inflammation is localized in the terminal ileum in 50%, and 50% have multifocal involvement of the small bowel. In 10% of patients, disease is isolated to the large bowel, with no involvement of the small bowel. The inflammation is usually patchy, and ulcerations are interspersed with normal mucosa. Grossly, the bowel wall is thickened by chronic inflammation and edema; as a result, the bowel lumen may be narrowed and adjacent loops of bowel may be displaced. The mesentery may be thickened and edematous. Fat migrates over the serosal surface of the bowel, creating a characteristic appearance of “fat wrapping.” Microscopically, the diagnostic lesion is a granuloma, but granulomas can be identified in only 25% of the mucosal endoscopic biopsy specimens of the large bowel and only 40% of surgically resected specimens. Endoscopically, the appearance of the mucosa may be one of superficial ulcerations overlying lymphoid follicles or of large, linear (“bear claw”) ulcers. A cobblestone appearance may result when linear ulcerations isolate blocks of regenerating mucosa.
The initial inflammatory lesion typically evolves into stricturing (fibrostenotic) or penetrating (fistulizing) disease. Fistulae arise when transmural inflammation erodes into adjacent structures. The most common site of fistula formation is an adjacent loop of bowel, but fistulae may occur anywhere, including the perineum, abdominal wall, bladder, or vagina. An ulcer may also erode the bowel wall and end blindly in a localized inflammatory mass, or phlegmon. Stricturing disease occurs when circumferential inflammation results, and fibrosis restricts the size of the intestinal lumen and limits the flow of contents through the intestine.
A general increase in incidence was documented between 1950 and 2000. In approximately 60% pediatric patients with CD, the diagnosis is made between the ages of 16 and 20 years, and in 30% between 11 and 15 years. Only 10% of patients present between 6 and 10 years of age. CD is more common in the white and Jewish populations. Girls are 20% more likely to develop CD than boys. The frequency of CD is higher in certain disorders, including:
Turner syndrome
Glycogen storage disease type 1B
Cystic fibrosis
Pachydermoperiostosis
Hermansky-Pudlak syndrome
ULCERATIVE COLITIS
The inflammation of UC is limited to the large bowel. Classically, the inflammation is continuous from the distal to the proximal bowel. At the time of the initial diagnosis in children, approximately two thirds have disease involving the total colon. Disease is limited to the rectum in 15%, and to the left side of the colon in 25%. Occasionally in children, the rectum is spared at the time of the initial diagnosis, but continuous inflammation usually develops during the course of the disease. Of the children who initially have left-sided inflammation or inflammation limited to the rectum, 75% progress to total colonic disease within 10 years.
The endoscopic changes in UC consist of mucosal erythema and edema that produce a granular appearance. In severe disease, deep ulceration and sloughing of the mucosa may be seen. The typical histologic findings are uninterrupted inflammation of the crypts with crypt abscesses and chronic inflammatory cells.
The onset of symptoms is typically between the ages of 16 and 20 years, with symptoms developing in approximately one third of children between the ages of 11 and 15 years. Symptoms appear within the first decade of life in approximately 10% of cases, but UC is uncommon before the age of 6 years.
The epidemiology of UC is similar to that of CD. UC is more common in whites than in individuals of color and is identified more often in the Jewish population. Boys are slightly more likely to develop UC than girls. IBD is more common in the northern United States, and the incidence is higher in urban areas than in rural settings.
ETIOLOGIC CONSIDERATIONS
A variety of studies have investigated the relationship of IBD to nutritional, infectious, and psychologic abnormalities. The incidence of CD is higher in persons with diets high in sugar and lower in those with a higher intake of fluids, fruits, vitamin C, and magnesium. Diets rich in vegetables and potassium also have been associated with a lower risk for development of the disease. Smoking increases the relative risk for CD and decreases the risk for UC. A variety of infectious organisms have been implicated in the pathophysiology of IBD. Measles infection early in life has been associated with a higher risk for CD. Investigation into the possible role of Mycobacterium paratuberculosis has yielded conflicting results, but more recent DNA hybridization studies suggest it is not associated with the development of IBD. Abnormalities in intestinal mucus have been demonstrated to enhance the inflammatory process and are associated with IBD. No specific emotional factors have been associated with the development of IBD. A genetic predisposition to IBD is suggested by a predisposition to the development of IBD in certain ethnic groups and an increased incidence among the family members of initially identified persons. Twin studies demonstrate a high concordance rate for CD among monozygotic twins, approximately 40%, and a concordance rate among dizygotic twins of 10%. Less dramatic increases in concordance rates are seen in UC (10% for monozygotic twins and 3% for dizygotic twins). The incidence of both CD and UC is increased in the first-degree and more distant relatives of initially identified persons. Overall, 10% to 20% of patients with IBD report having a relative with IBD. After an index case has been identified, the likelihood that CD will develop in a sibling is 5% to 10% over a lifetime. The lifetime risk that CD will develop in the offspring of a parent with CD is similar, approximately 10%. In families in which both parents have CD, the risk may be as high as 50%. Familial statistics for UC tend to follow the same patterns but with less dramatic associations. Overall, IBD is found five to ten times more frequently in the relatives of individuals with CD or UC than in control families. In families with IBD, disease is generally diagnosed at a younger age, tends to involve the small bowel, and Jewish ethnicity is relatively common. The lack of an increased risk in adopted siblings and spouses makes an environmental influence unlikely.
NOD2/CARD15 mutations have been identified and associated with CD. Three variations of the gene were found to be associated with CD but not UC. The pathophysiology of how mutations in the NOD2 gene suggest the mutations are associated with a decreased ability of the immune system to respond to bacterial products suggesting CD may be related to a defective host response to normal intestinal flora. Recently genome wide association studies have identified several other areas that also are related to the development of IBD. Defects in the IL23R gene region have been associated with both UC and CD.
SYMPTOMS
The various presenting features of CD and UC are listed in Table 5.1. Rectal bleeding is more common in UC, whereas
weight loss and growth failure are more common in CD. The typical presentation of UC is bloody diarrhea. Occasional patients in whom inflammation is limited to the rectum may present with formed stools that are coated with blood and mucus. Most children also have cramping abdominal pain that is relieved by the passage of stool. Bowel movements are typically more frequent in the mornings, when patients may experience rectal spasm associated with muscular irritability. The muscular spasm creates the sensation that stool is within the rectal vault, and patients may be in and out of the bathroom until the spasm subsides.
weight loss and growth failure are more common in CD. The typical presentation of UC is bloody diarrhea. Occasional patients in whom inflammation is limited to the rectum may present with formed stools that are coated with blood and mucus. Most children also have cramping abdominal pain that is relieved by the passage of stool. Bowel movements are typically more frequent in the mornings, when patients may experience rectal spasm associated with muscular irritability. The muscular spasm creates the sensation that stool is within the rectal vault, and patients may be in and out of the bathroom until the spasm subsides.
TABLE 5.1 PRESENTING FEATURES OF CROHN DISEASE AND ULCERATIVE COLITIS IN CHILDHOOD | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Children with CD most often have abdominal pain in the right lower quadrant secondary to ileal inflammation. The pain is not necessarily associated with meals or defecation. If the upper gastrointestinal tract (gastroduodenal region) is involved, they may experience epigastric pain simulating that associated with peptic ulcer disease. Diarrhea occurs in approximately half of the patients with CD. Blood is more likely to be present in the stools of patients with disease of the distal colon. Many children with CD have oral aphthous ulcers. They usually persist for a longer period than lesions associated with viral inflammation. Perianal inflammation is present in 25% or more of children with CD. The most common findings are rectal fissures and surrounding tags. The finding of significant perianal disease or inflammation of the small bowel distinguishes CD from UC.
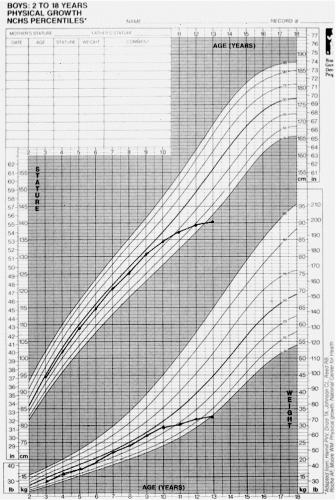
Growth failure is a hallmark of CD, although it may also occur in UC. Typically, serial measurements of growth demonstrate weight and height decreases that may precede other signs and symptoms of disease (Fig. 5.1). A deceleration in growth velocity is seen in up to 90% of patients. Growth failure is secondary to inadequate caloric intake in most children. Fever is more common in CD than in UC. It is usually of low grade and may occasionally occur without other gastrointestinal symptoms. Arthritis is more common in CD than in UC and may precede the development of bowel symptoms by months or years (see Table 5.1). A typical form of joint involvement is a unilateral migratory arthritis of the large joints of the lower extremities. The joints may be erythematous or swollen, but the arthritis is not usually associated with joint destruction. Joint
inflammation usually parallels the activity of the underlying bowel disease. Ankylosing spondylitis occurs in 2% to 6% of patients with IBD and is independent of the bowel disease. Clubbing is typically found in CD and is the result of hypertrophic osteoarthropathy.
inflammation usually parallels the activity of the underlying bowel disease. Ankylosing spondylitis occurs in 2% to 6% of patients with IBD and is independent of the bowel disease. Clubbing is typically found in CD and is the result of hypertrophic osteoarthropathy.
The most common cutaneous manifestations are erythema nodosum and pyoderma gangrenosum, which occur in 1% to 4% of patients with IBD (Table 5.2). Other, less common skin conditions include polyarteritis nodosa and epidermolysis bullosa. Ocular complications are uncommon, occurring in fewer than 10% of patients. Episcleritis produces painless red eyes with no changes in vision. Iritis and uveitis are typically painful and may affect vision. Subcapsular cataracts are typically associated with the use of corticosteroids.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree