Table 40–2. Diagnostic tests for viral infections.
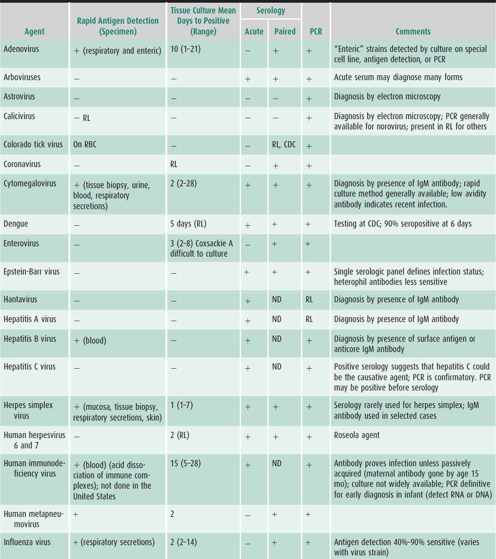
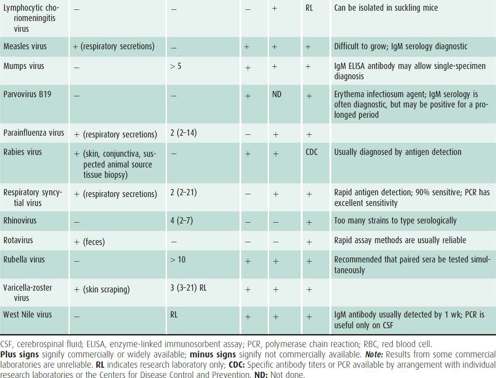
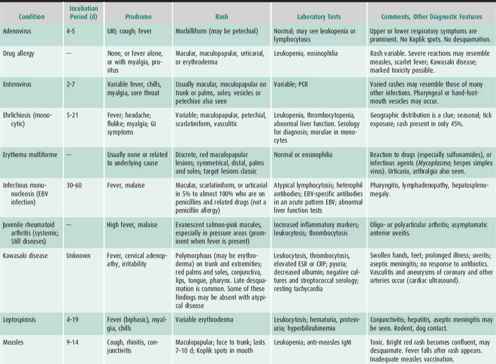
Table 40–3. Some red rashes in children.

RESPIRATORY INFECTIONS
Many viral infections can cause either upper or lower respiratory tract signs and symptoms, sometimes both in the same patient. Those that produce a predominance of these signs and symptoms are described in the text that follows. Many so-called respiratory viruses can also produce distinct nonrespiratory disease (eg, enteritis or cystitis or myocarditis caused by adenoviruses; parotitis caused by parainfluenza viruses). Respiratory viruses can cause disease in any area of the respiratory tree. Thus, they can cause coryza, pharyngitis, sinusitis, tracheitis, bronchitis, bronchiolitis, and pneumonia—although certain viruses tend to be closely associated with one anatomic area (eg, parainfluenza with croup, respiratory syncytial virus [RSV] with bronchiolitis) or discrete epidemics (eg, influenza, RSV, parainfluenza). Thus it is impossible on clinical grounds to be certain of the specific viral cause of an infection in a given child. This information, which is provided by the virology laboratory, is often important for epidemiologic, therapeutic, and preventive reasons. In immunocompromised patients these annoying, but otherwise benign, viruses can cause severe pneumonia.
VIRUSES CAUSING THE COMMON COLD
The common cold syndrome (also called upper respiratory infection) is characterized by combinations of runny nose, nasal congestion, sore throat, tearing, cough, and sneezing. Low-grade fever may be present. The causal agent is usually not sought or determined. Epidemiologic studies indicate that rhinoviruses, which are the most common cause (30%–40%; much more in some series), are present throughout the year, but are more prevalent in the colder months in temperate climates. Adenoviruses also cause colds in all seasons and epidemics are common. Respiratory syncytial virus, parainfluenza viruses, human metapneumovirus, and influenza viruses cause the cold syndrome during epidemics from late fall through winter. Multiple strains of coronaviruses account for 5%–10% of colds in winter. Equally prevalent in aggregate are other newly identified respiratory viruses such as the human bocavirus (a parvovirus) and several polyomaviruses. The precise role of these newly discovered viruses in childhood disease is under study. Enteroviruses cause the “summer cold.” One outcome of the common cold is morbidity continuing for 5–7 days. It is also likely that changes in respiratory epithelium, local mucosal swelling, and altered local immunity are sometimes the precursors of more severe illnesses such as otitis media, pneumonia, and sinusitis. During and following a cold, the bacterial flora changes and bacteria are found in normally sterile areas of the upper airway. Asthma attacks are frequently provoked by any of the viruses that cause the common cold. These “cold viruses” are a common cause of lower respiratory tract infection in young children. There is no evidence that antibiotics will prevent complications of the common cold, and the unjustified widespread use of antibiotics for cold symptoms has contributed to the emergence of antibiotic-resistant respiratory flora.
In 5%–10% of children, symptoms from these virus infections persist for more than 10 days. This overlap with the symptoms of bacterial sinusitis presents a difficult problem for clinicians, especially because colds can produce an abnormal computed tomography (CT) scan of the sinuses. Viruses that cause a minor illness in immunocompetent children, such as rhinoviruses, influenza, RSV, and metapneumovirus, can cause severe lower respiratory disease in immunologically or anatomically compromised children.
There is conflicting evidence that symptomatic relief for children can be achieved with oral antihistamines, decongestants, or cough suppressants. The FDA has recommended that such over-the-counter medications not be used in children less than 2 years old. Topical decongestants provide temporary improvement in nasal symptoms. Vitamin C has not been shown to have a significant preventative or therapeutic role. Zinc therapy of the common cold and prevention with zinc may be effective in adults, but there is great uncertainty about dosing and some adverse effects. Humidified air and garlic do not alter the course of colds.
De Sutter AI et al: Oral antihistamine-decongestant-analgesic combinations for the common cold. Cochrane Database Syst Rev 2012;2:CD004976 [PMID: 22336807].
Greenber SB: Update on rhinovirus and coronavirus infections. Sem Resp Crit Care Med 2011;32(4):433 [PMID: 21858748].
Olenec JP et al: Weekly monitoring of children with asthma for infections and illness during common cold seasons. J Allergy Clin Immunol 2010;125(5):1001 [PMID: 20392488].
Singh M, Das RR: Zinc for the common cold. Cochrane Database Syst Rev 2011;2:CD001364 [PMID: 21328251].
Techasaensiri B et al: Viral coinfections in children with invasive pneumococcal disease. Ped Infect Dis J 2010;29:2010 [PMID: 20051928].
Wylie KM et al: Sequence analysis of the human virome in febrile and afebrile children. PLoS ONE 2012;7(6):e27735 [PMID: 22719819].
INFECTIONS DUE TO ADENOVIRUSES
There are 57 types of adenoviruses, which account for 5%–15% of all respiratory illnesses in childhood, usually pharyngitis or tracheitis, but including 5% of childhood lower respiratory tract infections. Adenoviral infections, which are common early in life (most prior to age 2 years), occur 3–10 days after exposure to respiratory droplets or fomites. Enteric adenoviruses are an important cause of childhood diarrhea. Epidemic respiratory disease from adenoviruses occurs in winter and spring, especially in closed environments such as day care centers and institutions. Because of latent infection in lymphoid tissue, asymptomatic shedding from the respiratory or intestinal tract is common.
Specific Adenoviral Syndromes
A. Pharyngitis
Pharyngitis is the most common adenoviral disease, and the most common viral cause of severe pharyngitis in children. Fever and adenopathy are common. Tonsillitis may be exudative. Rhinitis and an influenza-like systemic illness may be present. Laryngotracheitis or bronchitis may accompany pharyngitis.
B. Pharyngoconjunctival Fever
Conjunctivitis may occur alone and be prolonged, but most often is associated with preauricular adenopathy, fever, pharyngitis, and cervical adenopathy. Foreign body sensation in the eye and other symptoms last less than a week. Lower respiratory symptoms are uncommon.
C. Epidemic Keratoconjunctivitis
Symptoms are severe conjunctivitis with punctate keratitis and occasionally visual impairment. A foreign body sensation, photophobia, and swelling of conjunctiva and eyelids are characteristic. Preauricular adenopathy and subconjunctival hemorrhage are common.
D. Pneumonia
Severe pneumonia may occur at all ages. It is especially common in young children (age < 3 years). Chest radiographs show bilateral peribronchial and patchy ground-glass interstitial infiltrates in the lower lobes. Symptoms persist for 2–4 weeks. Adenoviral pneumonia can be necrotizing and cause permanent lung damage, especially bronchiectasis. A pertussis-like syndrome with typical cough and lymphocytosis can occur with lower respiratory tract infection. A new variant of adenovirus serotype 14 can cause unusually severe, sometimes fatal pneumonia in children and adults.
E. Rash
A diffuse morbilliform (rarely petechial) rash resembling measles, rubella, or roseola may be present. Koplik spots are absent.
F. Diarrhea
Enteric adenoviruses (types 40 and 41) cause 3%–5% of cases of short-lived diarrhea in afebrile children, especially in those less than 4 years old.
G. Mesenteric Lymphadenitis
Fever and abdominal pain may mimic appendicitis. Pharyngitis is often associated. Adenovirus-induced adenopathy may be a factor in appendicitis and intussusception.
H. Other Syndromes
Immunosuppressed patients, including neonates, may develop severe or fatal pulmonary or gastrointestinal infections or multisystem disease. Hemorrhagic cystitis can be a serious problem in immunocompromised children. Other rare complications that can occur in the immune competent child include encephalitis, hepatitis, and myocarditis. Adenoviruses have been implicated in the syndrome of idiopathic myocardiopathy.
 Laboratory & Diagnostic Studies
Laboratory & Diagnostic Studies
Diagnosis can be made by conventional culture of conjunctival, respiratory, or stool specimens, but several days to weeks are required. Viral culture using the rapid culture technique with immunodiagnostic reagents detects adenovirus in 48 hours. Adenovirus infection can also be diagnosed using these reagents directly on respiratory secretions. This is quicker, but less sensitive, than the culture methods. PCR is an important, relatively rapid and sensitive diagnostic method for adenovirus infections. Special cells are needed to isolate enteric adenoviruses. ELISA tests rapidly detect enteric adenoviruses in diarrheal specimens. Respiratory adenovirus infections can be detected retrospectively by comparing acute and convalescent sera, but this is not helpful during an acute illness.
 Treatment
Treatment
There is no specific treatment for adenovirus infections. Intravenous immuno globulin (IVIG) may be tried in immunocompromised patients with severe pneumonia. There are anecdotal reports of successful treatment of immunocompromised patients with cidofovir, which inhibits adenovirus in vitro.
Lynch JP III, Fishbein M, Echavarria M: Adenovirus. Sem Resp Critical Care Med 2011;32(4):494 [PMID: 21859752].
Pavia AT: Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis 2011;52(Suppl 4):S284 [PMID: 21460286].
Tebruegge M, Curtis N: Adenovirus: an overview for pediatric infectious diseases specialists. Ped Infect Dis J 2012;31(6):626 [PMID: 22592487].
INFLUENZA
Symptomatic infections are common in children because they lack immunologic experience with influenza viruses. Infection rates in children are greater than in adults and are instrumental in initiating community outbreaks. Epidemics occur in fall and winter. Three main types of influenza viruses (A/H1N1, A/H3N2, B) cause most human epidemics, with antigenic drift ensuring a supply of susceptible hosts of all ages. In recent years, avian influenza A/H5N1 has caused isolated human outbreaks in Asia that are associated with high rates of hospitalization and death. A swine-origin influenza A/H1N1 initiated a human pandemic in the spring of 2009. Almost 50 million Americans were infected with this virus in 2009. Illnesses caused by this virus tend to be more severe in older children and young adults. In addition, the rates of hospitalization and death are higher than typically observed with seasonal influenza.
 Clinical Findings
Clinical Findings
Spread of influenza occurs by way of airborne respiratory secretions. The incubation period is 2–7 days.
A. Symptoms and Signs
Influenza infection in older children and adults produces a characteristic syndrome of sudden onset of high fever, severe myalgia, headache, and chills. These symptoms overshadow the associated coryza, pharyngitis, and cough. Usually absent are rash, marked conjunctivitis, adenopathy, exudative pharyngitis, and dehydrating enteritis. Fever, diarrhea, vomiting, and abdominal pain are common in young children. Infants may develop a sepsis-like illness and apnea. Chest examination is usually unremarkable. Unusual clinical findings include croup (most severe with type A influenza), exacerbation of asthma, myositis (especially calf muscles), myocarditis, parotitis, encephalopathy (distinct from Reye syndrome), nephritis, and a transient maculopapular rash. Acute illness lasts 2–5 days. Cough and fatigue may last several weeks. Viral shedding may persist for several weeks in young children.
B. Laboratory Findings
The leukocyte count is normal to low, with variable shift. Influenza infections may be more difficult to recognize in children than in adults even during epidemics, and therefore a specific laboratory test is highly recommended. The virus can be found in respiratory secretions by direct fluorescent antibody staining of nasopharyngeal epithelial cells, ELISA, optic immunoassay (OIA), and PCR. PCR has the highest sensitivity and specificity, close to 100%, and is rapidly becoming the preferred test. It can also be cultured within 3–7 days from pharyngeal swabs or throat washings. Many laboratories use the rapid culture technique by centrifuging specimens onto cultured cell layers and detecting viral antigen after 48 hours. Other body fluids or tissues (except lung) rarely yield the virus in culture and are more appropriately tested by PCR, which, due to its high sensitivity, can increase influenza detection in respiratory specimens. A late diagnosis may be made with paired serology, using hemagglutination inhibition assays.
C. Imaging
The chest radiograph is nonspecific; it may show hyperaeration, peribronchial thickening, diffuse interstitial infiltrates, or bronchopneumonia in severe cases. Hilar nodes are not enlarged. Pleural effusion is rare in uncomplicated influenza.
 Differential Diagnosis
Differential Diagnosis
The following may be considered: all other respiratory viruses, Mycoplasma pneumoniae or Chlamydia pneumoniae (longer incubation period, prolonged illness), streptococcal pharyngitis (pharyngeal exudate or petechiae, adenitis, no cough), bacterial sepsis (petechial or purpuric rash may occur), toxic shock syndrome (rash, hypotension), and rickettsial infections (rash, different season, insect exposure). High fever, the nature of preceding or concurrent illness in family members, and the presence of influenza in the community are distinguishing features from parainfluenza or RSV infections.
 Complications & Sequelae
Complications & Sequelae
Lower respiratory tract symptoms are most common in children younger than age 5 years. Hospitalization rates are highest in children younger than 2 years. Influenza can cause croup in these children. Secondary bacterial infections (classically staphylococcal) of the middle ear, sinuses, or lungs (pneumococcal was common in the swine-origin H1N1 pandemic of 2009) are common. Of the viral infections that precede Reye syndrome, varicella and influenza (usually type B) are most notable. During an influenza outbreak, ill children who develop protracted vomiting or irrational behavior should be evaluated for Reye syndrome. Influenza can also cause viral or postviral encephalitis, with cerebral symptoms much more prominent than those of the accompanying respiratory infection. Although the myositis is usually mild and resolves promptly, severe rhabdomyolysis and renal failure have been reported.
Children with underlying cardiopulmonary, metabolic, neuromuscular, or immunosuppressive disease may develop severe viral pneumonia. During the H1N1 pandemic, new high risk conditions were described: obesity and the first 2 weeks of postpartum.
 Prevention
Prevention
The trivalent inactivated influenza vaccine is moderately protective in older children (see Chapter 10). A live attenuated influenza vaccine (FluMist) is significantly more efficacious in children and is currently recommended for immunocompetent children 2 years of age or older. It is currently recommended that all children 6 months and older, and adults should be immunized with one of the available influenza vaccines, and that two doses be administered during the first year of immunization to children less than 9 years old. There is an ongoing effort to broaden the influenza B coverage by adding an additional influenza B strain to the seasonal vaccine. Quadrivalent live attenuated and inactivated influenza vaccines have been approved by the FDA; the quadrivalent live vaccine will become available for the 2013–2014 season. Widespread resistance to adamantanes of seasonal influenza A H3N2 and pandemic influenza A H1N1/2009 has made these drugs obsolete for the treatment and prevention of influenza. For prophylaxis oseltamivir is the most widely used agent (children < 15 kg, 30 mg daily; those 15–23 kg, 45 mg daily; those 23–40 kg, 60 mg daily; and those > 40 kg, 75 mg daily). Zanamivir (10 mg daily inhalations) can also be used in children older than age 5 years. Chemoprophylaxis should be considered during an epidemic for high-risk children who cannot be immunized or who have not yet developed immunity (about 6 weeks after primary vaccination or 2 weeks after a booster dose). For outbreak prophylaxis, therapy should be maintained for 2 weeks or more and for 1 week after the last case of influenza is diagnosed.
 Treatment & Prognosis
Treatment & Prognosis
Treatment consists of general support and management of pulmonary complications, especially bacterial superinfections. Antivirals are of benefit against seasonal influenza in immunocompetent hosts if begun within 48 hours after symptom onset. Treatment duration is 5 days and the doses are twice those used for prophylaxis (see earlier). Studies in immunocompromised patients during the 2009/2010 pandemic showed that oseltamivir was useful in this population even when initiated later than 2 days after the onset of disease.
Recovery is usually complete unless severe cardiopulmonary or neurologic damage has occurred. Fatal cases occur in very young infants, immunodeficient and anatomically compromised children, pregnant women including the first 2 weeks of postpartum, and obese individuals.
Effective treatment or prophylaxis of influenza in children markedly reduces the incidence of acute otitis media and antibiotic usage during the flu season.
Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2012;61(32):613–618.
Hsu J et al: Antivirals for treatment of influenza: a systematic review and meta-analysis of observational studies. Ann Intern Med 2012;156:21–24 [PMID: 22371849].
PARAINFLUENZA (CROUP)
Parainfluenza viruses (types 1–4) are the most important cause of croup. Most infants are infected with type 3 within the first 3 years of life, often in the first year. Type 3 appears annually, with a peak in the spring or summer. Infection with types 1 and 2 is experienced gradually over the first 5 years of life, usually during outbreaks in the fall; most primary infections are symptomatic and frequently involve the lower respiratory tract. The concept that parainfluenza 4 is less pathogenic is currently being reevaluated. Its epidemiology seems to overlap with that of parainfluenza 3.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Clinical diseases include febrile upper respiratory infection (especially in older children with reexposure), laryngitis, tracheobronchitis, croup, and bronchiolitis (second most common cause after RSV). The relative incidence of these manifestations is type-specific. Parainfluenza viruses (especially type 1) cause 65% of cases of croup in young children, 25% of tracheobronchitis, and 50% of laryngitis. Croup is characterized by a barking cough, inspiratory stridor (especially when agitated), and hoarseness. Type 2 parainfluenza is more likely to cause bronchiolitis. Parainfluenza virus can cause pneumonia in infants and immunodeficient children, and causes particularly high mortality among stem cell recipients. Onset is acute. Most children are febrile. Symptoms of upper respiratory tract infection often accompany croup.
B. Laboratory Findings
Diagnosis is often based on clinical findings. These viruses can be identified by conventional or rapid culture techniques (48 hours), by direct immunofluorescence on nasopharyngeal epithelial cells in respiratory secretions (< 3 hours), or by PCR (< 24 hours).
 Differential Diagnosis
Differential Diagnosis
Parainfluenza-induced respiratory syndromes are difficult to distinguish from those caused by other respiratory viruses. Viral croup must be distinguished from epiglottitis caused by Haemophilus influenzae (abrupt onset, toxicity and high fever, drooling, dyspnea, little cough, left shift of blood smear, and a history of inadequate immunization).
 Treatment
Treatment
No specific therapy or vaccine is available. Croup management is discussed in Chapter 19. Ribavirin is active in vitro and has been used in immunocompromised children, but its efficacy is unproved.
Ruuskanen O, Lahti E, Jennings LC, Murdoch DR: Viral pneumonia. Lancet 2011;377(9773):1264 [PMID: 21435708].
RESPIRATORY SYNCYTIAL VIRUS DISEASE
 General Considerations
General Considerations
RSV is the most important cause of lower respiratory tract illness in young children, accounting for more than 70% of cases of bronchiolitis and 40% of cases of pneumonia. RSV is a ubiquitous virus of early childhood. Almost all children develop upper respiratory symptoms; of these 20%–30% will develop lower respiratory infection. Outbreaks occur annually, and attack rates are high; 60% of children are infected in the first year of life, and 90% by age 2 years. During peak season (cold weather in temperate climates), the clinical diagnosis of RSV infection in infants with bronchiolitis is as accurate as most laboratory tests. Despite the presence of serum antibody, reinfection is common. Two distinct genotypes can co-circulate or one may predominate in a community. Yearly shift in prevalence of these genotypes is a partial explanation for reinfection. However, reinfection generally causes only upper respiratory symptoms in anatomically normal children. Immunosuppressed patients may develop progressive severe pneumonia. Children with congenital heart disease with increased pulmonary blood flow, children with chronic lung disease (eg, cystic fibrosis), and premature infants younger than age 6 months (especially when they have chronic lung disease of prematurity) are also at higher risk for severe illness. No vaccine is available.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Initial symptoms are those of upper respiratory infection. Low-grade fever may be present. The classic disease is bronchiolitis, characterized by diffuse wheezing, variable fever, cough, tachypnea, difficulty feeding, and, in severe cases, cyanosis. Hyperinflation, crackles, prolonged expiration, wheezing, and retractions are present. The liver and spleen may be palpable because of lung hyperinflation, but are not enlarged. The disease usually lasts 3–7 days in previously healthy children. Fever is present for 2–4 days; it does not correlate with pulmonary symptoms and may be absent during the height of lung involvement.
Apnea, poor feeding, and lethargy may be presenting manifestations, especially in premature infants, in the first few months of life. Apnea usually resolves after a few days, often being replaced by obvious signs of bronchiolitis.
RSV infection in older children is more likely to cause tracheobronchitis or upper respiratory tract infection. Exceptions are immunocompromised children and those with severe chronic lung or heart disease, who may have especially severe or prolonged primary infections and are subject to additional attacks of severe pneumonitis.
B. Laboratory Findings
Rapid detection of RSV antigen in nasal or pulmonary secretions by fluorescent antibody staining or ELISA requires only several hours and is more than 90% sensitive and specific. Real-time PCR is more sensitive than antigen testing, but is more expensive. Often the PCR is multiplexed to detect four or more viral respiratory pathogens in the same assay. Rapid tissue culture methods take 48 hours and have comparable sensitivity, but require a carefully collected and handled specimen.
C. Imaging
Diffuse hyperinflation and peribronchiolar thickening are most common; atelectasis and patchy infiltrates also occur in uncomplicated infection, but pleural effusions are rare. Consolidation (usually subsegmental) occurs in 25% of children with lower respiratory tract disease.
 Differential Diagnosis
Differential Diagnosis
Although almost all cases of bronchiolitis are due to RSV during an epidemic, other viruses, including parainfluenza, rhinovirus, and especially human metapneumovirus, cannot be excluded. Mixed infections with other viruses, chlamydiae, or bacteria can occur. Wheezing may be due to asthma, a foreign body, or other airway obstruction. RSV infection may closely resemble chlamydial pneumonitis when fine crackles are present and fever and wheezing are not prominent. The two may also coexist. Cystic fibrosis may present with respiratory symptoms resembling RSV infection; a positive family history or failure to thrive associated with GI symptoms, hyponatremia or hypoalbuminemia should prompt a sweat chloride test. Pertussis should also be considered in this age group, especially if cough is prominent and the infant is younger than age 6 months. A markedly elevated leukocyte count should suggest bacterial superinfection (neutrophilia) or pertussis (lymphocytosis).
 Complications
Complications
RSV commonly infects the middle ear. Symptomatic otitis media is more likely when secondary bacterial infection is present (usually due to pneumococci or H influenzae). This is the most common complication (10%–20%) of RSV infection. Bacterial pneumonia complicates only 0.5%–1% of hospitalized patients. Sudden exacerbations of fever and leukocytosis should suggest bacterial infection. Respiratory failure or apnea may require mechanical ventilation, but occurs in less than 2% of hospitalized previously healthy full-term infants. Cardiac failure may occur as a complication of pulmonary disease or myocarditis. RSV commonly causes exacerbations of asthma. Nosocomial RSV infection is so common during outbreaks that elective hospitalization or surgery, especially for those with underlying illness, should be postponed. Well-designed hospital programs to prevent nosocomial spread are imperative (see next section).
 Prevention & Treatment
Prevention & Treatment
Children who are very hypoxic or cannot feed because of respiratory distress must be hospitalized and given humidified oxygen as directed by oxygen saturation, and given tube or intravenous feedings. Antibiotics, decongestants, and expectorants are of no value in routine infections. RSV-infected children should be kept in respiratory isolation. Cohorting ill infants in respiratory isolation during peak season (with or without rapid diagnostic attempts) and emphasizing good hand washing may greatly decrease nosocomial transmission.
The utility of bronchodilator therapy alone has not been consistently demonstrated. Often a trial of bronchodilator therapy is given to determine response and is subsequently discontinued if there is no improvement. Racemic epinephrine occasionally works when β-agonists fail. This therapeutic trial should only be undertaken in a hospital setting and care taken to observe children for an extended period after a positive response. The use of corticosteroids is also controversial in RSV bronchiolitis without complicating features such as asthma and chronic lung disease of prematurity. A meta-analysis of numerous studies of corticosteroid therapy indicated a significant effect on hospital stay, especially in those most ill at the time of treatment, but use of a single dose of corticosteroids in an outpatient setting had no lasting effect on respiratory status and did not prevent hospitalization. The combined use of racemic epinephrine and 5 days of oral dexamethasone significantly reduced hospitalization in one trial, but needs more evaluation before it can be recommended.
Ribavirin is the only licensed antiviral therapy used for RSV infection. It is given by continuous aerosolization. It is rarely used in infants without significant anatomic or immunologic defects. At best, there is a very modest effect on disease severity in immunocompetent infants with no underlying anatomic abnormality. Even in high-risk infants, a favorable clinical response to ribavirin therapy was not demonstrated in several studies, although some data suggest that it might be more efficacious if initiated early in the illness. Nevertheless, ribavirin is sometimes used in severely ill children who are immunologically or anatomically compromised and in those with severe cardiac disease.
Monthly intramuscular administration of humanized RSV monoclonal antibody is now recommended to prevent severe disease in selected high-risk patients during epidemic periods. Monthly administration should be considered during the RSV season for high-risk children (described in Chapter 10). Use of passive immunization for immunocompromised children is logical but not established. RSV antibody is not effective for treatment of established infection.
 Prognosis
Prognosis
Although mild bronchiolitis does not produce long-term problems, 30%–40% of patients hospitalized with this infection will wheeze later in childhood, and RSV infection in infancy may be an important precursor to asthma. Chronic restrictive lung disease and bronchiolitis obliterans are rare sequelae.
Geevarghese B, Simoes EA: Antibodies for prevention and treatment of respiratory syncytial virus infections in children. Antivir Ther 2012;17(1 Pt B):201 [PMID: 22311607].
Hall CB: The burgeoning burden of respiratory syncytial virus among children. Infect Disord Drug Targets 2012;12(2):92 [PMID: 22335498].
Krilov LR: Respiratory syncytial virus disease: update on treatment and prevention. Expert Rev Antiinfect Ther 2011;9(1): 27–32 [PMID: 21171875].
HUMAN METAPNEUMOVIRUS INFECTION
 General Considerations
General Considerations
Human metapneumovirus (hMPV) is a common agent of respiratory tract infections that is very similar to RSV in epidemiologic and clinical characteristics. Like RSV, parainfluenza, mumps, and measles, hMPV belongs to the paramyxovirus family. Humans are its only known reservoir. Seroepidemiologic surveys indicate that the virus has worldwide distribution. More than 90% of children contract hMPV infection by age 5 years, typically during late autumn through early spring outbreaks. hMPV accounts for 15%–25% of the cases of bronchiolitis and pneumonia in children younger than 2 years. Older children and adults can also develop symptomatic infection.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
The most common symptoms are fever, cough, rhinorrhea, and sore throat. Bronchiolitis and pneumonia occur in 40%–70% of the children who acquire hMPV before the age of 2 years. Asymptomatic infection is uncommon. Other manifestations include otitis, conjunctivitis, diarrhea, and myalgia. Acute wheezing has been associated with hMPV in children of all ages, raising the possibility that this virus, like RSV, might trigger reactive airway disease. Dual infection with hMPV and RSV or other respiratory viruses seems to be a common occurrence and may increase morbidity and mortality.
B. Laboratory Findings
The virus has very selective tissue culture tropism, which accounts for its late discovery in spite of its presence in archived specimens from the mid-1950s. The preferred method of diagnosis is PCR performed on respiratory specimens. Rapid shell vial culture is an acceptable, albeit less sensitive, alternative. Antibody tests are available, but are most appropriately used for epidemiologic studies.
C. Imaging
Lower respiratory tract infection frequently shows hyperinflation and patchy pneumonitis on chest radiographs.
 Treatment & Prognosis
Treatment & Prognosis
No antiviral therapy is available to treat hMPV. Ribavirin has in vitro activity against human metapneumovirus, but there are no data to support its therapeutic value. Children with lower respiratory tract disease may require hospitalization and ventilatory support, but less frequently than with RSV-associated bronchiolitis. Duration of hospitalization in hMPV is typically shorter than in RSV.
Edwards KM et al: Burden of human metapneumovirus infection in young children. N Engl J Med 2013;368:633 [PMID:].
Feuillet F, Lina B, Rosa-Calatrava M, Boivin G: Ten years of human metapneumovirus research. J Clin Virol 2012;53(2):97 [PMID: 22074934].
Kroll JL, Weinberg A: Human metapneumovirs. Sem Respir Crit Care Med 2011;32(4):447 [PMID: 21858749].
INFECTIONS DUE TO ENTEROVIRUSES
Enteroviruses are a major cause of illness in young children. The multiple types have similar nucleic acid and protein components, and may produce identical syndromes, but they differ antigenically, which makes vaccine development impractical and has hindered development of antigen detection and serologic tests. However, common RNA sequences and group antigens have led to diagnostic tests for viral nucleic acid and proteins. A PCR assay is available in many medical centers, but tissue culture is still used in some centers as a diagnostic method for echoviruses, polioviruses, and coxsackie B viruses. Although cultures may turn positive in 2–4 days, the relatively rapid answer obtained with PCR facilitates clinical decisions, particularly in cases of meningoencephalitis and severe unexplained illness in neonates.
Parechoviruses are a genus of the family picornaviruses which were formerly considered to be enteroviruses (echoviruses 22 and 23). It is now realized that these are responsible for a significant number of pediatric infections. Some of the 15 types of parechovirures infect almost every child before the age of 2 years; others before age 5 years.
Transmission of enteroviruses is fecal-oral or from upper respiratory secretions. Multiple enteroviruses circulate in the community at any one time; summer–fall outbreaks are common in temperate climates, but infections are seen year-round. After poliovirus, coxsackie B virus is most virulent, followed by echovirus. Neurologic, cardiac, and overwhelming neonatal infections are the most severe forms of illness.
ACUTE FEBRILE ILLNESS
Accompanied by nonspecific upper respiratory or enteric symptoms, the sudden onset of fever and irritability in infants or young children is often enteroviral in origin, especially in late summer and fall. More than 90% of enteroviral infections are not distinctive. Occasionally a petechial rash is seen; more often a diffuse maculopapular or morbilliform eruption (often prominent on palms and soles) occurs on the second to fourth day of fever. Rapid recovery is the rule. More than one febrile enteroviral illness can occur in the same patient in one season. The leukocyte count is usually normal. Infants, because of fever and irritability, may undergo an evaluation for bacteremia or meningitis and be hospitalized to rule out sepsis. Approximately half of these infants have aseptic meningitis. In the summer months enterovirus infection is more likely than human herpesvirus 6 (HHV-6) to cause an acute medical visit for fever. Duration of illness is 4–5 days.
Romero JR, Selvarangan R: The human parechoviruses: an overview. Adv Pediatr 2011;58(1):65 [PMID: 21736976].
RESPIRATORY TRACT ILLNESSES
1. Febrile Illness with Pharyngitis
This syndrome is most common in older children, who complain of headache, sore throat, myalgia, and abdominal discomfort. The usual duration is 3–4 days. Vesicles or papules may be seen in the pharynx. There is no exudate. Occasionally, enteroviruses are the cause of croup, bronchitis, or pneumonia. They may also exacerbate asthma.
2. Herpangina
Herpangina is characterized by an acute onset of fever and posterior pharyngeal grayish white vesicles that quickly form ulcers (< 20 in number), often linearly arranged on the posterior palate, uvula, and tonsillar pillars. Bilateral faucial ulcers may also be seen. Dysphagia, vomiting, abdominal pain, and anorexia also occur and, rarely, parotitis or vaginal ulcers. Symptoms disappear in 4–5 days. The epidemic form is due to several coxsackie A viruses; coxsackie B viruses and echoviruses cause sporadic cases.
The differential diagnosis includes primary herpes simplex gingivostomatitis (ulcers are more prominent anteriorly, and gingivitis is present), aphthous stomatitis (fever absent, recurrent episodes, anterior lesions), trauma, hand-foot-and-mouth disease (see later discussion), and Vincent angina (painful gingivitis spreading from the gum line, underlying dental disease). If the enanthema is missed, tonsillitis might be incorrectly diagnosed.
3. Acute Lymphonodular Pharyngitis
Coxsackievirus A10 has been associated with a febrile pharyngitis characterized by nonulcerative yellow-white posterior pharyngeal papules in the same distribution as herpangina. The duration is 1–2 weeks; therapy is supportive.
4. Pleurodynia (Bornholm Disease, Epidemic Myalgia)
Caused by coxsackie B virus (epidemic form) or many nonpolio enteroviruses (sporadic form), pleurodynia is associated with an abrupt onset of unilateral or bilateral spasmodic pain of variable intensity over the lower ribs or upper abdomen. Associated symptoms include headache, fever, vomiting, myalgias, and abdominal and neck pain. Physical findings include fever, chest muscle tenderness, decreased thoracic excursion, and occasionally a friction rub. The chest radiograph is normal. Hematologic tests are nondiagnostic. The illness generally lasts less than 1 week.
This is a disease of muscle, but the differential diagnosis includes bacterial pneumonia, bacterial and tuberculous effusion, and endemic fungal infections (all excluded radio-graphically and by auscultation), costochondritis (no fever or other symptoms), and a variety of abdominal problems, especially those causing diaphragmatic irritation.
There is no specific therapy. Potent analgesic agents and chest splinting alleviate the pain.
Tagarakis GI et al: Bornholm disease—a pediatric clinical entity that can alert a thoracic surgeon. J Paed Child Health 2011;47(4):242 [PMID: 21501275].
RASHES (INCLUDING HAND-FOOT- AND-MOUTH DISEASE)
The rash can be macular, maculopapular, urticarial, scarlatiniform, petechial, or vesicular. One of the most characteristic is that of hand-foot-and-mouth disease (caused by coxsackieviruses, especially types A5, A10, and A16), in which vesicles or red papules are found on the tongue, oral mucosa, hands, and feet. Often they appear near the nails and on the heels. Associated fever, sore throat, and malaise are mild. The rash may appear when fever abates, simulating roseola.
Cardiac Involvement
Myocarditis and pericarditis can be caused by a number of nonpolio enteroviruses, particularly type B coxsackieviruses. Most commonly, upper respiratory symptoms are followed by substernal pain, dyspnea, and exercise intolerance. A friction rub or gallop may be detected. Ultrasound will define ventricular dysfunction or pericardial effusion, and electrocardiography may show pericarditis or ventricular irritability. Creatine phosphokinase may be elevated. The disease may be mild or fatal; most children recover completely. In infants, other organs may be involved at the same time; in older patients, cardiac disease is usually the sole manifestation (see Chapter 20 for therapy). Enteroviral RNA is present in cardiac tissue in some cases of dilated cardiomyopathy or myocarditis; the significance of this finding is unknown. Epidemics of enterovirus 71, which occur in Asia, as well as sporadic cases in the United States, are associated with severe left ventricular dysfunction and pulmonary edema following typical mucocutaneous manifestations of enterovirus infection. Enterovirus 71 also can cause isolated severe neurologic disease or neurologic disease in combination with myocardial disease.
Badran SA, Midgley S, Andersen P, Bottigner B: Clinical and virological features of enterovirus 71 infection in Denmark, 2005–2008. Scand J Infect Dis 2011;43(8):642 [PMID: 21526904].
Ooi MH et al: Clinical features, diagnosis, and management of enterovirus 71. Lancet Neurol 2010;9(11):1097 [PMID: 20965438].
Simpson KE, Canter CE: Acute myocarditis in children. Expert Opin Cardiovasc Ther 2011;9(6):771 [PMID: 21714608].
Severe Neonatal Infection
Sporadic and nosocomial nursery cases of severe systemic enteroviral disease occur. Clinical manifestations include combinations of fever, rash, pneumonitis, encephalitis, hepatitis, gastroenteritis, myocarditis, pancreatitis, and myositis. The infants, usually younger than 1 week, may appear septic, with cyanosis, dyspnea, and seizures. The differential diagnosis includes bacterial and herpes simplex infections, necrotizing enterocolitis, other causes of heart or liver failure, and metabolic diseases. Diagnosis is suggested by the finding of cerebrospinal fluid (CSF) mononuclear pleocytosis and confirmed by the isolation of virus or detection of enteroviral RNA in urine, stool, CSF, or pharynx. Therapy is supportive. IVIG is often administered, but its value is uncertain. Passively acquired maternal antibody may protect newborns from severe disease. For this reason, labor should not be induced in pregnant women near term who have suspected enteroviral disease. Some of these infections are now known to be caused by parechoviruses.
Tebruegge M, Curtis N: Enterovirus infections in neonates. Semin Fetal Neonatal Med 2009;14:222 [PMID: 19303380].
CENTRAL NERVOUS SYSTEM ILLNESSES
1. Poliomyelitis
 General Considerations
General Considerations
Poliovirus infection is subclinical in 90%–95% of cases; it causes nonspecific febrile illness in about 5% of cases and aseptic meningitis, with or without paralytic disease, in 1%–3%. In endemic areas, most of older children and adults are immune because of prior inapparent infections. Occasional cases in the United States occur in patients who travel to foreign countries or come in contact with visitors from areas that have poliovirus outbreaks. Severe poliovirus infection was a rare complication of OPV (oral poliovirus vaccine) vaccination as a result of reversion of the vaccine virus. The incidence of vaccine-associated paralytic poliomyelitis (VAPP) in the United States was 1:750,000 and 1:2.4 million doses for the first and second dose of OPV, respectively. Although rare, VAPP became more common than wild-type poliomyelitis in the United States in the 1980s. This led to a change in the recommended immunization regimen, substituting inactivated poliovirus vaccine (IPV) for OPV (see Chapter 10).
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
The initial symptoms are fever, myalgia, sore throat, and headache for 2–6 days. In less than 10% of infected children, several symptom-free days are followed by recurrent fever and signs of aseptic meningitis: headache, stiff neck, spinal rigidity, and nausea. Mild cases resolve completely. In only 1%–2% of these children do high fever, severe myalgia, and anxiety portend progression to loss of reflexes and subsequent flaccid paralysis. Sensation remains intact, although hyperesthesia of skin overlying paralyzed muscles is common and pathognomonic.
Paralysis is usually asymmetrical. Proximal limb muscles are more often involved than distal, and lower limb involvement is more common than upper. Bulbar involvement affects swallowing, speech, and cardiorespiratory function and accounts for most deaths. Bladder distention and marked constipation characteristically accompany lower limb paralysis. Paralysis is usually complete by the time the temperature normalizes. Weakness often resolves completely. Atrophy is usually apparent by 4–8 weeks. Most improvement of muscle paralysis occurs within 6 months.
B. Laboratory Findings
In patients with meningeal symptoms, the CSF contains up to several hundred leukocytes (mostly lymphocytes) per μL; the glucose level is normal, and protein concentration is mildly elevated. Poliovirus is easy to grow in cell culture and can be readily differentiated from other enteroviruses. It is rarely isolated from spinal fluid but is often present in the throat and stool for several weeks following infection. Paired serology is also diagnostic. Laboratory methods are available to differentiate wild from attenuated vaccine isolates.
 Differential Diagnosis
Differential Diagnosis
Aseptic meningitis due to poliovirus is indistinguishable from that due to other viruses. Paralytic disease in the United States is usually due to nonpolio enteroviruses. Polio may resemble Guillain-Barré syndrome (minimal sensory loss, ascending symmetrical loss of function; minimal pleocytosis, high protein concentration in spinal fluid), polyneuritis (sensory loss), pseudoparalysis due to bone or joint problems (eg, trauma, infection), botulism, or tick paralysis.
 Complications & Sequelae
Complications & Sequelae
Complications are the result of the acute and permanent effects of paralysis. Respiratory, pharyngeal, bladder, and bowel malfunction are most critical. Deaths are usually due to complications arising from respiratory dysfunction. Limbs injured near the time of infection, such as by intramuscular injections, excessive prior use, or trauma, tend to be most severely involved and have the worst prognosis for recovery (provocation paralysis).
 Treatment & Prognosis
Treatment & Prognosis
Therapy is supportive. Bed rest, fever and pain control (heat therapy is helpful), and careful attention to progression of weakness (particularly of respiratory muscles) are important. No intramuscular injections should be given during the acute phase. Intubation or tracheostomy for secretion control and catheter drainage of the bladder may be needed. Assisted ventilation and enteral feeding may also be needed. Disease is worse in adults and pregnant women than in children. Postpolio muscular atrophy occurs in 30%–40% of paralyzed limbs 20–30 years later, characterized by increasing weakness and fasciculations in previously affected, partially recovered limbs.
2. Nonpolio Viral Meningitis
Nonpolio enteroviruses cause over 80% of cases of aseptic meningitis at all ages. In the summer and fall, cases may be seen associated with circulation of multiple neurotropic strains. Nosocomial outbreaks also occur.
 Clinical Findings
Clinical Findings
The usual enteroviral incubation period is 4–6 days. Because many enteroviral infections are subclinical or not associated with central nervous system (CNS) symptoms, a history of contact with a patient with meningitis is unusual. Neonates may acquire infection from maternal blood, vaginal secretions, or feces at birth; occasionally the mother has had a febrile illness just prior to delivery.
A. Symptoms and Signs
Incidence is much greater in children younger than age 1 year. Onset is usually acute with variable fever, marked irritability, and lethargy in infants. Older children also describe frontal headache, photophobia, and myalgia. Abdominal pain, diarrhea, and vomiting may occur. The incidence of rash varies with the infecting strain. If rash occurs, it is usually seen after several days of illness and is diffuse, macular or maculopapular, occasionally petechial, but not purpuric. Oropharyngeal vesicles and rash on the palms and soles suggest an enterovirus. The anterior fontanelle may be full. Meningismus may be present. The illness may be biphasic, with nonspecific symptoms and signs preceding those related to the CNS. In older children, it is easier to demonstrate meningeal signs. Seizures are unusual, and focal neurologic findings, which are rare, should lead to a search for an alternative cause. Frank encephalitis, which is uncommon at any age, occurs most often in neonates. Because of the overall frequency of enteroviral disease in children, 5%–10% of all cases of encephalitis of proved viral origin are caused by enteroviruses. Enteroviruses tend to cause less severe encephalitis than other viral agents. However, parechoviruses, which have recently been demonstrated to be a significant cause of aseptic meningitis, sometimes cause white matter defects.
Enterovirus 71 infections that begin with typical mucocutaneous manifestations of enteroviruses can be complicated by severe brainstem encephalitis and polio-like flaccid paralysis. Enterovirus 70 outbreaks have resulted in hemorrhagic conjunctivitis together with paralytic poliomyelitis. Other nonpolio enteroviruses cause sporadic cases of acute motor weakness similar to that seen with poliovirus infection. Children with congenital immune deficiency, especially agammaglobulinemia, are subject to chronic enteroviral meningoencephalitis that is often fatal or associated with severe sequelae.
B. Laboratory Findings
Blood leukocyte counts are often normal. The spinal fluid leukocyte count is 100–1000/μL. Early in the illness, polymorphonuclear cells predominate; a shift to mononuclear cells occurs within 8–36 hours. In about 95% of cases, spinal fluid parameters include a total leukocyte count less than 3000/μL, protein less than 80 mg/dL, and glucose more than 60% of serum values. Marked deviation from any of these findings should prompt consideration of another diagnosis (see following section). The syndrome of inappropriate secretion of antidiuretic hormone may occur, but is rarely clinically significant.
Culture of CSF may yield an enterovirus within a few days (< 70%). However, PCR for enteroviruses is the most useful diagnostic method in many centers (sensitivity > 90%) and can give an answer within 24–48 hours. Parechoviruses will be detected by most PCR methods, but will be identified as “enterovirus.” Virus may be detected in acellular CSF. Detection of an enterovirus from throat or stool suggests, but does not prove, enteroviral meningitis. Vaccine-strain poliovirus present in feces in infants being evaluated for aseptic meningitis (outside of the United States) may confuse the diagnosis, but can usually be distinguished by growth characteristics.
C. Imaging
Cerebral imaging is not often indicated; if done, it is usually normal. Subdural effusions, infarcts, edema, or focal abnormalities seen in bacterial meningitis are absent except for the rare case of focal encephalitis.
 Differential Diagnosis
Differential Diagnosis
The leading cause of aseptic meningitis is enteroviruses, especially in the summer and fall. Other causative viruses are mosquito-borne viruses (flavivirus, bunyavirus). These are usually considered during an investigation of encephalitis, but many of them are more likely to cause isolated meningitis and should be considered when seasonal clusters of viral meningitis occur. Primary herpes simplex infection can cause aseptic meningitis in adolescents who have a genital herpes infection. In neonates, early herpes simplex meningoencephalitis may mimic enteroviral disease (see section on Infections due to Herpesviruses). This is an important alternative diagnosis to exclude because of the need for urgent antiviral therapy. Lymphocytic choriomeningitis virus causes meningitis in children in contact with rodents (pet or environmental exposure). Meningitis occurs in some patients at the time of infection with human immunodeficiency virus (HIV).
Other causes of aseptic meningitis that may resemble enteroviral infection include partially treated bacterial meningitis (recent antibiotic treatment, CSF parameters resembling those seen in bacterial disease and bacterial antigen sometimes present); parameningeal foci of bacterial infection such as brain abscess, subdural empyema, mastoiditis (predisposing factors, glucose level in CSF may be lower, focal neurologic signs, and characteristic imaging); tumors or cysts (malignant cells detected by cytologic examination, a history of neurologic symptoms, higher protein concentration or lower glucose level in CSF); trauma (presence, without exception, of red blood cells, which may be erroneously assumed to be due to traumatic lumbar puncture, but are crenated and fail to clear); vasculitis (other systemic or neurologic signs, found in older children); tuberculous or fungal meningitis (see Chapters 42 and 43); cysticercosis; parainfectious encephalopathies (M pneumoniae, cat-scratch disease, respiratory viruses [especially influenza]); Lyme disease; leptospirosis; and rickettsial diseases.
 Prevention & Treatment
Prevention & Treatment
No specific therapy exists. Infants are usually hospitalized, isolated, and treated with fluids and antipyretics. Moderately to severely ill infants are given appropriate antibiotics for bacterial pathogens until cultures are negative for 48–72 hours. This practice is changing, and hospital stay shortened, in areas where the PCR assay for enteroviruses is available. If patients, especially older children, are mildly ill, antibiotics may be withheld and the child observed. The illness usually lasts less than 1 week. Codeine compounds or other strong analgesics may be needed. C-reactive protein and lactate levels are usually low in the CSF of children with viral meningitis; both may be elevated with bacterial infection. With clinical deterioration, repeat lumbar puncture, cerebral imaging, neurologic consultation, and more aggressive diagnostic tests should be considered. Herpesvirus encephalitis is an important consideration in such cases, particularly in infants younger than age 1 month, and often warrants empiric acyclovir therapy until an etiologic diagnosis is made.
 Prognosis
Prognosis
In general, enteroviral meningitis has no significant short-term neurologic or developmental sequelae. Developmental delay may follow severe neonatal infections. Unlike mumps, enterovirus infections rarely cause hearing loss.
Poh CL, Tan EL: Detection of enteroviruses from clinical specimens. Meth Molecular Biol 2011;665:65 [PMID: 21116796].
Rhoades RE et al: Enterovirus infections of the central nervous system. Virology 2011;411(2):288 [PMID: 21251690].
INFECTIONS DUE TO HERPESVIRUSES
HERPES SIMPLEX INFECTIONS
 General Considerations
General Considerations
There are two types of herpes simplex virus (HSV). Type 1 (HSV-1) causes most cases of oral, skin, and cerebral disease in older children. Type 2 (HSV-2) causes most (> 50%, especially in adolescents and young adults) genital and congenital infections, although HSV-1 has become a much more common cause of infection at these sites. Latent infection is routinely established in sensory ganglia during primary infection. Recurrences may be spontaneous or induced by external events (eg, fever, menstruation, or sunlight) or immunosuppression. Transmission is by direct contact with infected secretions. HSV is very susceptible to antiviral drugs.
Primary infection with HSV-1 often occurs early in childhood, although many adults (20%–50%) never get infected. Primary infection with HSV-1 is subclinical in 80% of cases and causes gingivostomatitis in the remainder. HSV-2, which is transmitted sexually, is also usually (65%) sub-clinical or produces mild, nonspecific symptoms. Infection with one type of HSV may prevent or attenuate clinically apparent infection with the other type, but individuals can be infected at different times with both HSV-1 and HSV-2. Recurrent episodes are due to reactivation of latent HSV.
The source of primary infection is usually an asymptomatic excreter. Most previously infected individuals shed HSV at irregular intervals. At any one time (point prevalence), more than 5% of normal seropositive adults excrete HSV-1 in the saliva; the percentage is higher in recently infected children, and detection of viral DNA exceeds 12%. HSV-2 shedding in genital secretions occurs with a similar or higher point prevalence exceeding 15%, depending on the method of detection (viral isolation vs PCR) and the interval since the initial infection. A history of contact with an active HSV infection is unusual.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
1. Gingivostomatitis—High fever, irritability, and drooling occur in infants. Multiple oral ulcers are seen on the tongue and on the buccal and gingival mucosa, occasionally extending to the pharynx. Pharyngeal ulcers may predominate in older children and adolescents. Diffusely swollen red gums that are friable and bleed easily are typical. Cervical nodes are swollen and tender. Duration is 7–14 days. Herpangina, aphthous stomatitis, thrush, and Vincent angina should be excluded.
2. Vulvovaginitis or urethritis (See Chapter 44)—Genital herpes (especially HSV-2) in a prepubertal child should suggest sexual abuse. Vesicles or painful ulcers on the vulva, vagina, or penis, and tender adenopathy are seen. Systemic symptoms (fever, flulike illness, myalgia) are common with the initial episode. Painful urination is frequent, especially in females. Primary infection lasts 10–14 days before healing. Lesions may resemble trauma, syphilis (ulcers are painless), or chancroid (ulcers are painful and nodes are erythematous and fluctuant) in the adolescent, and bullous impetigo or severe chemical irritation in younger children.
3. Cutaneous infections—Direct inoculation onto cuts or abrasions may produce localized vesicles or ulcers. A deep HSV infection on the finger (called herpetic whitlow) may be mistaken for a bacterial felon or paronychia; surgical drainage is of no value and is contraindicated. HSV infection of eczematous skin may result in extensive areas of vesicles and shallow ulcers (eczema herpeticum), which may be mistaken for impetigo or varicella.
4. Recurrent mucocutaneous infection—Recurrent oral shedding is asymptomatic. Perioral recurrences often begin with a prodrome of tingling or burning limited to the vermillion border, followed by vesiculation, scabbing, and crusting around the lips over 3–5 days. Recurrent intraoral lesions are rare. Fever, adenopathy, and other symptoms are absent. Recurrent cutaneous herpes most closely resembles impetigo, but the latter is often outside the perinasal and perioral region, recurs infrequently in the same area of skin, responds to antibiotics, yields a positive result on Gram stain, and Streptococcus pyogenes or Staphylococcus aureus can be isolated. Recurrent genital disease is common after the initial infection with HSV-2. It is shorter (5–7 days) and milder (mean, four lesions) than primary infection and is not associated with systemic symptoms. Recurrent genital disease, which may also recur on the thighs and buttocks, is also preceded by a cutaneous sensory prodrome. Recurrence of HSV-1 in the genital region is much less common than occurs after HSV-2 infection.
5. Keratoconjunctivitis—Keratoconjunctivitis may be part of a primary infection due to spread from infected saliva. Most cases are caused by reactivation of virus latent in the ciliary ganglion. Keratoconjunctivitis produces photophobia, pain, and conjunctival irritation. With recurrences, dendritic corneal ulcers may be demonstrable with fluorescein staining. Stromal invasion may occur. Corticosteroids should never be used for unilateral keratitis without ophthalmologic consultation. Other causes of these symptoms include trauma, bacterial infections, and other viral infections (especially adenovirus if pharyngitis is present; bilateral involvement makes HSV unlikely) (see Chapter 16).
6. Encephalitis—Although unusual in infants outside the neonatal period, encephalitis may occur at any age, usually without cutaneous herpes lesions. In older children, HSV encephalitis can follow a primary infection, but often represents reactivation of latent virus. HSV is the most common cause of sporadic severe encephalitis. Diagnosing this cause of encephalitis is very important because it can be treated with specific antiviral therapy. Acute onset is associated with fever, headache, behavioral changes, and focal neurologic deficits and/or focal seizures. Mononuclear pleocytosis is typically present along with an elevated protein concentration, which continues to rise on repeat lumbar punctures. In older children, hypodense areas with a medial and inferior temporal lobe predilection are seen on CT scan, especially after 3–5 days, but the findings in infants may be more diffuse. Magnetic resonance imaging (MRI) is more sensitive and is positive sooner. Periodic focal epileptiform discharges are seen on electroencephalograms, but are not diagnostic of HSV infection. Viral cultures of CSF are rarely positive. The PCR assay to detect HSV DNA in CSF is a sensitive and specific rapid test. Without early antiviral therapy, the prognosis is poor. The differential diagnosis includes mumps, mosquito-borne and other viral encephalitides, parainfectious and postinfectious encephalopathy, brain abscess, acute demyelinating syndromes, and bacterial meningoencephalitis.
7. Neonatal infections—Infection is occasionally acquired by ascending spread prior to delivery (< 5% of cases), but most often occurs at the time of vaginal delivery from a mother with genital infection. Eight to fifteen percent of HSV-2–seropositive pregnant women at delivery have HSV-2 detected by PCR in the genital tract. However, in most cases this represents reactivation of infection acquired in the distant past. Neonatal infection is rarely acquired from mothers with reactivation disease, whereas it is frequently acquired during delivery of mothers with current or very recent primary infection. This is because transplacentally acquired antibody is usually protective. Occasionally, the infection is acquired in the postpartum period from oral secretions of family members or hospital personnel. A history of genital herpes in the mother may be absent. Within a few days and up to 6 weeks (most often within 4 weeks), skin vesicles appear (especially at sites of trauma, such as where scalp monitors were placed). Some infants (45%) have infection limited to the skin, eye, or mouth. Other infants are acutely ill, presenting with jaundice, shock, bleeding, or respiratory distress (20%). Some infants appear well initially, but dissemination of the infection to the brain or other organs becomes evident during the ensuing week. HSV infection (and empiric therapy) should be strongly considered in newborns with the sepsis syndrome that is unresponsive to antibiotic therapy and has negative bacterial cultures. Some infected infants exhibit only neurologic symptoms at 2–3 weeks after delivery: apnea, lethargy, fever, poor feeding, or persistent seizures. The brain infection in these children is often diffuse and is best diagnosed by MRI. The skin lesions may resemble impetigo, bacterial scalp abscesses, or miliaria. Skin lesions may be absent at the time of presentation or may never develop. Skin lesions may recur over weeks or months after recovery from the acute illness. Progressive culture–negative pneumonitis is another manifestation of neonatal HSV. Most cases of neonatal herpes infection are acquired from mothers with undiagnosed genital herpes, most of whom acquired the infection during the pregnancy—especially near term.
B. Laboratory Findings
With multisystem disease, abnormalities in platelets, clotting factors, and liver function tests are often present. A finding of lymphocytic pleocytosis and elevated CSF protein indicates viral meningitis or encephalitis. Virus may be cultured from infected epithelial sites (vesicles, ulcers, or conjunctival scrapings). Cultures of CSF yield positive results in about 50% of neonatal cases, but are uncommon in older children. HSV will be detected within 2 days by rapid tissue culture methods, but PCR is the preferred diagnostic method for all specimens. A positive test from skin, throat, eye, or stool of a newborn is diagnostic. Vaginal culture of the mother may offer circumstantial evidence for the diagnosis, but may be negative.
Rapid diagnostic tests include immunofluorescent stains or ELISA to detect viral antigen in skin or mucosal scrapings. The PCR assay for HSV DNA is positive (> 95%) in the CSF when there is brain involvement. Serum is often positive in the presence of multisystem disease. Typing of genital HSV isolates from adolescents has prognostic value, since HSV-1 genital infection recurs much less frequently than genital HSV-2 infection.
 Complications, Sequelae, & Prognosis
Complications, Sequelae, & Prognosis
Gingivostomatitis may result in dehydration due to dysphagia; severe chronic oral disease and esophageal involvement may occur in immunosuppressed patients. Primary vulvovaginitis may be associated with aseptic meningitis, paresthesias, autonomic dysfunction due to neuritis (urinary retention, constipation), and secondary candidal infection. HIV transmission from individuals who are also seropositive for HSV infection is facilitated, and HIV acquisition is enhanced in HSV-infected contacts. Extensive cutaneous disease (as in eczema) may be associated with dissemination and bacterial superinfection. Keratitis may result in corneal opacification or perforation. Untreated encephalitis is fatal in 70% of patients and causes severe damage in most of the remainder. When acyclovir treatment is instituted early, 20% of patients die and 40% are neurologically impaired.
Disseminated neonatal infection (25% of cases) is fatal for 30% of neonates in spite of therapy, and 20% of survivors are often impaired. Infants with CNS infection (30% of cases) have a 5% mortality with therapy and 70% of survivors are impaired; treated neonates with infection limited to skin, eye, and mouth survive, most often without sequelae.
 Treatment
Treatment
A. Specific Measures
HSV is sensitive to antiviral therapy.
1. Topical antivirals—Antiviral agents are effective for corneal disease and include 1% trifluridine and 3% acyclovir (1–2 drops five times daily). These agents should be used with the guidance of an ophthalmologist and used concurrently with oral antiviral therapy. They are inferior to oral formulations for treating mucocutaneous and genital infections.
2. Mucocutaneous HSV infections—These infections respond to administration of oral nucleoside analogues (acyclovir, valacyclovir, or famciclovir). The main indications are severe genital HSV infection in adolescents (see Chapter 44; acyclovir, 400 mg three times daily for 7–10 days) and severe gingivostomatitis in young children. Antiviral therapy is beneficial for primary disease when begun early. Recurrent disease rarely requires therapy. Frequent genital recurrences may be suppressed by oral administration of nucleoside analogues (acyclovir, 400 mg twice daily), but this approach should be used sparingly. Other forms of severe cutaneous disease, such as eczema herpeticum, respond to these antivirals. Intravenous acyclovir may be required when disease is extensive in immunocompromised children (10–15 mg/kg or 500 mg/m2 every 8 hours for 14–21 days). Oral acyclovir, which is available in suspension, is also used within 72–96 hours for severe primary gingivostomatitis in immunocompetent young children (20 mg/kg per dose [maximum of 400 mg per dose] four times a day for 7 days). Antiviral therapy does not alter the incidence or severity of subsequent recurrences of oral or genital infection. Development of resistance to antivirals, which is very rare after treating immunocompetent patients, occurs in immunocompromised patients who receive frequent and prolonged therapy.
3. Encephalitis—Treatment consists of intravenous acyclovir, 20 mg/kg (500 mg/m2) every 8 hours for 21 days.
4. Neonatal infection—Newborns receive intravenous acyclovir, 20 mg/kg every 8 hours for 21 days (14 days if infection is limited to skin, eye, or mouth). Therapy should not be discontinued in neonates with CNS disease unless a repeat CSF HSV PCR assay is negative near the end of treatment. The outcome at one year is improved in infants that receive oral acyclovir (300 mg/m2/dose three times daily) for 6 months after completion of IV therapy.
B. General Measures
1. Gingivostomatitis—Gingivostomatitis is treated with pain relief and temperature control measures. Maintaining hydration is important because of the long duration of illness (7–14 days). Nonacidic, cool fluids are best. Topical anesthetic agents (eg, viscous lidocaine or an equal mixture of kaolin–attapulgite [Kaopectate], diphenhydramine, and viscous lidocaine) may be used as a mouthwash for older children who will not swallow it; ingested lidocaine may be toxic to infants or may lead to aspiration. Antiviral therapy is indicated in normal hosts with severe disease. Antibiotics are not helpful.
2. Genital infections—Genital infections may require pain relief, assistance with voiding (warm baths, topical anesthetics, rarely catheterization), and psychological support. Lesions should be kept clean; drying may shorten the duration of symptoms. Sexual contact should be avoided during the interval from prodrome to crusting stages. Because of the frequency of asymptomatic shedding, the only effective way to prevent spread is the use of condoms. Candidal superinfection occurs in 10% of women with primary genital infections.
3. Cutaneous lesions—Skin lesions should be kept clean, dry, and covered if possible to prevent spread. Systemic analgesics may be helpful. Secondary bacterial infection is uncommon in patients with lesions on the mucosa or involving small areas. Secondary infection should be considered and treated if necessary (usually with an antistaphylococcal agent) in patients with more extensive lesions.
4. Recurrent cutaneous disease—Recurrent disease is usually milder than primary infection. Sun block lip balm helps prevent labial recurrences that follow intense sun exposure. There is no evidence that the many popular topical or vitamin therapies are efficacious.
5. Keratoconjunctivitis—An ophthalmologist should be consulted regarding the use of cycloplegics, anti-inflammatory agents, local debridement, and other therapies.
6. Encephalitis—Extensive support will be required for obtunded or comatose patients. Rehabilitation and psychological support are often needed for survivors.
7. Neonatal infection—The affected infant should be isolated and given acyclovir. Cesarean delivery is indicated if the mother has obvious cervical or vaginal lesions, especially if these represent primary infection (35%–50% transmission rate). With infants born vaginally to mothers who have active lesions of recurrent genital herpes, appropriate cultures should be obtained at 24–48 hours after birth, and the infant should be observed closely. Treatment is given to infants whose culture results are positive or who have suggestive signs or symptoms. Infants born to mothers with obvious primary genital herpes should receive therapy before the culture results are known. For women with a history of genital herpes infection, but no genital lesions, vaginal delivery with peripartum cultures of maternal cervix is the standard. Clinical follow-up of the newborn is recommended when maternal culture results are positive. Repeated cervical cultures during pregnancy are not useful.
A challenging problem is the newborn, especially in the first 3 weeks of life, that presents with fever (or hypothermia) and a sepsis-like picture. This is further confounded in the late summer by the existence of circulating enteroviruses. These infants should be considered for empiric acyclovir therapy, pending results of PCR studies, given the poor outcome of disseminated herpes in the newborn. The index of suspicion is increased when there is a CSF pleocytosis, elevated hepatic transaminase levels, a very ill-appearing infant, rash, or respiratory distress.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree












































