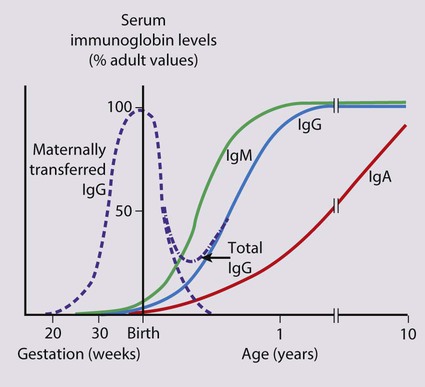
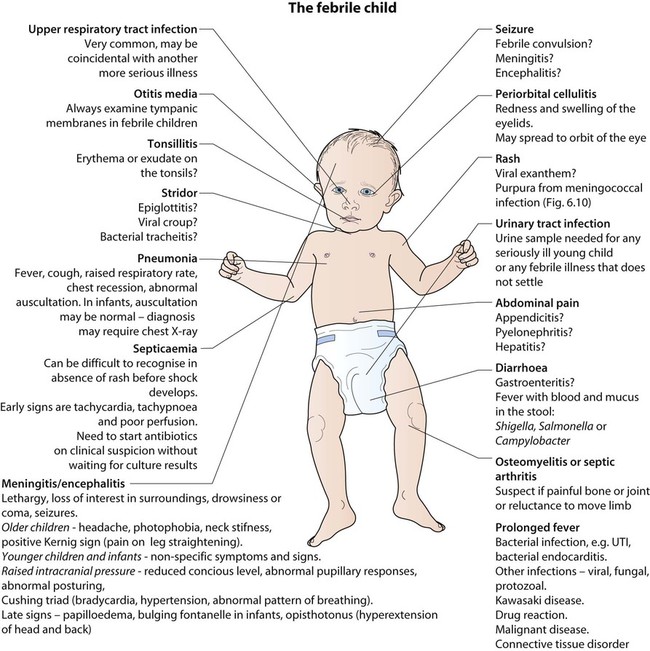
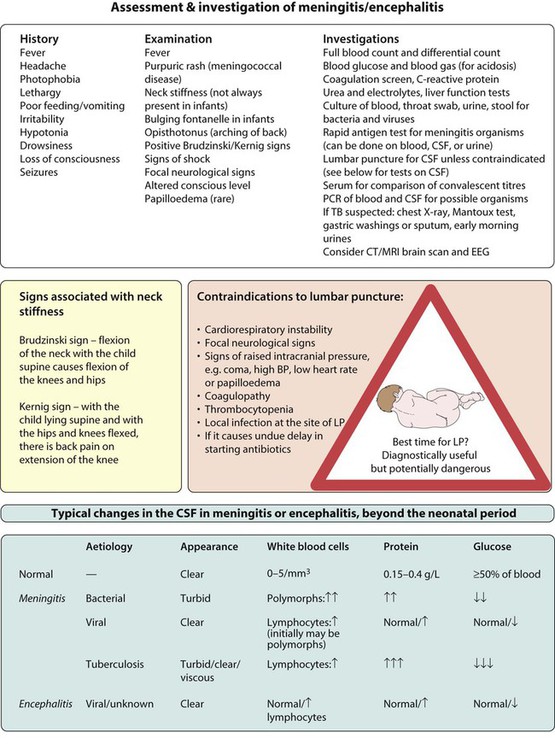
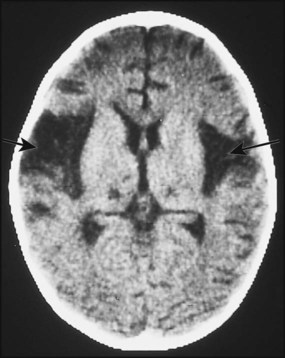
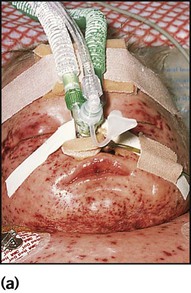
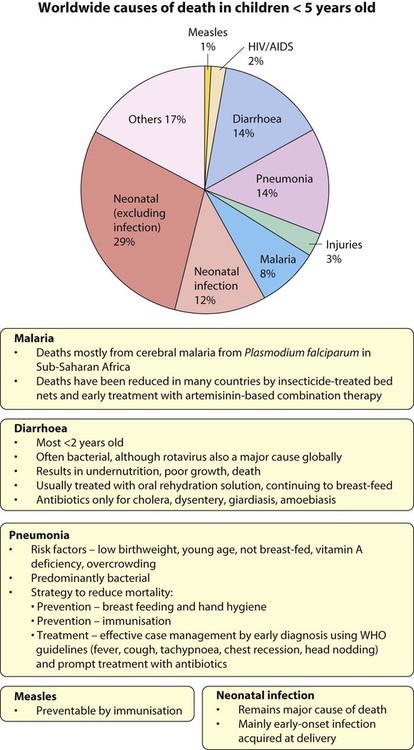
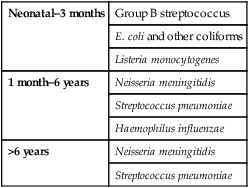
Infections are the most common cause of acute illness in children. Worldwide, acute respiratory infections, diarrhoea, neonatal infection, malaria, measles and HIV infection, often accompanied by undernutrition, are responsible for the deaths of more than 4.5 million children <5 years old annually (Fig. 14.1). When assessing a febrile child, consider the following. Parents usually know if their child has been febrile. In hospital, it is measured at: • <4 weeks old by an electronic thermometer in the axilla • 4 weeks to 5 years by an electronic or chemical dot thermometer in the axilla or infrared tympanic thermometer. In general, axillary temperatures underestimate body temperature by 0.5°C. Febrile infants <3 months old present with non-specific clinical features (see Box 10.2) and often have a bacterial infection, which cannot be identified reliably on clinical examination alone. It is uncommon for them to have the common viral infections of older infants and children because of passive immunity from their mothers (Fig. 14.2). Unless a clear cause for the fever is identified, they require urgent investigation with a septic screen (Box 14.1) and intravenous antibiotic therapy given immediately to avoid the illness becoming more severe and to prevent rapid spread to other sites of the body. This is considered in more detail in the section on neonatal infection (Chapter 10 Neonatal medicine). • Illness of other family members • If a specific illness is prevalent in the community • Recent travel abroad, e.g. malaria, typhoid • Contact with animals, e.g. brucellosis. • Increased susceptibility from immunodeficiency. This is usually secondary, e.g. post-autosplenectomy in sickle cell disease or splenectomy or nephrotic syndrome, resulting in increased susceptibility to encapsulated organisms (Streptococcus pneumoniae, Haemophilus influenzae and salmonella), or rarely, primary immune deficiency. Examination may identify a focus of infection (Fig. 14.3). If identified, investigations and management will be directed towards its treatment. However, if no focus is identified, this is often because it is the prodromal phase of a viral illness, but may indicate serious bacterial infection, especially urinary tract infection or septicaemia. Children who are not seriously ill can be managed at home with regular review by the parents, as long as they are given clear instructions (e.g. what clinical features should prompt reassessment by a doctor). Children who are significantly unwell, particularly if there is no focus of infection, will require investigations and observation or treatment in a paediatric assessment unit or A&E department or children’s ward. A septic screen will be required (Box 14.1). This is considered in Chapter 6 on Paediatric Emergencies. The organisms which commonly cause bacterial meningitis vary according to the child’s age (Table 14.1). Table 14.1 Organisms causing bacterial meningitis according to age The clinical features are listed in Figure 14.4. The early signs and symptoms of meningitis are non-specific, especially in infants and young children. Only children old enough to talk are likely to describe the classical meningitis symptoms of headache, neck stiffness and photophobia. But neck stiffness may also be seen in some children with tonsillitis and cervical lymphadenopathy. As children with meningitis may also be septicaemic, signs of shock, such as tachycardia, tachypnoea, prolonged capillary refill time, and hypotension, should be sought. Purpura in a febrile child of any age should be assumed to be due to meningococcal sepsis, even if the child does not appear unduly ill at the time; meningitis may or may not be present. The essential investigations are listed in Figure 14.4. A lumbar puncture is performed to obtain CSF to confirm the diagnosis, identify the organism responsible, and its antibiotic sensitivity. If any of the contraindications listed in Figure 14.4 are present, a lumbar puncture should not be performed, as under these circumstances, the procedure carries a risk of coning of the cerebellum through the foramen magnum. In these circumstances, a lumbar puncture can be postponed until the child’s condition has stabilised. Even without a lumbar puncture, bacteriological diagnosis can be achieved in at least 50% of cases from the blood by culture or polymerase chain reaction (PCR), and rapid antigen screens can be performed on blood and urine samples. Throat swabs should also be obtained for bacterial and viral cultures. A serological diagnosis can be made on convalescent serum 4–6 weeks after the presenting illness if necessary. • Hearing loss. Inflammatory damage to the cochlear hair cells may lead to deafness. All children who have had meningitis should have an audiological assessment promptly, as children who become deaf may benefit from hearing amplification or a cochlear implant. • Local vasculitis. This may lead to cranial nerve palsies or other focal lesions. • Local cerebral infarction. This may result in focal or multifocal seizures, which may subsequently lead to epilepsy. • Subdural effusion. Particularly associated with Haemophilus influenzae and pneumococcal meningitis. This is confirmed by CT scan. Most resolve spontaneously but may require prolonged antibiotic treatment. • Hydrocephalus. May result from impaired resorption of CSF (communicating hydrocephalus) or blockage of the ventricular outlets by fibrin (non-communicating hydrocephalus). A ventricular shunt may be required. • Cerebral abscess. The child’s clinical condition deteriorates with the emergence of signs of a space-occupying lesion. The temperature will continue to fluctuate. It is confirmed on CT scan. Drainage of the abscess is required. • Direct invasion of the cerebrum by a neurotoxic virus (such as herpes simplex virus, HSV) • Delayed brain swelling following a disordered neuroimmunological response to an antigen, usually a virus (post-infectious encephalopathy), e.g. following chickenpox • A slow virus infection, such as HIV infection or subacute sclerosing panencephalitis (SSPE) following measles. The clinical features and investigation of encephalitis are described in Figure 14.4. Most children present with fever, altered consciousness and often seizures. Initially, it may not be possible to clinically differentiate encephalitis from meningitis, and treatment for both should be started. The underlying causative organism is only detected in 50% of cases. In the UK, the most frequent causes of encephalitis are enteroviruses, respiratory viruses and herpesviruses (e.g. herpes simplex virus, varicella and HHV6). Worldwide, microorganisms causing encephalitis include Mycoplasma, Borrelia burgdorferi (Lyme disease), Bartonella henselae (cat scratch disease), rickettsial infections (e.g. Rocky Mountain spotted fever) and the arboviruses. Herpes simplex virus (HSV) is a rare cause of childhood encephalitis but it may have devastating long-term consequences. All children with encephalitis should therefore be treated initially with high-dose intravenous aciclovir, since this is a very safe treatment. Most affected children do not have outward signs of herpes infection, such as cold sores, gingivostomatitis or skin lesions. The PCR of the CSF may be positive for HSV. As HSV encephalitis is a destructive infection, the EEG and CT/MRI scan may show focal changes, particularly within the temporal lobes (Fig. 14.5). These tests may be normal initially and need to be repeated after a few days if the child is not improving. Later confirmation of the diagnosis may be made from HSV antibody production in the CSF. Proven cases of HSV encephalitis or cases where there is a high index of suspicion should be treated with intravenous aciclovir for 3 weeks, as relapses may occur after shorter courses. Untreated, the mortality rate from HSV encephalitis is over 70% and survivors usually have severe neurological sequelae. Meningococcal infection is a disease that strikes fear into both parents and doctors, as it can kill previously healthy children within hours (Case History 14.1). However, of the three main causes of bacterial meningitis, meningococcal has the lowest risk of long-term neurological sequelae, with most survivors recovering fully. The septicaemia is usually accompanied by a purpuric rash which may start anywhere on the body and then spread. The rash may or may not be present with meningococcal meningitis. Characteristic lesions are non-blanching on palpation, irregular in size and outline and have a necrotic centre (Fig. 14.8a,b). Any febrile child who develops a purpuric rash should be treated immediately, at home or in the general practitioner’s surgery, with systemic antibiotics such as penicillin before urgent admission to hospital. Although there are now polysaccharide conjugate vaccines against groups A and C meningococcus, there is still no effective vaccine for group B meningococcus, which accounts for the majority of isolates in the UK. This is a localised, highly contagious, staphylococcal and/or streptococcal skin infection, most common in infants and young children. It is more common where there is pre-existing skin disease, e.g. atopic eczema. Lesions are usually on the face, neck and hands and begin as erythematous macules which may become vesicular/pustular or even bullous (Fig. 14.9). Rupture of the vesicles with exudation of fluid leads to the characteristic confluent honey-coloured crusted lesions. Infection is readily spread to adjacent areas and other parts of the body by autoinoculation of the infected exudate. Topical antibiotics (e.g. mupirocin) are sometimes effective for mild cases. Narrow-spectrum systemic antibiotics (e.g. flucloxacillin) are needed for more severe infections, although more broad-spectrum antibiotics such as co-amoxiclav or cefaclor have simpler oral administration regimens, taste better and therefore have better adherence. Affected children should not go to nursery or school until the lesions are dry. Nasal carriage is an important source of infection which can be eradicated with a nasal cream containing mupirocin or chlorhexidine and neomycin. In periorbital cellulitis there is fever with erythema, tenderness and oedema of the eyelid (Fig. 14.10). It is almost always unilateral. In young, unimmunised children it may also be caused by Haemophilus influenzae type b which may also be accompanied by infection at other sites, e.g. meningitis. It may follow local trauma to the skin. In older children, it may spread from a paranasal sinus infection or dental abscess. Periorbital cellulitis should be treated promptly with intravenous antibiotics to prevent posterior spread of the infection to become an orbital cellulitis. In orbital cellulitis, there is proptosis, painful or limited ocular movement and reduced visual acuity. It may be complicated by abscess formation, meningitis or cavernous sinus thrombosis. Where orbital cellulitis is suspected, a CT scan should be performed to assess the posterior spread of infection and a lumbar puncture may be required to exclude meningitis. This is caused by an exfoliative staphylococcal toxin which causes separation of the epidermal skin through the granular cell layers. It affects infants and young children, who develop fever and malaise and may have a purulent, crusting, localised infection around the eyes, nose and mouth with subsequent widespread erythema and tenderness of the skin. Areas of epidermis separate on gentle pressure (Nikolsky sign), leaving denuded areas of skin (Fig. 14.11), which subsequently dry and heal without scarring. Management is with an intravenous anti-staphylococcal antibiotic, analgesia and monitoring of fluid balance. Many of the common childhood infections present with fever and a rash (Table 14.2). Incubation periods vary from 24 h for viral gastroenteritis, to about 2 weeks for chickenpox, but for some diseases, such as HIV, the length of time between exposure and the development of symptomatic illness may extend to many years. This is a reflection of host–pathogen interactions; an effective initial host response may result in a prolonged period of clinical latency, whereas an ineffective response permits rapid evolution of disease. Table 14.2
Infection and immunity
The febrile child
Clinical features
(i) How is fever identified in children?
(ii) How old is the child?
(iii) Are there risk factors for infection?
(vi) Is there a focus for infection?
Management
Serious life-threatening infections
Septicaemia
Meningitis
Bacterial meningitis
Organisms
Neonatal–3 months
Group B streptococcus
E. coli and other coliforms
Listeria monocytogenes
1 month–6 years
Neisseria meningitidis
Streptococcus pneumoniae
Haemophilus influenzae
>6 years
Neisseria meningitidis
Streptococcus pneumoniae
Presentation
Investigations
Cerebral complications
Encephalitis/encephalopathy
Specific bacterial infections
Meningococcal infection
Staphylococcal and group A streptococcal infections
Impetigo
Periorbital cellulitis
Scalded skin syndrome

Common viral infections
Maculopapular rash
Viral
HHV6 or 7 ( Roseola infantum) – <2 years old
Enteroviral rash
Parvovirus (‘slapped cheek’) – usually school-age
Measles – uncommon if immunised
Rubella – uncommon if immunised
Bacterial
Scarlet fever (group A streptococcus)
Erythema marginatum – rheumatic fever
Salmonella typhi (typhoid fever) – classically rose spots
Lyme disease – erythema migrans
Other
Kawasaki disease
Juvenile idiopathic arthritis
Vesicular, bullous, pustular
Viral
Varicella-zoster virus – chickenpox, shingles
Herpes simplex virus
Coxsackie – hand, foot and mouth
Bacterial
Impetigo – characteristic crusting
Boils – infection of hair follicles/sweat glands
Staphylococcal bullous impetigo
Staphylococcal scalded skin
Toxic epidermal necrolysis
Other
Erythema multiforme; Stevens–Johnson syndrome
Petechial, purpuric
Bacterial
Meningococcal, other bacterial sepsis
Infective endocarditis
Viral
Enterovirus and other viral infections
Other
Henoch–Schönlein purpura (HSP)
Thrombocytopenia
Vasculitis
Malaria ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Infection and immunity