Fig. 32.1
This segmental tibia fracture in an adolescent was treated with casting and went onto malunion. The patient subsequently developed knee and ankle osteoarthritis
What Is Acceptable Alignment?
There has been an evolution in what constitutes acceptable alignment among our peers. Through the 1990s all focus was on achieving union with the following alignment dogma: less than 10° of angular deformity and less than 2 cm of shortening were well tolerated [1, 2]. Sarmiento stated, “We accept minor losses in length and alignment as small sacrifices in an effort to provide early function and decreased morbidity.” Changes in stress patterns at the tibiotalar joint are not significant with angular deformities less than 10° in any plane. In over 25 years of observation small amounts of shortening and angulation have not been associated with osteoarthritis or diminished function at a later date and are cosmetically acceptable to the patient [3]. Many patients were left with large rotation deformities of the femur and tibia, bone shortening, or angular and translational deformities (Fig. 32.2). Surgeons have moved toward more stringent criteria with less than 5° of angular deformity considered ideal [4–6]. The adoption of intramedullary nailing and marginalization of casting as a standard of care for adult tibia fractures has given surgeons the ability to obtain more accurate fracture reductions [7]. Similarly, the management of pediatric femur fractures has moved toward surgery making traction and casting less popular [8] (Fig. 32.3).



Fig. 32.2
This distal tibial fracture was sustained during adolescence and was treated with casting. The angulation of 10° was accepted and the fracture healed uneventfully. The patient developed ankle arthritis years later with more joint space narrowing seen in the medial aspect of the tibiotalar joint

Fig. 32.3
This fracture was treated in adolescence with traction and casting resulting in 16° of varus and 3 cm of shortening
What Are the Consequences of Malalignment?
It is not uncommon to see adult patients with childhood deformities present to the office with knee or ankle arthritis secondary to the long-standing malalignment. This poor alignment places abnormal or asymmetric stress across the adjacent joint(s) leading to premature cartilage breakdown [7–10]. This contention is supported by Vallier et al. who found that a tibial malunion of more than 5° was significantly associated with knee and ankle pain [4]. Palmu found that the treatment of femur fractures in children older than 10 years with traction led to a high incidence of deformities greater than 10° that he later correlated with the development of knee arthritis at a young age [8] (Fig. 32.4). We should strive to reestablish these normal parameters for bone alignment to avoid abnormal limb mechanics. This will help to prevent articular cartilage wear and pelvic and low back problems, and facilitate joint replacement, if and when needed. More importantly, if initial treatment results in unacceptable alignment then we are obligated to consider the long-term implications for this patient and suggest further surgical correction for this patient. If the surgeon is not comfortable performing this “residual correction” then the patient should be referred to a specialized center. Many patients will elect no further treatment or may not be candidates for further intervention, but the malalignment needs to be acknowledged.


Fig. 32.4
This varus femur malunion resulted in malalignment that developed medial compartment osteoarthritis years after the injury
What Are the Legal Implications of Iatrogenic Deformities?
Nearly 15 % of orthopedic surgeons face a malpractice claim annually [11]. Restricting the criteria for acceptable deformity is analogous to “narrowing the strike zone.” This places increased responsibility on the surgeon to have a “perfect” result, thus making our job more difficult. If a malunion is a failure and the criteria for malunion are now broadened then there are legal implications. Patients are glad to have their concerns about their deformity legitimized, but their next question is why the deformity occurred and whether this was malpractice. Based on our experience, in most cases, the best policy is to concede that the result is not ideal, reassure that every effort was made to provide an optimal result and that there was no medical negligence, and counsel that further surgery to deliver a superior outcome is recommended. The greatest predictor of payment to a plaintiff is the severity of the patient’s disability [12]. This implies that the best course of action is to do everything possible to improve their condition and decrease disability. At no time should the surgeon abandon or blame the patient. A good doctor-patient relationship and better preoperative discussions of known complications will help to calm the impulse to bring legal action against the physician [13, 14]. Contact the hospital legal department and identify this patient as “at risk” for litigation. The hospital will often have patient services mitigate any feelings of discontent or help finance further treatment. When a patient does seek legal action, an angry patient will be less likely to settle the case. So, one must do as much as possible to avoid a hostile relationship with the patient and his or her caretakers. One must keep in mind that we are judged not only by our successes but also by how we handle adversity. These difficult situations are hurdles along the career path of every orthopedic surgeon.
Common Iatrogenic Deformities
Tibia Malunion
The immature skeleton’s ability to remodel a “malunion” is determined by the number of years of growth remaining. If the remodeling potential of an angulated bone is limited, then the fracture is considered a malunion and warrants intervention. If a child of advanced age presents with a displaced long bone fracture of the lower extremity that will likely go on to a malunion (impending malunion) if treated with cast immobilization, the surgeon will often select operative treatment to help ensure acceptable alignment at skeletal maturity. The current criteria for “acceptable” alignment in pediatric fractures fall into two groups. Children 8 years old or less often remodel angular deformities of up to 10°. In children older than eight and in adolescents, angular deformity of up to 5°, 1 cm of shortening, and less than 10° of rotational deformity is acceptable [15]. Most remodeling occurs within 2 years after fracture healing [15]. Due in part to a robust periosteum and rapid healing, most tibia fractures in children can be treated with casting while still maintaining acceptable alignment, length, and rotation [16]. However certain fractures are difficult to manage in a cast or are at high risk for displacement and malunion and are often treated surgically: high-energy unstable fractures, open fractures, fractures with soft tissue injury or compartment syndrome, oblique fractures with an intact fibula, floating knee, and fractures in older children [16–19]. Operative management of tibia factures is most commonly performed with elastic titanium intramedullary (IM) nails [20]. Circular external fixation has been shown to be superior to monolateral fixation for unstable diaphyseal fractures of the tibia in children and adolescents and is gaining popularity [21]. Circular fixation may also be equivalent to elastic IM nailing in adolescents [22]. External fixation may be superior to casting as it allows for ease of monitoring and management of compartment syndrome, which remains one of the most common complications of pediatric tibia fractures [23, 24]. Use of the programmable, six-axis circular fixator in high-energy pediatric tibia fractures has proved successful affording very accurate alignment and early weight bearing [25, 26]. However, the use of external fixation is associated with a small incidence of refracture and fracture through the pin sites [27].
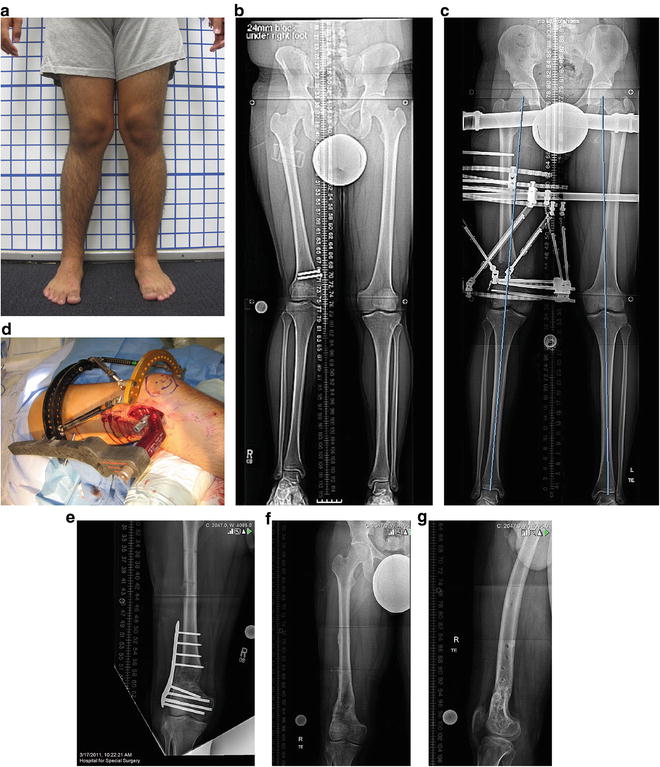
Case 1
A 12-year-old male presented with a noticeable deformity of the lower leg including varus, external rotation, and shortening. He had sustained a Salter–Harris type II fracture of the distal tibia at the age of 8 years. A metaphyseal osteotomy was performed for deformity correction and was stabilized with a plate and screws. The growth plate became tethered medially driving the epiphysis into varus and slowing the growth of the entire physis (Fig. 32.5a, b). This was recognized by his orthopedist who had been following him yearly after the injury. He was referred for deformity correction and limb lengthening. The sum of these deformities led to significant functional problems with walking and running and put him at increased risk for developing arthritis of the ankle and low back pain. He was noted to have limited ankle dorsiflexion of the injured side compared with the unaffected left ankle. His external rotation deformity of the tibia was 20°. He had a 2.5-cm shortening of the tibia. Surgical planning included calculation of the future shortening that would result from formal closure of the distal tibial physis. Correction with the six-axis circular fixator was considered a good option. This would allow for deformity correction and lengthening. The entire distal tibial growth plate was closed surgically. A distal metaphyseal osteotomy was created with an osteotome to allow for gradual correction of the varus and rotational deformities. Lengthening through the same osteotomy site has two disadvantages: the patient may develop a significant equinus, and the time to consolidation of the lengthening regenerate would be lengthy. To address these potential problems a second more proximal osteotomy was performed for the lengthening (see Fig. 32.5c, d). The final result was correction of the deformities including length with a full functional recovery (see Fig. 32.5e–g) He had a contracture of the gastrocnemius that fully resolved with physical therapy 6 months after frame removal. Another option would have been to lengthen the gastrocnemius muscle tendon for a more rapid recovery of ankle motion.
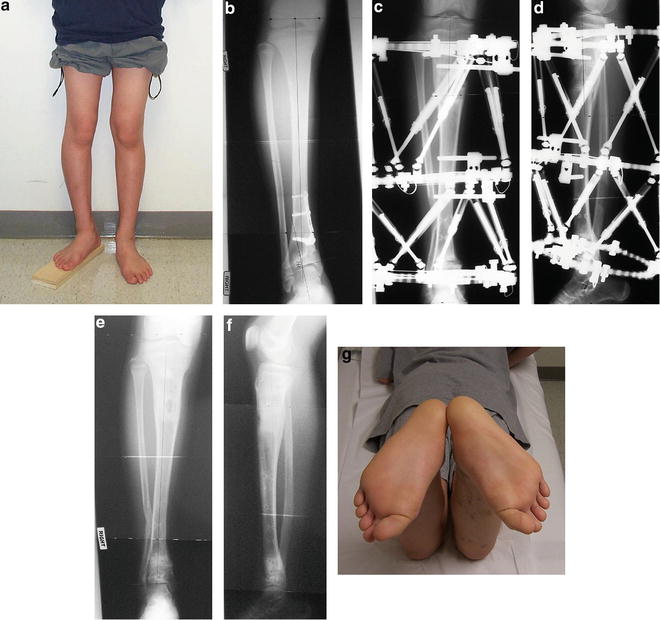
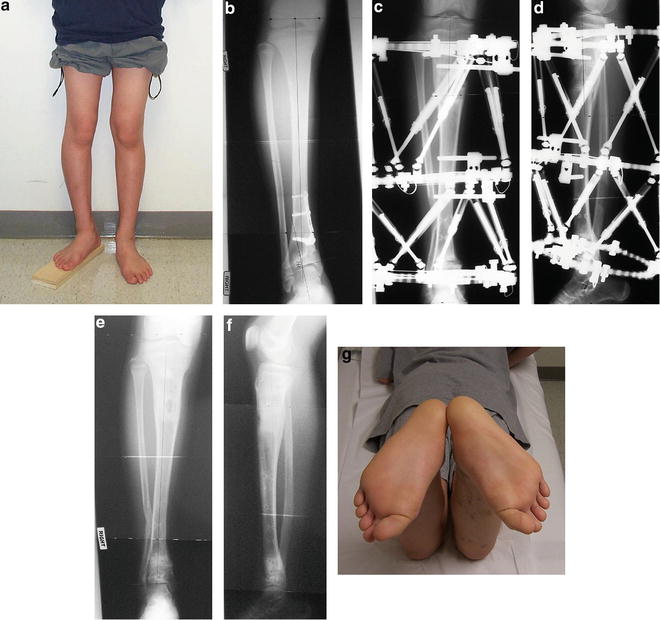
Fig. 32.5
(a) This patient has a malunion with shortening, external rotation, and varus. (b) AP X-ray shows retained hardware, medial physeal tethering, and distal varus deformity. (c, d) AP and lateral radiographs during treatment demonstrating the two-level osteotomy and double-level circular fixation for deformity correction and lengthening. (e, f) These X-rays show healing of both osteotomies with accurate correction of the underlying deformities. (g) Restoration of the axial alignment of the tibia is assessed with the prone exam
Case 2
A high-energy closed tibia fracture in a 13-year-old male was treated with a monolateral pin-to-bar external fixation as the definitive stabilization. The reduction resulted in 2 cm of lateral translation of the distal fragment and 10° of apex anterior angular deformity (Fig. 32.6a, b) The surgeon explained that this was acceptable alignment and that he was unable to improve it with closed reduction; because the deformity was acceptable open reduction was not indicated. The family sought a second opinion. This sagittal plane deformity is greater than 5° and will likely not remodel in this adolescent patient. The clinical concern about residual apex anterior deformity of the tibial shaft is that it may create abnormal wear on the knee and ankle joints, increases stress on the anterior cruciate ligament (ACL), and prevents full leg extension. Trepidations about the fixation construct included further loss of reduction, impending malunion, and even possible nonunion. Treatment with a six-axis circular fixator using the Taylor Spatial Frame (TSF) (Smith & Nephew, Memphis, TN) was provided. This device allowed for a percutaneous surgery, an accurate and gradual correction of the residual deformity, avoidance of the growth plates, and weight bearing as tolerated ambulation during the entire treatment period (see Fig. 32.6c–e) After 3 months of wearing the external fixator, the final result was a near-anatomic bony alignment and no functional impairment (see Fig. 32.6f, g).
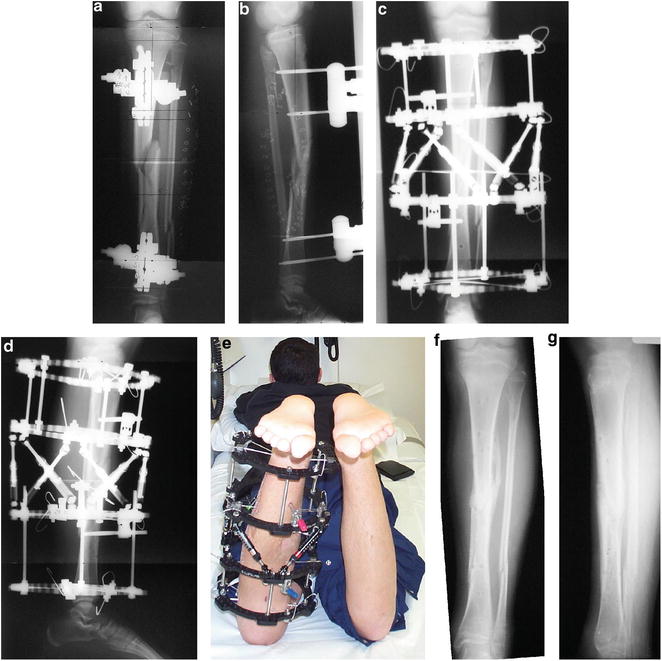
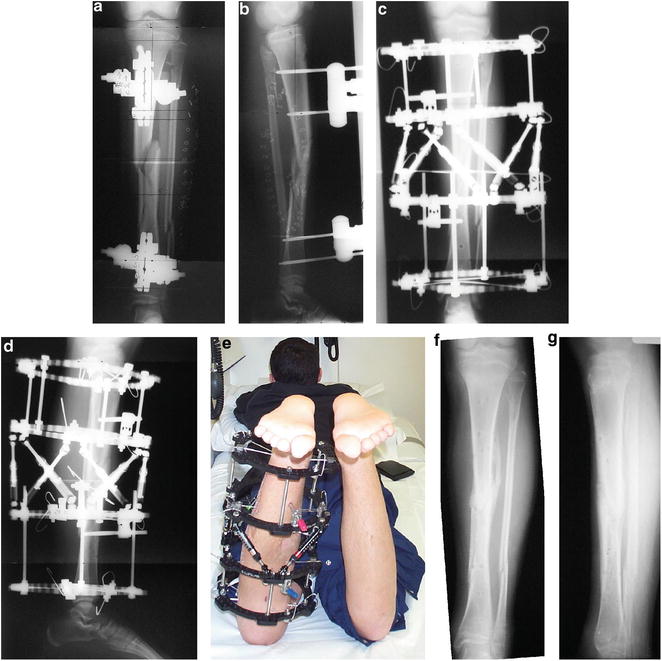
Fig. 32.6
(a, b) AP and lateral radiographs show a high-energy tibial fracture treated with temporizing external fixation. Soft-tissue swelling and damage made internal fixation a poor option. (c, d) The circular external fixator provided superior stability and allowed for early weight bearing. (e) The prone exam is important to confirm that axial alignment has been restored. (f, g) The final result is a healed fracture with excellent alignment
Fibular Malunion
Fibular fractures in children and adolescents commonly heal without incident. In rare circumstances growth arrest of the distal fibular physis can occur causing progressive fibular shortening. This leads to valgus orientation of the hindfoot, widening of the syndesmosis, and early ankle joint degeneration [28–33]. Once recognized, this fibular shortening and syndesmotic laxity can be corrected surgically [34–36]. Manoudis et al. reported a case of fibular shortening from physeal arrest corrected by open osteotomy, acute lengthening, grafting with tricortical iliac crest, and internal fixation [37]. An open release of the syndesmosis was necessary to reduce the fibular tip into its proper location. Other authors have reported on the same technique without the need for syndesmotic dissection [29]. Alternatively, a percutaneous technique can be employed to both lengthen the fibula through distraction osteogenesis and utilize distraction histiogenesis to stretch the syndesmotic ligaments and achieve distal migration of the fibular tip.
Case 3
A 13-year-old female presented with a valgus deformity of the hindfoot after premature fibular physeal closure. The patient had previously undergone curettage of a benign distal fibular bone cyst (without apparent physeal involvement) with prophylactic plating to prevent fracture of the distal fibula. The hardware was removed 1 year later without incident. The distal fibular physis closed prematurely postoperatively leading to a shortening deformity of the fibula over time. The etiology of the physeal injury is not clear but an iatrogenic cause could not be excluded. The patient’s hindfoot drifted into valgus when compared with the other side. Radiographs revealed a shortened fibula with a distal physeal closure. X-rays of the contralateral ankle were taken to establish the normal fibular length and talocrural angle (Fig. 32.7a, b). This deformity was unacceptable as it would lead to asymmetric wear of the lateral talus and possibly arthritis. Fibular shortening of 1.5 cm was measured. The treatment plan included lengthening of the fibula. The tibia was included in the proximal fibular ring block to protect the proximal tibiofibular joint from subluxation and ensure distal migration and reduction of the fibular tip (see Fig. 32.7c, d). The fibula was lengthened with the external fixator. When the correct length was obtained the patient was brought back to the operating room for insertion of syndesmotic screws and early removal of the frame (see Fig. 32.7e). The patient’s hindfoot alignment was corrected with no loss of ankle motion (see Fig. 32.7f).
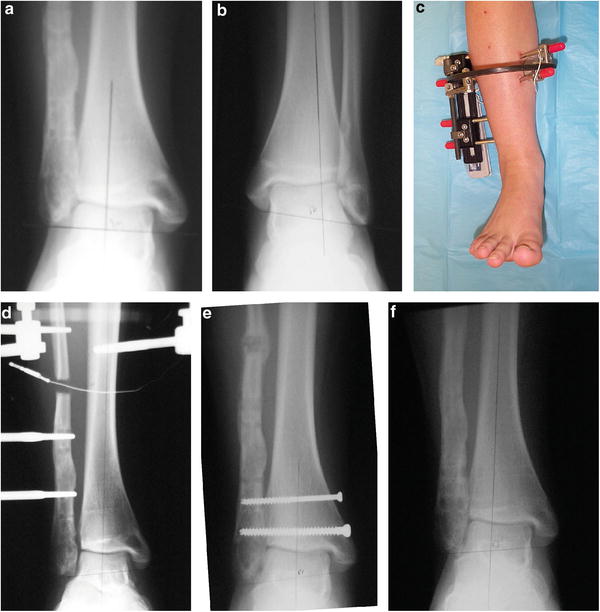
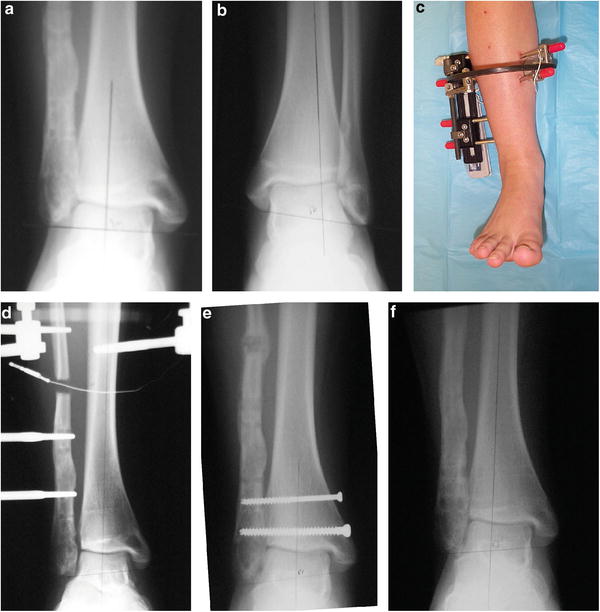
Fig. 32.7
(a, b) AP radiographs of the shortened right fibula and the normal left fibula. Tibial alignment is within normal. (c, d) An external fixator was used to lengthen the fibula using half pins. (e) At the time of frame removal the syndesmosis was stabilized with two screws. (f) Final radiographs show restoration of the length of the fibula and removal of the screws
Transphyseal ACL Reconstruction Causes Premature Physeal Closure
An option for ACL reconstruction in older children (age 11–14 years) is the transphyseal tunnel technique. Most authors report minimal complications with this method including an average growth plate disturbance risk of 3 % [38–44]. Kumar et al. reported on 32 children with an average age of 11.25 years where the transphyseal reconstruction was used with one case of mild valgus and no leg length discrepancy [38]. Similarly, transphyseal surgery in a series of 15 patients, average age 12.8 years, resulted in one case of valgus malalignment of the knee [39]. Asymmetric growth of the distal femoral physis is the most commonly reported mechanism for the valgus deformity [41]. Other series report no adverse trauma to the physis with this technique, but authors caution to make sure that the graft bone blocks are not in contact with the physis [42–44]. Physeal sparing reconstruction carries minimal risk to the growth plate but may not be as reliable with regard to maintenance of ligamentous stability of the knee [45]. Although the risk of growth plate disturbance around the knee is small, its occurrence in some cases is undeniable and such iatrogenic angular deformities may require surgical correction.
Case 4
A 15-year-old male presented with a deformity of the proximal tibia including varus, recurvatum, and shortening. At age 12 he sustained an ACL injury. The ACL was reconstructed using the transphyseal technique in the tibia and an over-the-top technique in the femur. The anterior-medial proximal tibial physis was likely damaged. A progressive angular deformity developed with significant retardation of physeal growth (Fig. 32.8a–c). The radiologic deformities included 15° of varus, 28° of apex posterior (recurvatum), and 4.5 cm of shortening. The clinical deformity included 10° of hyperextension of the knee and normal knee ligamentous stability. Growth remaining discrepancy was calculated to be an additional 1 cm. Treatment was closure of the remainder of the proximal tibial physis to prevent further deformity, proximal tibial osteotomy, and TSF application for deformity correction and lengthening (see Fig. 32.8d, e). The latest follow-up at 12 months post-frame removal shows restoration of length and alignment, and a full functional recovery is expected (see Fig. 32.8f–h).
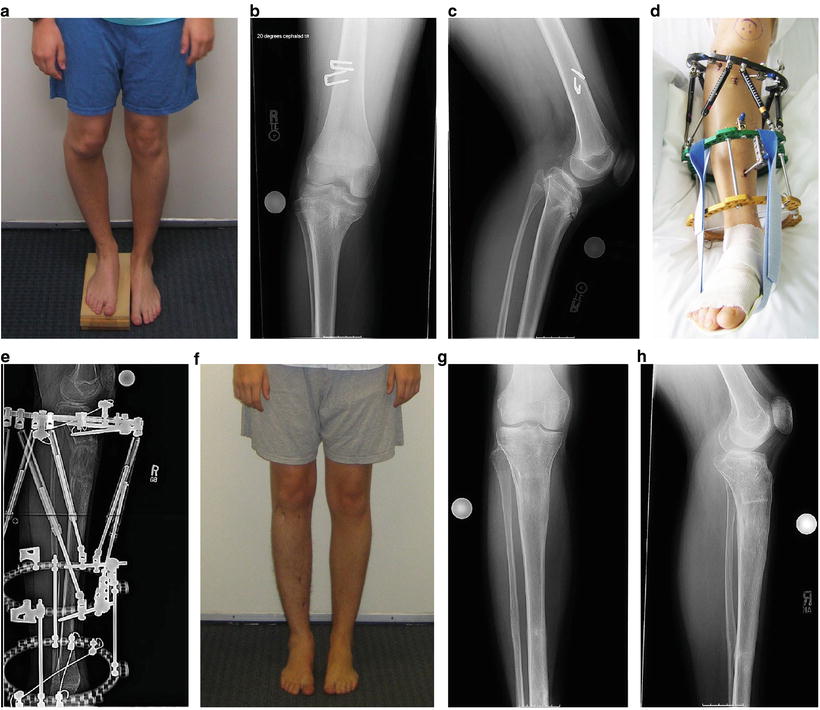
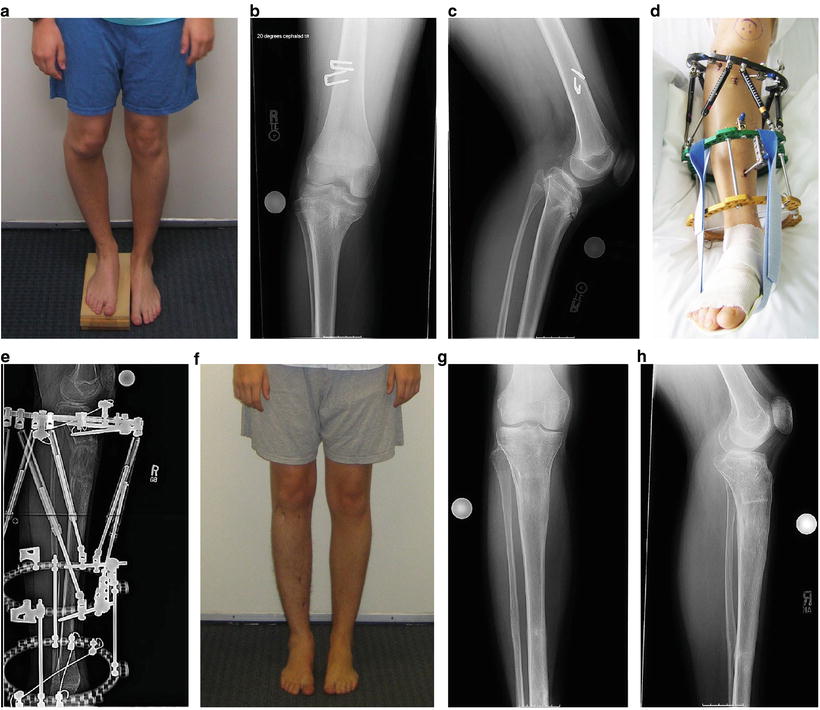
Fig. 32.8
(a) This clinical photo shows a proximal tibial deformity with shortening, varus, and malrotation. (b, c) AP and lateral X-rays show varus and recurvatum angulation with closure of the anteromedial physis. (d, e) This photo shows the early postoperative external fixator mimicking the deformity. The radiograph was taken near the end of the correction showing the proximal tibial lengthening. (f–h) Final clinical photo and radiographs demonstrate full correction of the deformity
Femur Malunion and Growth Disturbance
Distal femur physeal fractures are afflicted by a high rate of physeal arrest and subsequent deformity [46]. Displaced fractures and Salter–Harris II injuries are predictors of a poor outcome with a 40 % risk of physeal bar formation [47]. Surgical reduction and fixation are recommended, and smooth Steinman pins crossing the physis do not seem to further increase the already high risk of physeal arrest [46, 48].
Distal femur malunion without growth plate arrest is another complication of pediatric femur fractures. Although the skeletally immature femur has a tremendous remodeling potential, angulation and shortening may not be tolerated as well as many surgeons believe. In children over 10 years old varus-valgus angulation of greater than 5° and procurvatum-recurvatum of greater than 10° should not be accepted because such deformities can be associated with premature knee arthritis [8].
Treatment of diaphyseal and distal femoral deformities that occur during childhood and subsequently present in adulthood can be accomplished with various implants including IM nail, plate and screws, and external fixation. The challenge is managing the femoral shortening that is often present in these individuals. External fixation allows for deformity correction and lengthening simultaneously [49]. Integrated fixation techniques provide the best of both devices using external fixation to achieve length and deformity correction and then converting to internal fixation while the immature bone consolidates [50–52]. The newer internal lengthening nails provide an all-internal correction of deformity and bone lengthening solution [53].
Case 5
A 19-year-old male presented with femoral valgus and shortening. He had been struck by a vehicle when he was 11 years old sustaining a distal femur physeal fracture. The fracture was stabilized with internal fixation. It is not known whether the fracture was reduced anatomically or was stabilized with residual valgus angulation. If the initial postoperative alignment was appropriate then this may not qualify as an iatrogenic deformity. He was an avid soccer player but was having increasing difficulty playing due to the lower limb deformity and knee pain. Partial closure of the lateral distal femoral physis caused a valgus deformity and 3 cm of shortening (Fig. 32.9a, b). The patient was at risk for knee arthritis, hip, and low back problems. The proposed treatment would address both the valgus deformity and the femur shortening. A distal osteotomy with lengthening is best done with a circular fixator, but the frame would need to be on the leg for a long time and femoral rings are very uncomfortable. The LAP (lengthening and plating) technique was selected. A femoral osteotomy was created and stabilized with a TSF (see Fig. 32.9c). The correction was performed gradually with lengthening. Once the acceptable length and alignment were reached, the patient was brought back to surgery for insertion of a plate and screws and removal of the frame (see Fig. 32.9d, e). The femur healed and the plate was later removed (see Fig. 32.9f, g). He returned to play soccer without any limitations.