Fig. 5.1
Examination trolley & range of equipment. Examination trolley showing from left to right: a tray with 0.1 % chlorhexidine cleaning fluid, a cusco speculum and lubricating jelly; sponge forceps, Uterine sound, 5Fr balloon HSG catheter, Margolin acorn catheter, Goldstein HyCoSy catheter, 4Fr vessel dilator, Rocket 27 mm suction cup, 21 g plastic venous cannula and 10 cc syringe with contrast medium
The tip of the catheter is placed in the high cervical canal and once the chosen catheter is securely placed, if possible, the speculum is removed, however if visualization of the cervix has been difficult or to remove the speculum may dislodge the catheter then it is left in situ.
Before any contrast is introduced into the uterine cavity the radiologist should review the pelvic cavity fluoroscopically for radio-opaque densities such as calcified fibroids, dermoid cysts or surgical clips and, if indicated, take a control image. A radio-opaque side marker is placed on the image intensifier.
Non-ionic iodinated water-soluble radiographic contrast medium (Omnipaque 300) is infused slowly and gently by hand injection into the uterine cavity under intermittent fluoroscopic control. It is crucial to infuse the contrast slowly in order to minimize discomfort. Forcible or rapid infusion causes significant pain, which in turn may limit the investigation and cause tubal spasm. Mechanical injection devices should not be used.
An early filling image of the uterine cavity is taken to visualize small intrauterine filling defects, such as polyps or fibroids, which may be obscured by contrast medium in later images. This is followed by right and left anterior oblique images to demonstrate the uterine cavity and the fallopian tubes throughout their length. These images may be acquired by either turning the patient and/or utilizing the rotational capability of the image intensifier. A fourth image is obtained in the frontal projection to show intra-peritoneal spill from the fallopian tubes. It is essential to obtain at least one true en-face image of the uterine cavity (Fig. 5.2) if significant pathology is not to be missed, this may require gentle traction or upward pressure on the cannula combined with patient rotation and/or angulation of the image intensifier. These 4 images are the minimum required – it may be necessary to acquire more and the examination can be supplemented by fluoroscopic grab images. Tilting the patient head down on the examination couch, rotating the patient through 360 degrees and taking delayed images may also be necessary to adequately demonstrate the fallopian tubes [5, 9].


Fig. 5.2
Normal HSG enface view. A normal HSG showing the cervical canal, uterine cavity en-face and both fallopian tubes with free intraperitoneal spill. U0 C0 V0
Usually a maximum 10 cc contrast medium is sufficient to demonstrate the cavity and tubes but in a very enlarged cavity up to 50 cc may be required.
If the catheter has been introduced into the lower segment of the uterine cavity it is essential that any balloon is deflated and the catheter is withdrawn whilst continuing to infuse contrast medium under fluoroscopic control at the end of the procedure in order to adequately visualize the lower uterine segment and upper cervical canal (Fig. 5.3a, b). Hoffmann [10] observed that common causes for misdiagnosis in HSG include failure to obtain an en-face view, failure to deflate an intra-uterine balloon and failure remove a speculum obscuring the cervical canal.
Fig. 5.3
Balloon in LUS inflated & deflated. (a) HSG showing a balloon catheter inflated in the lower uterine segment (LUS). (b) The same patient following deflation of the balloon and a normal LUS. U0 C0 V0
In our unit we employ a Siemens Axiom Artis C arm x-ray machine. As in all investigations involving ionising radiation it is essential to keep the dose to the patient as low as practicable. In our department the mean screening time is 1 s and the DAP (dose area product) is 0.48 Gy cm2. The national DRL (dose reference level) for HSG is 2 Gy cm2 & 0.7 min (42 s) [11].
Complications [6, 9]
As with any procedure HSGs may be associated with complications, these can be minimized by good technique and observance of the contraindications.
Complications of Hysterosalpingography
Infection
Pain
Intravasation
Pregnancy irradiation
Failure
Vasovagal episode
Contrast medium allergic reaction
A significant complication of HSG is pelvic infection, which is reported to occur in between 1 and 3 % of all cases and up to 10 % in the presence of tubal pathology [12–14]. In women with a medical history of pelvic infection the risk of infection is reduced by the use of prophylactic antibiotics [7, 13]. Whilst some centres routinely screen all women for Chlamydia prior to HSG some authors advocate prophylactic antibiotics in all women before uterine instrumentation without preliminary screening [15]. The author’s practice is to administer 1 g of Azithromycin immediately prior to the procedure. It is impossible to completely exclude the risk of infection. Aseptic technique, prophylactic antibiotics, additional antibiotic therapy in the presence of hydrosalpinges and the avoidance of undertaking an HSG in the presence of active or recent PID (pelvic inflammatory disease) will help minimize the incidence.
An HSG is an invasive and intimate examination however by paying attention to the environment, establishing a rapport with the patient and with experience and good technique the patient may experience mild discomfort but it should rarely be a painful examination. We do not advise the use of analgesia before the procedure as this increases the expectation, and therefore the experience, of pain. Patients are advised that they may experience some discomfort post procedure and to take analgesia if necessary.
Intravasation is usually indicative of uterine pathology. If it occurs it is of no clinical significance but may limit the study as it may not be possible to accurately identify the fallopian tubes (Fig. 5.4a, b) [7].
Fig. 5.4
Intravasation; HSG a woman who suffered a miscarriage and has undergone an ERPC. (a) The study reveals a uterine cavity that has an arcuate configuration, evidence of intra-uterine synechiae in the left fundal and cornual region and early venous intravasation. (b) A later image shows extensive venous intravasation
Irradiation of an early pregnancy is avoided by abstinence from intercourse from the first day of the menstrual cycle and until after the HSG has been performed and by performing a urine ß hCG pregnancy test on the day of the examination.
Failure to perform an HSG is usually due to severe vaginismus and consideration should be given to mild sedation if this occurs.
Vasovagal episodes are usually mild but may, on occasion, be severe and can occur at any stage during the procedure. Good technique dramatically reduces the incidence of vasovagal reactions. Conservative treatment is usually all that is required, tilt the head of the examination couch down (Trendelenberg position), reassure the patient, provide ice-cold water to drink and allow the patient to rest until recovered. Rarely the reaction may be more severe and warrant intravenous fluids and/or atropine.
Allergic reactions following the use of water-soluble contrast agents for HSG are rare. The authors would not undertake an HSG in someone with history of a previous severe reaction to iodinated contrast medium as an HSG is an elective procedure and the information required can be obtained in other ways if necessary for example by HyCoSy, MRI, or hysteroscopy.
Hysterosalpingographic Demonstration of Female Genital Tract Anomalies
In the evaluation of congenital anomalies HSG is complementary but it cannot be wholly diagnostic. The HSG demonstrates the uterine cavity and fallopian tubes but it cannot accurately characterize the external contour of the uterus which is essential for the proper definition of FGTAs /Mullerian Duct Anomalies (MDA) [16, 17]. Accurate delineation and classification is essential for determining treatment and reproductive prognosis. 3D Ultrasound and MRI are the modalities of choice for full the anatomical evaluation of MDAs [18].
The HSG may be the first examination to detect a congenital anomaly. The HSG report should be descriptive. The radiologist may be able to suggest which ESHRE/ESGE [19] class any demonstrated anomaly falls into but cannot give a definitive answer and must therefore provide a differential diagnosis and suggest additional imaging such as MRI and/or 3D ultrasound for full characterisation of the abnormality [20]. For example the HSG cannot distinguish between a septate and a bicornuate (bicorporeal) uterine cavity and it cannot exclude a non-communicating rudimentary horn in a hemi or unicornuate uterus.
The HSG is useful in demonstrating concomitant pathology affecting the cavity and fallopian tubes including intrauterine synechiae, endometrial polyps, leiomyomata, salpingitis isthmica nodosa (SIN), tubal occlusive disease and hydrosalpinges. Demonstration of all relevant abnormalities is essential if fully informed consent is to be obtained preoperatively that allows the removal or correction of all pathology detected at surgery. Hysterosalpingography is also of significant value in post-operative assessment following surgical correction of operable congenital anomalies [21].
Normal Uterus, Cervix and Vagina (ESHRE/ESGE U0, C0 V0)
A normal HSG reveals a triangular shaped uterine cavity with the fundus representing the base of the triangle and the apex the lower segment extending into the endo-cervical canal. The walls of the cavity should be smooth, the filling pattern even and the fundal margin should be straight or showing minimal convexity or concavity. The fallopian tubes, which arise from the uterine cornu, are divided into four parts the short intramural portion, the long narrow isthmus, the wider ampulla with prominent mucosal folds and the infundibulum, a series of fimbriae, which radiate round the tubal ostium (Figs. 5.2, 5.3 and 5.5). Free intraperitoneal spill from the fallopian tubes disperses around bowel loops and may flow over the fundus indicating clearly the thickness of the myometrium (Fig. 5.6).
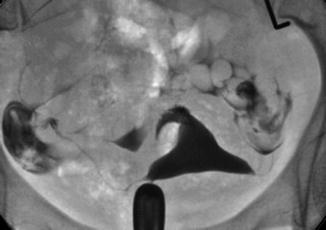
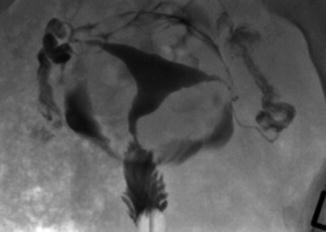
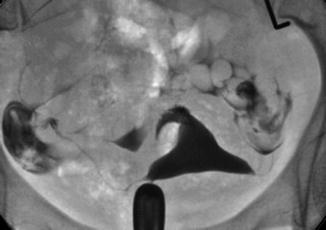
Fig. 5.5
Normal HSG. Enface view in steeply ante-verted uterine cavity U0 C0 V0
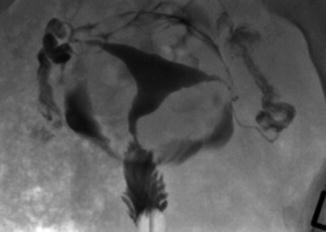
Fig. 5.6




Normal HSG demonstrating spill over the uterine fundus Intraperitoneal spill is seen arching over the uterine fundus demonstrating normal myometrial thickness U0 C0 V0
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


