Classification
Subheading
Subgroup
Category
I. Failure of formation
A. Transverse arrest
1. Shoulder
2. Arm
3. Elbow
4. Forearm
5. Wrist
6. Carpal
7. Metacarpal
8. Phalanx
B. Longitudinal arrest
1. Radial deficiency
2. Ulnar deficiency
3. Central deficiency
4. Intersegmental
Phocomelia
II. Failure of differentiation
A. Soft tissue
1. Disseminated
(a) Arthrogryposis
2. Shoulder
3. Elbow and forearm
4. Wrist and hand
(a) Cutaneous syndactyly
(b) Camptodactyly
(c) Thumb-in-palm
(d) Deviated/deformed digits
B. Skeletal
1. Shoulder
2. Elbow
Synostosis
3. Forearm
(a) Proximal
(b) Distal
4. Wrist and hand
(a) Osseous syndactyly
(b) Carpal bone synostosis
(c) Symphalangia
(d) Clinodactyly
C. Tumorous conditions
1. Hemangiotic
2. Lymphatic
3. Neurogenic
4. Connective tissue
5. Skeletal
III. Duplication
A. Whole limb
B. Humeral
C. Radial
D. Ulnar
1. Mirror hand
E. Digit
1. Polydactyly
(a) Radial (preaxial)
(b) Central
(c) Ulnar (postaxial)
IV. Overgrowth
A. Whole limb
B. Partial limb
C. Digit
1. Macrodactyly
V. Undergrowth
A. Whole limb
B. Whole hand
C. Metacarpal
D. Digit
1. Brachysyndactyly
2. Brachydactyly
VI. Constriction band syndrome
VII. Generalized skeletal abnormalities
While it is interesting to discuss how different upper extremity anomalies can fit in to certain classification systems, it should be stated that as the understanding of developmental biology improves, these systems will continue to evolve over time (Manske and Oberg 2009). A more recent scheme for classifying congenital hand anomalies, referred to as the Oberg, Manske, and Tonkin (OMT) system (Oberg et al. 2010; Tonkin et al. 2013), has proposed three distinct categories that distinguish malformations from those that represent deformities or dysplasia (Table 2). Ultimately, the hope is that by continuing to explore these developmental differences, the physician community may be able to offer better treatment protocols for a child with a specific deformity. Rather than delving into these categorical differences, the goal of this chapter is to develop an appreciation of the more common anomalies associated with both undergrowth and failures of formation in the upper extremity. To accomplish this, the focus will be on the clinical presentation, associated findings, and treatment considerations for these conditions.
Table 2
Oberg, Manske, and Tonkin (OMT) classification
1. Malformations |
A. Failure of axis formation/differentiation – entire upper limb |
1. Proximal-distal outgrowth |
Brachymelia with brachydactyly |
Symbrachydactyly |
Transverse deficiency |
Intersegmental deficiency |
2. Radial-ulnar (anteroposterior) axis |
Radial longitudinal deficiency |
Ulnar longitudinal deficiency |
Ulnar dimelia |
Radioulnar synostosis |
Humeroradial synostosis |
3. Dorsal-ventral axis |
Nail-patella syndrome |
B. Failure of axis formation/differentiation – hand plate |
1. Radial-ulnar (anteroposterior) axis |
Radial polydactyly |
Triphalangeal thumb |
Ulnar polydactyly |
2. Dorsal-ventral axis |
Dorsal dimelia (palmar nail) |
Hypoplastic/aplastic nail |
C. Failure of axis formation/differentiation – unspecified axis |
1. Soft tissue |
Syndactyly |
Camptodactyly |
2. Skeletal deficiency |
Brachydactyly |
Clinodactyly |
Kirner’s deformity |
Metacarpal and carpal synostoses |
3. Complex |
Cleft hand |
Synpolydactyly |
Apert hand |
2. Deformations |
A. Constriction ring sequence |
B. Arthrogryposis |
C. Trigger digits |
D. Not otherwise specified |
3. Dysplasias |
A. Hypertrophy |
1. Macrodactyly |
2. Upper limb |
3. Upper limb and macrodactyly |
B. Tumorous conditions |
An additional point to consider is that cleft hands, transverse deficiencies, and phocomelia are among the most obvious and disfiguring of all congenital anomalies. With the advent of advanced prenatal imaging, the accuracy in diagnosing congenital upper extremity anomalies in utero is improving. As such, parents may consult the orthopedic surgeon about these disorders in the prenatal period. For a source of guidance about these matters, Bae, et al. provide an excellent discussion about the current status of prenatal screening as well as ethical and treatment considerations involved with the implementation of this technology (Bae et al. 2009).
Hypoplasia
Hypoplasia is defined as a small or underdeveloped body part. In the upper extremity, any anatomic segment such as a digit, a hand, or even the entire arm may be considered hypoplastic when compared to its normal counterpart in the contralateral extremity. Despite its small size, a hypoplastic body part may well be very functional, and when possible, every effort should be attempted to preserve or augment these affected, yet functional units.
The exact incidence of hypoplasia in the upper extremity is difficult to determine because in many congenital anomalies that are encountered, a hypoplastic anatomic part can also be identified as a part of the main condition. However, if one considers isolated hypoplasia of a single upper extremity segment with no other associated musculoskeletal deficits, the condition represents about 8 % of all congenital upper extremity anomalies (Giele et al. 2001). Yet it is suspected that this number may be artificially small due to underreporting of hypoplasia when the upper extremity remains very functional.
The inheritance patterns of hypoplastic anomalies are thought to be sporadic in nature unless the condition is associated with a specific syndrome. For example, many children with Feingold syndrome (inherited as autosomal dominant) are found to have small second and fifth fingers as part of the disorder. Thumb hypoplasia, which is discussed in detail in another chapter, can be seen in association with Fanconi anemia, an autosomal recessive disorder. As such, if hypoplasia is seen in conjunction with anomalies, a formal genetic consultation is probably indicated, and additional diagnostic testing may be needed to rule out other organ system involvement.
The clinical presentation of a child with hypoplasia can be quite variable. Obvious size differences are usually easy to detect, but the best way to identify subtler forms is to directly measure the region of concern and compare it to the contralateral upper extremity. In these mild forms of hypoplasia, radiographs may aid in confirming the diagnosis. In addition to noting potential size differences, comparison radiographs can also show other anomalies such as missing carpal bones, carpal coalitions, and malformed phalanges. Additional testing modalities such as MRI and CT scanning are usually not necessary for diagnostic purposes.
Any treatment considerations for the patient with hypoplasia should focus on maximizing function of the involved extremity. Often, this will require following the patient for an extended period of time, before recommending any surgical interventions, in order to understand just how the child uses the extremity most efficiently. In addition to getting subjective input about hand usage from the family, occupational therapists can provide objective functional data by administering age-appropriate testing modalities and thus offer valuable insights during this process.
Most patients with mild hypoplasia are very high functioning and require no surgical treatment for the condition. These children may need to alter the manner in which a task needs to be performed; yet they adapt very well in most task-oriented situations. There are, however, a few instances where surgery can offer benefit to these patients. One example would be if a child has a small, floppy digit that gets “in the way” of gripping or pinching tasks. In this case, hand use is being compromised, and amputation of that digit should be considered. In contrast, a small, stable finger with good tendon function might be made more useful by bone lengthening (Arata et al. 2011), and reconstruction is the best surgical option for this particular digit. It is equally important that the patient’s family has a very clear understanding of the expected goals of any type of surgery. Maximizing the child’s use of the extremity should be the primary goal, and focusing on this goal may help dismiss any unrealistic expectations regarding treatment outcomes.
Treatment Strategy
Because the majority of children with hypoplasia of a portion of the upper extremity are very high functioning, they require no surgical care. Nonetheless, there are two instances where surgical treatments are helpful. The first indication is to remove a “floppy” digit that is interfering with the functional abilities of the hand. In such cases, excising the affected digit and reconstructing the local web space are recommended as surgical care. A short course of occupational therapy following the procedure may be helpful as well. The second circumstance, which is discussed in another chapter, involves reconstructing and improving the function of a hypoplastic thumb.
Brachydactyly and Symbrachydactyly
After considering hypoplasia of the upper extremity in general, a discussion of the more common clinical types is appropriate. Flatt reported that out of 2,758 collected cases of congenitally anomalous hands, brachydactyly (5.2 %) and thumb hypoplasia (3.5 %) were the most frequently seen undergrowth conditions (Flatt 1994a). Because thumb hypoplasia is discussed as a separate topic elsewhere, this section will focus on brachydactyly and symbrachydactyly.
The term brachydactyly as translated from Greek means “short finger.” While the whole digit may appear to be small, on radiographic examination, an individual bone segment is often smaller than normal. When the phalanges are involved, the middle phalanx is the most commonly affected bone. In this instance, the condition may be referred to as brachymesophalangia (short middle phalanx). Short metacarpals can be seen in association with some syndromes (e.g., Turner’s), so the term brachymetacarpia may be encountered in the literature (Fig. 1). It should be stated that these terms are purely descriptive and do not imply that one type consistently has a more favorable prognosis than others.


Fig. 1
Fourteen-year-old female with bilateral ring and small short metacarpals otherwise known as “knuckle-knuckle-bump-bump” (Courtesy of Shriners Hospitals for Children, Philadelphia)
Most forms of brachydactyly are inherited in an autosomal dominant manner, usually with variable severity. However, there are some cases of brachydactyly are felt to be sporadic in occurrence because of no well-documented family inheritance pattern. On the molecular level, alterations in BMP cartilage-derived morphogenic protein have been shown to be associated with brachydactyly in humans and mouse models (Waters and Bae 2012a; Fig. 2). A classification system for brachydactyly, first proposed by Bell in 1951 (Fitch 1979), focuses on the anatomic location of the hypoplastic segment to categorize the anomaly (Table 3). This system has been most useful in the identification of certain inheritance patterns by being able to follow specific types along family pedigrees. For example, the most common types, A3 and D, have been shown to demonstrate autosomal dominant inheritance with reduced penetrance. Some populations also have a relatively high frequency of certain types of brachydactyly (Temtamy and Aglan 2008). As far as the clinical presentation is concerned, the degree to which any digit is involved may range from a “small, but normal” appearing finger to a tiny residual “nubbin ,” which may be nothing more than a small pouch of skin attached to the hand.
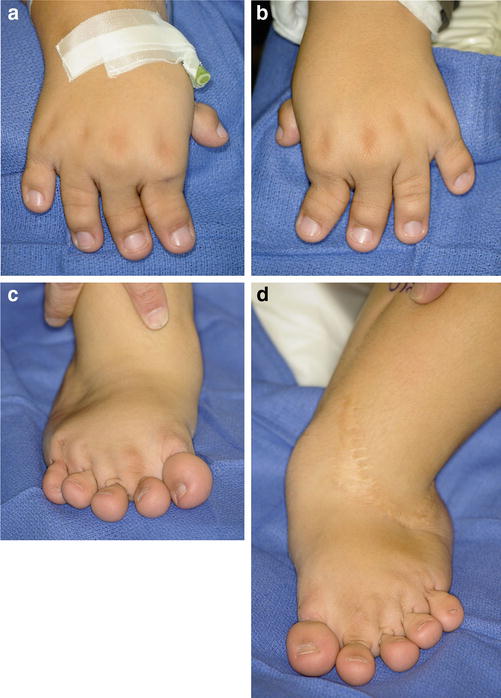
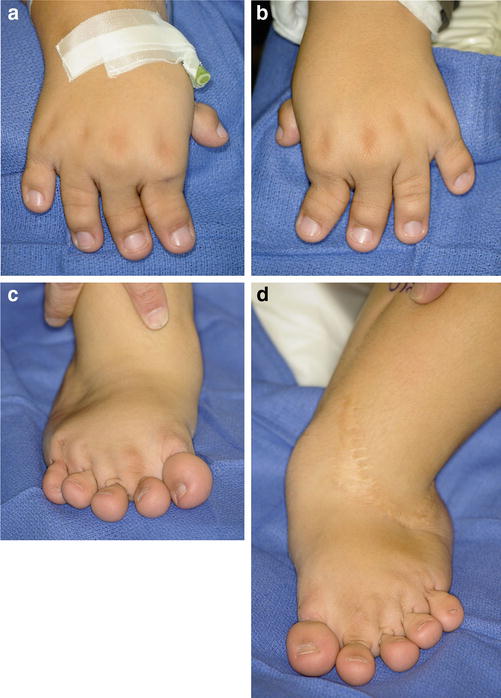
Fig. 2
Fourteen-year-old female with Grebes’ chondrodysplasia and severe brachydactyly associated with a cartilage-derived morphogenetic protein deficiency (Courtesy of Shriners Hospital for Children, Philadelphia). (a) Right hand, (b) left hand, (c) right foot, (d) left foot
Type | Inheritance | Proposed gene defect | Clinical features |
|---|---|---|---|
A1 | Autosomal dominant | Indian hedgehog | Short middle phalanges (usually digits I–IV) |
Rare | |||
A2 | Autosomal dominant | BMP receptor on q4 | Short middle phalanx (digit II) |
Very rare | |||
A3 | Autosomal dominant | Unknown | Short middle phalanx (digit V) |
Common (up to 21 % in some populations) | |||
A4 | Few pedigrees identified | Mutation: HOXD13 | Short middle phalanges (digits II and V) |
Rare (autosomal dominant) | |||
B | Few pedigrees identified | Mutation: ROR2 | Absence/hypoplasia of terminal digits (II–V), with nail absence |
Rare (autosomal dominant) | Distal phalanx of thumb may be duplicated | ||
C | Few pedigrees identified | Mutation: CDMP1 | Brachymesophalangy of digits II, III, and V |
Rare (? autosomal dominant) | Ring finger (digit IV) is usually normal in size | ||
D | Autosomal dominant (up to 4 % in some populations) | Unknown (possible mutation: HOXD13) | Short distal phalanx of digit I (thumb) |
E | Autosomal dominant | Unknown (possible mutation: HOXD13) | Variable shortening of metacarpals (often digit IV) |
When evaluating a patient with small digits, the term symbrachydactyly may be encountered in the congenital hand anomalies literature. As defined, symbrachydactyly is the condition representing hypoplastic digits (brachydactyly), webbing between fingers (syndactyly), and a general hypoplasia of the hand. To avoid confusion, brachydactyly refers specifically to the digit, whereas symbrachydactyly describes a spectrum of clinical findings seen in the hand.
A descriptive classification system has identified four separate types of symbrachydactyly: peromelic, oligodactylic, short finger, and monodactylic (Nguyen and Jones 2009) based upon the most commonly seen anatomic features (Figs. 3 and 4). Symbrachydactyly is often seen unilaterally, and the occurrence is felt to be sporadic in nature. It is secondary to a failure of formation, but the exact manner by which this occurs continues to be investigated. Symbrachydactyly can be seen in association with other conditions, and the classic example is Poland’s syndrome (absence of the sternal head of the pectoralis major muscle with various degrees of ipsilateral hand hypoplasia; Fig. 5). This condition has recently been reported in association with transverse deficiency at the level of the forearm (Kallemeier et al. 2007). The term “atypical cleft hand” is also seen describing cases of symbrachydactyly.




Fig. 3
Short finger symbrachydactyly is characterized by the triad of syndactyly, brachydactyly, and symphalangism (Courtesy of Shriners Hospitals for Children, Philadelphia)

Fig. 4
Monodactylic symbrachydactyly with perseveration of the thumb (Courtesy of Shriners Hospitals for Children, Philadelphia)

Fig. 5
A young girl with a Poland’s syndrome denoted by the absence of the pectoralis muscles and the breast nipple (Courtesy of Shriners Hospitals for Children, Philadelphia)
Although symbrachydactyly and constriction band syndrome (CBS, discussed in another chapter) can appear similar in clinical appearance, the conditions have different diagnostic and treatment implications. There are two distinct differences. First, in patients with CBS, actual bands are usually identified elsewhere in the body. However, in symbrachydactyly, only one hand is commonly affected, and no other bands are seen. Second, with symbrachydactyly, the anatomic structures proximal to the small digits are also hypoplastic or abnormal. In CBS, the musculoskeletal structures proximal to a constriction band are normal in size (Fig. 6).


Fig. 6
Constriction band syndrome around the index and long fingers with normal musculoskeletal structures proximal to the banding (Courtesy of Shriners Hospitals for Children, Philadelphia)
While classification schemes regarding brachydactyly and symbrachydactyly are helpful in describing the child’s clinical presentation, these systems are unable to predict the child’s ability to use the hand. Any surgical recommendations should focus on improving a child’s functional outcome as “function trumps form.” Input from the family about hand use, evaluations from therapists, and direct observation of the patient are critical in the decision-making process. Many patients with brachydactyly and symbrachydactyly are highly functional, adapt well to their hand anomaly, and do not warrant surgical intervention. They may occasionally need an assistive device to help with a specific task, however; surgery would not appreciably improve their function. There are cases that warrant surgery to augment hand use.
Probably the most common surgical technique to augment function involves altering the skin about the affected digit(s) through syndactyly release and/or web space reconstruction. Because the care of syndactylized fingers is presented in another chapter, a brief summary of web space reconstruction will be discussed here. The main goals of this procedure are to increase digital separation (span) and improve the apparent length of the fingers by providing depth to the web space. The Z-plasty and its varied modifications are the most common methods used to improve the web space (Shaw et al. 1973). Strict attention to detail is needed when designing the angles and arm’s length of flap transpositions in order to maximize skin mobilization. Also, great care must be used when handling the transposed flaps so that tension on the skin is minimized. In most cases, well-designed skin flaps do not require additional soft tissue coverage. However, if skin is needed, a full-thickness skin graft can be used to supplement the reconstruction. As mentioned in the treatment of syndactyly, skin grafts should be avoided in the web space commissure due to their propensity to contract.
The actual length of a finger can be improved in two ways. For minor changes in digit length, an osteotomy and interposition bone grafting can be used. While this technique allows for immediate gains in length, the concern is that inserting too large a graft in a small digit may compromise the surrounding skin and soft tissue structures leading to necrosis of the fingertip (Flatt 1994b). An alternative is distraction osteogenesis,which involves gradual lengthening of the bone and the soft tissues. There have been many methods described to achieve this task (Arata et al. 2011), although the basic technique requires an osteotomy and a device to gradually distract (lengthen) the osteotomy site. The most common types of distractors are uni-plane external fixators, attached to the bone by small wires. The slow distraction rate, about 0.5 mm to1mm per day, allows for both fracture callus formation and the accommodation of the soft tissues necessary for bone lengthening. Gains in digital length of up to 3.5 cm have been reported (Seitz and Froimson 1995). After the bone is lengthened to the desired amount, the distraction ceases and the external fixator is left in place until the regenerate callus matures to resemble normal bone (i.e., a cortical shell and medullary cavity). Subsequently, the device is removed and appropriate therapy is begun. Early removal can result in callus deformation or overt fracture through the regenerative bone.
Nonvascularized toe phalangeal transfer is a method used to achieve immediate length in a hypoplastic digit. The technique typically involves harvesting the proximal phalanx from a toe, then transplanting it within the skin of a hypoplastic digit. This procedure is controversial with regard to indications and outcome. The best results are when the procedure is done before 18 months of age, as the rates of physeal arrest and phalangeal resorption increase beyond this age (Nguyen and Jones 2009). Preliminary nonvascularized toe phalangeal transfer followed by distraction lengthening of the phalanx has been performed (Netscher and Lewis 2008). A recent article has shown that there is potential donor site morbidity with the nonvascularized toe phalangeal transfer, thus narrowing the indications for he procedure (Garagnani et al. 2012).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


