Hydrops
Paula J. Woodward, MD
DIFFERENTIAL DIAGNOSIS
Common
Nonimmune Hydrops
Idiopathic
Cardiac
Structural Cardiac Defect
Tachyarrhythmia
Bradyarrhythmia
Fetal Masses
Hemangioendothelioma
Teratoma
Vascular Malformations
Placental Chorioangioma
Chromosome Abnormalities
Turner Syndrome (XO)
Trisomy 21
Twin-Twin Transfusion Syndrome
Infection
Immune Hydrops
Rh Incompatibility
Other Antibodies
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Defined as fluid accumulation in 2 or more body cavities
Skin/subcutaneous edema
Scalp edema often first sign
Ascites
Bilateral pleural effusions
Pericardial effusion
Other findings
Placentomegaly (placenta thickness > 40 mm)
Polyhydramnios
Hepatosplenomegaly
Broadly classified as immune (hemolytic disease → fetal anemia) and nonimmune (all others)
90% are nonimmune hydrops
10% immune
Helpful Clues for Common Diagnoses
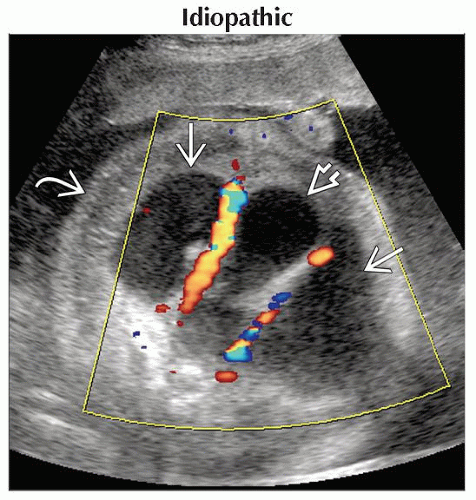
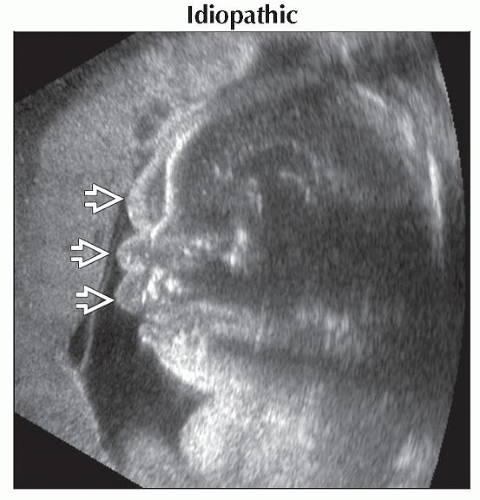
Idiopathic
Over 50% of cases will not have an identifiable cause
Structural Cardiac Defect
Poor contractility → heart failure → hydrops
May be accompanied by bradycardia
Tachyarrhythmia
Sustained heart rate > 200 bpm
Supraventricular tachycardia (SVT) most common cause
Hydrops develops in 50-75% fetuses with sustained tachycardia
Increased risk of ischemic brain injury when hydrops is present
Bradyarrhythmia
50% associated with cardiac malformation, particularly atrioventricular septal defects
50% of cases seen in mothers with connective tissue disease
Increased mortality with heart rate < 50 bpm
Fetal Masses
Any mass causing increased cardiac output may lead to failure and hydrops
Teratomas and vascular malformations most common
Hemangioendothelioma may cause hemolytic anemia in addition to arteriovenous shunting
Chest masses may also impede cardiac return
Placental Chorioangioma
Benign, vascular placental tumor
Fetal hydrops from arteriovenous shunting or from fetal anemia secondary to hemolysis
Hydrops uncommon if mass is < 5 cm
Polyhydramnios common with large masses
Turner Syndrome (XO)
Female fetus with large, septated cystic hygroma
Failed or delayed connection between internal jugular veins and nuchal lymph sacs
Hydrops secondary to fluid overload from lymphatic obstruction
Edema is diffuse and may be dramatic
Dorsal pedal edema prominent feature
Hydrops can be seen in first trimester
Prognosis with hydrops is dismal
Trisomy 21
Small cystic hygroma (increased nuchal translucency in 1st trimester) becomes nuchal thickening in 2nd trimester
May present with hydrops
Other markers often seen
Twin-Twin Transfusion Syndrome
Monochorionic twins with artery-to-vein anastomoses in the placenta
Recipient at risk for hydrops
Larger twin with polyhydramnios
Donor at risk for growth restriction
Smaller twin with oligohydramnios
Twin-twin transfusion syndrome (TTTS) staging
Stage 1: Donor bladder visible, normal Doppler
Stage 2: Donor bladder empty, normal Doppler
Stage 3: Donor bladder empty, abnormal Doppler
Stage 4: Hydrops in recipient
Stage 5: Demise of one or both
Infection
Parvovirus most common but can occur with any severe infection
Infection → anemia, myocarditis
Look for other signs of infection
Intracranial and liver calcifications, ventriculomegaly, hepatosplenomegaly, echogenic bowel, growth restriction
Immune Hydrops
Maternal antibodies cross placenta and cause lysis of fetal red blood cells, leading to fetal anemia
Anemia causes an elevated middle cerebral artery (MCA) peak systolic velocity (PSV)
Need for intervention (transfusion) generally based on relationship of MCA PSV to gestational age
Rh Incompatibility
Maternal lack of D antigen on erythrocyte membrane (Rh -)
Sensitization 2° to fetal-maternal hemorrhage
Fetal D antigen causes maternal antibody response (< 1 cc fetal cells can lead to anti-D antibody response)
With subsequent pregnancy, maternal antibodies attack fetal red blood cells
Leads to lysis of fetal erythrocytes
Causes anemia and may progress to hydrops if left untreated
Other Antibodies
Non-D antigen causes alloimmunization (usually from incompatible blood transfusion)
Kell, Duffy, Kidd, E, C, c, and others
Most are variably present in different ethnic populations
Other Essential Information
First trimester hydrops highly associated with aneuploidy
Turner, trisomy 21 most common
Nonimmune hydrops
Over 50% have no unifying diagnosis or directly identifiable cause
22% have a cardiac defect
16% have aneuploidy
Turner syndrome > trisomy 21
Trisomy 18 and 13 less likely to present with hydrops (growth restriction more common)
Image Gallery
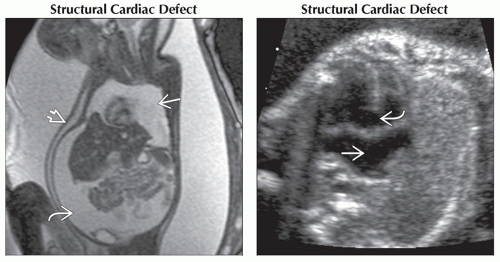 (Left) Coronal T2WI MR shows the typical MR findings of hydrops including high-signal skin edema
 , pleural effusions , pleural effusions  , and ascites , and ascites  . Hydrops resulted from poor cardiac return secondary to ectopia cordis (seen on other images). (Right) Four chamber view shows both a ventricular septal defect . Hydrops resulted from poor cardiac return secondary to ectopia cordis (seen on other images). (Right) Four chamber view shows both a ventricular septal defect  and absence of the atrial septum and absence of the atrial septum  . The ventricular rate was 53 beats per minute. 50% of fetuses with sustained bradycardia will have a cardiac malformation. . The ventricular rate was 53 beats per minute. 50% of fetuses with sustained bradycardia will have a cardiac malformation.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|