Fig. 8.1
(a) A 12-year-old boy had a femoral shortening of about 4.5 cm due to the growth arrest of distal femur. (b) Lengthening over an IM nail was performed using a trochanteric entry tibial nail and a monolateral external fixator. (c, d) The target length was achieved. (e) Two interlocking screws were fixed at the distal segment and the external fixator was removed. (f) 1 year later, the distraction callus had healed

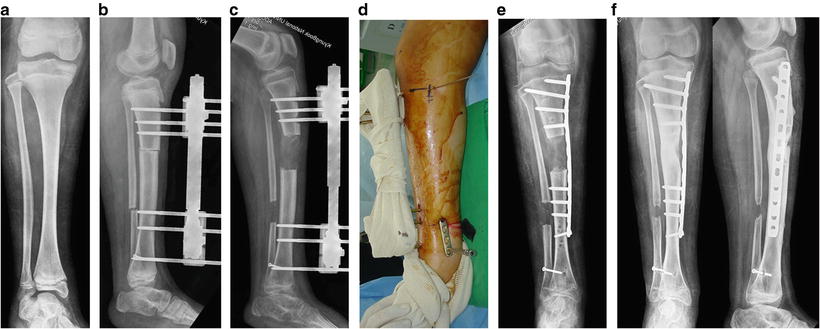
Fig. 8.2
This soldier was struck by an IED (improvised explosive device), causing open brain trauma and open fractures of the left femur and right forearm. (a–c) A 10-cm leg length discrepancy (LLD) with angulation, rotation, and translation of the femur developed. (d–f) Acute correction of the angulation, translation, and rotation was followed by lengthening over nail of 10 cm. (g) Functional gait was restored
Gordon et al. described their initial experience using LON in preadolescents in a retrospective series [8]. Nine children (average age, 9 years and 10 months) with femoral length discrepancy were treated with femoral lengthening over a humeral intramedullary nail. After nail insertion, a monolateral external fixator was placed and lengthening was performed through a proximal osteotomy. No avascular necrosis or proximal femoral valgus was noted at a minimum of 2 years follow-up. The authors concluded that the “technique is effective but has a high rate of complications, including osteomyelitis, which developed in two of the nine patients.” The technical challenge of pin placement remote from the intramedullary device requires practice, but is necessary to prevent the risk of bacterial contamination of the canal from the external fixator pins.
Box 8.1
When positioning the external fixator pins or wires, contact with the IM nail should be avoided.
Over-reaming of the medullary canal by 1.5–2 mm may be needed to under-size the diameter of nail, and thus prevent binding of the nail during lengthening.
Plate-Assisted Lengthening (PAL)
Iobst and Dahl first introduced this technique in 2007 [9]. This study is a description of the surgical technique and a retrospective examination of six patients treated using a technique designed for children with open growth plates as a means to remove the fixator sooner than with a fixator alone. A percutaneous locking plate is inserted at the beginning of the lengthening, along with a circular external fixator. Axis deviation was a problem in two cases, requiring adjustment during the locking of the plate. The plate is percutaneously locked at the completion of lengthening, at which time the fixator is removed. The procedure is tedious because of fixator hardware interfering with access for locking screws. The goal of shortening fixator time was accomplished with a mean external fixation index of 0.42 months/cm. Oh et al. also described a technique similar to limb lengthening with a submuscular locking plate [10, 11]. Submuscular plating has the advantage of providing angular stability and preserving the periosteal and endosteal blood supply, which is beneficial for distraction osteogenesis. The main indication of this technique is when an intramedullary nail is not a viable option, as in patients with a narrow medullary canal, bone deformity, open physes, or joint contractures (Figs. 8.3, 8.4, and 8.5).
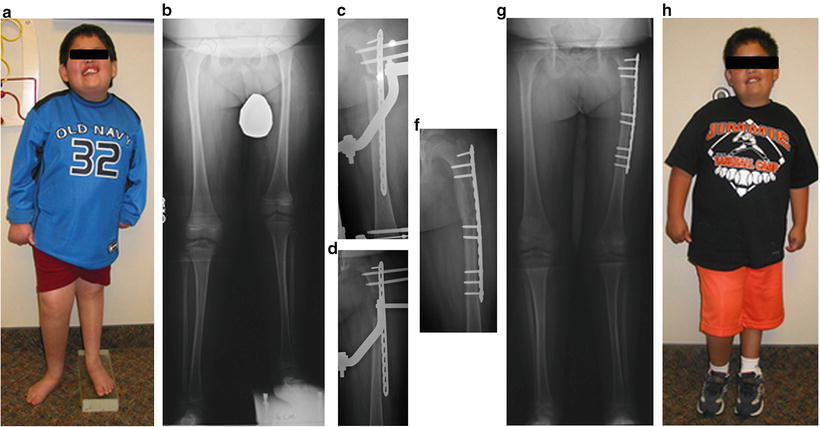
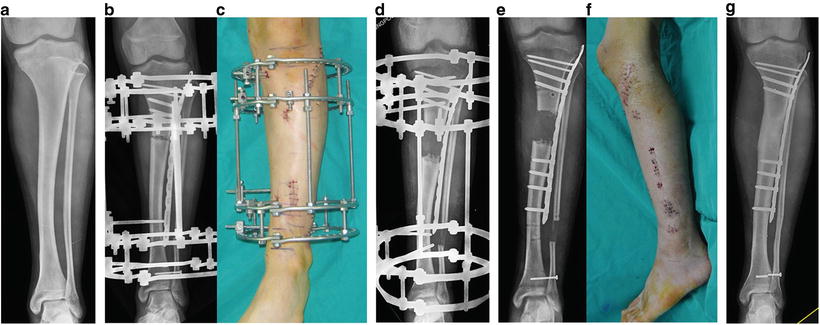
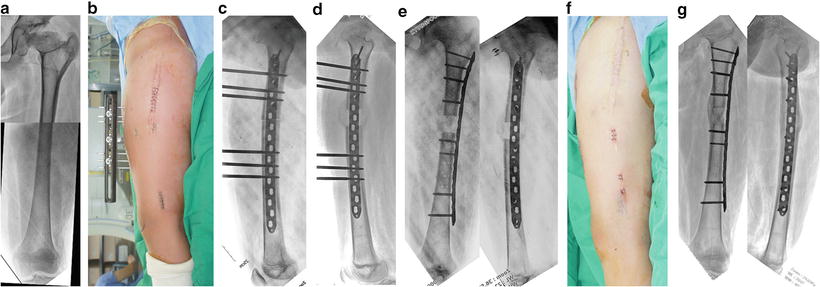
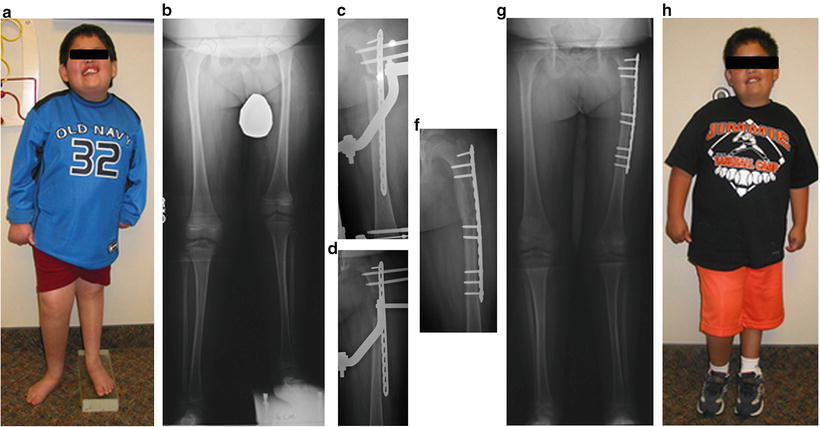
Fig. 8.3
(a, b) Clinical photo and AP X-ray of 6-year-old boy with 5.5-cm LLD secondary to congenital femoral hypoplasia. (c) AP X-ray of femur at 1 week of distraction. (d) AP X-ray of the femur at 3 weeks distraction. (e) AP X-ray of the femur at 7 weeks, after plate locking and frame removal. (f, g) X-ray and clinical photo at completion of treatment
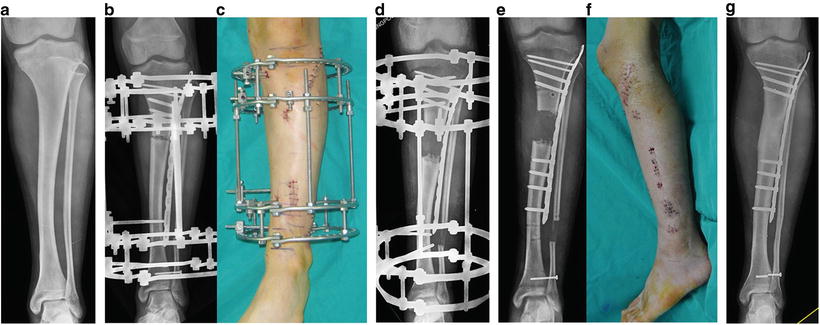
Fig. 8.4
(a) A 15-year-old boy had a tibial shortening of about 4.5 cm due to congenital postero-medial bowing. (b, c) A submuscular locking plate was placed laterally without involving the physeal plate, and a ring external fixator was fixed. After achieving the target length (d), four screws were percutaneously placed in the distal segment (e) and the external fixator was removed (f). Seven months later, the distraction callus had healed without complications (g)
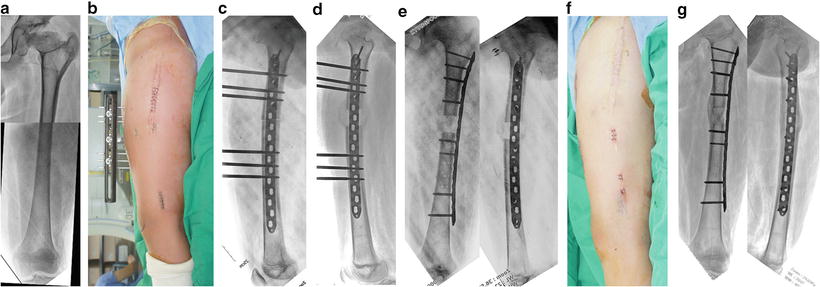
Fig. 8.5
(a) A 14-year-old boy had a femoral shortening of about 3.5 cm due to the Perthe’s disease. (b, c) Submuscular locking plate was placed laterally, and a monolateral external fixator was fixed anteriorly to lengthen the femur. After achieving the target length (d), four screws were percutaneously placed in the distal segment (e) and the external fixator was removed (f). (g) 10 months later, the distraction callus had healed uneventfully
Box 8.2
When placing the external fixator, half-pins or wires should not contact plate or screws, to avoid cross-contamination, which may evolve into deep infection.
To give sufficient stability, a longer plate should be chosen unless an anatomical contraint is present. Also, enough screws are needed to stabilize each segment.
Protection from full weight bearing and the use of a protective device (such as a patellar tendon bearing brace in tibia lengthening) is recommended until sufficient consolidation of the distraction callus is achieved.
When fixing a screw in skeletally immature patients, the adjacent physis should not be violated.
Insertion of screws in the distal segment at the end of distraction period should be performed prior to removal of the external fixator. This will prevent loss of correction that was gained at the lengthening site.
Lengthening and Then Plating (LAP)
This hybrid technique employs an external fixator lengthening, with the external fixator replaced by a percutaneously inserted plate at the completion of the bone lengthening (Figs. 8.6 and 8.7) [12]. Rozbruch and Fragomen published a retrospective case-matched comparison between LAP and a more typical Ilizarov technique with 27 extremities in each group [13]. The time wearing the frame and external fixation index were lower in the LAP group (4.5 vs. 6.2 months and 1.5 vs. 2 months/cm). Axis deviation was observed in seven patients in the LAP group and six in the classic group. Varus malalignment with plate breakage occurred in two patients in the LAP group. Pin-tract infection was more common in the classic group (12 vs. 2). No deep infections occurred in the LAP group.