Fig. 1
(a) Anteroposterior and (b) lateral radiographs demonstrating a humeral shaft fracture in a 6-day-old infant, which occurred as a result of a complicated delivery (Courtesy of Joshua M. Abzug, MD)
Humeral shaft fractures in children younger than 3 years of age may be associated with child abuse/non-accidental trauma. Fracture patterns correlated with abuse include transverse fractures, typically caused by direct trauma; oblique fractures, produced by traction with rotation of the humerus; and metaphyseal bucket-handle fractures (Fisher 1958). The presence of concomitant fractures of the ribs, sternum, or scapula is highly suspicious for child abuse and should be investigated further. Fractures of the humeral diaphysis may also occur following a fall on an outstretched hand (FOOSH) or from direct trauma to the upper arm (Shrader 2007; Carson et al. 2006).
The mechanisms of injury in children older than 10 years of age are most frequently associated with motor vehicle collisions and sporting activities. However, pathologic fractures may be seen in this age group due to various tumors and diseases affecting bone integrity, as the humerus is a common site of bone cysts and other benign lesions (Shaw et al. 1997; Caviglia et al. 2005; Carson et al. 2006; Shrader 2007) (Fig. 2). Stress fractures may also be observed, although there will be no displacement or visible deformity.


Fig. 2
(a) Anteroposterior and (b) lateral radiographs of the humerus demonstrating a benign unicameral bone cyst within the proximal humerus. Pathologic fractures are common when large cysts are present in this area (Courtesy of Joshua M. Abzug, MD)
Assessment of Humeral Shaft Fractures
Signs and Symptoms of Humeral Shaft Fractures
Children and adolescents with humeral shaft fractures typically present with mid-arm pain, swelling, and ecchymosis. Patients often hold the affected arm in adduction and internal rotation. A concomitant radial nerve injury may be present when a humeral shaft fracture occurs or as a complication of manipulation (Caviglia et al. 2005; Shrader 2007). When a radial nerve injury is present, patients of sufficient age (typically 8 years or greater) will complain of numbness to the dorsum of the hand between the first and second metacarpal and motor deficits, including decreased thumb and wrist extension, and difficulty with forearm supination. Therefore, radial nerve function should be evaluated by testing the first dorsal web space sensation as well as wrist, thumb, and digital extension. In addition to a decrease in function of forearm muscles, patients who sustain a Holstein-Lewis fracture will frequently display a significant decrease in strength of the triceps as well.
Physical findings in the neonate are similar, with mid-arm swelling, ecchymosis, and possible deformity. However, as infants cannot adequately express pain and discomfort, these patients may exhibit irritability when held. In addition, neonates sustaining a humeral shaft fracture may refuse to move the affected extremity secondary to pain, termed a “pseudoparalysis,” or may demonstrate an asymmetric Moro reflex (Caviglia et al. 2005; Benjamin and Hang 2007). Differential diagnoses for a diaphyseal humerus fracture in a newborn include a clavicle fracture, brachial plexus injury, and separation of the proximal humeral epiphysis (O’Neill et al. 1973; Szaley and Rockwood 1982; Leonidas 1983; Caviglia et al. 2005). However, it is important to remember that a humerus fracture can coexist with a brachial plexus birth palsy.
Humeral Shaft Fracture Imaging and Other Diagnostic Studies
Plain radiographs of the humerus are sufficient for diagnosis of a humeral shaft fracture. Anteroposterior (AP) and lateral views of the entire humerus should be obtained (Fig. 3). Additionally, the shoulder and elbow joints should be visualized, with dedicated radiographic series, in order to ensure there are no concomitant injuries. Magnetic resonance imaging and bone scan with technetium may be utilized to confirm the diagnosis in cases of a suspected stress fracture (Caviglia et al. 2005). If non-accidental trauma is a possible mechanism of injury, a full skeletal survey should be obtained.
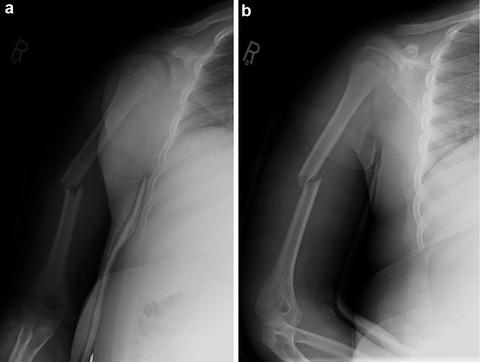
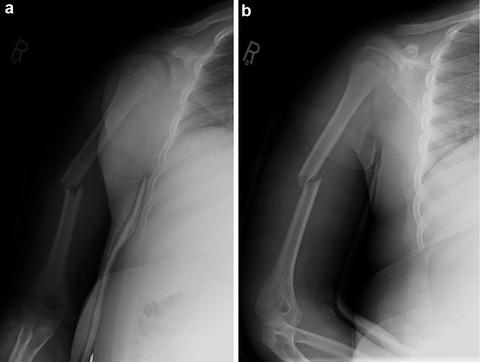
Fig. 3
(a) Anteroposterior and (b) lateral views of the humerus demonstrating a diaphyseal humerus fracture in a 12-year-old boy (Courtesy of Joshua M. Abzug, MD)
Injuries Associated with Humeral Shaft Fractures
The radial nerve is vulnerable to injury when a diaphyseal humerus fracture is sustained. The incidence of radial nerve palsies related to an injury to the humerus ranges from 2.4 % to 20 % (Caviglia et al. 2005). These palsies are described as either primary radial nerve palsies, occurring at the time of the fracture, or secondary radial nerve palsies, which occur during manipulation. Complete laceration of the radial nerve is rare; instead the radial nerve is commonly entrapped at the site of the fracture. The prognosis is generally excellent in the majority of cases with observation alone. Therefore, observation for a minimum of 8 weeks is the mainstay of treatment for radial nerve palsies, with complete resolution of symptoms occurring in 78–100 % of patients (Amillo et al. 1993).
Humeral Shaft Fracture Classification
Pediatric humeral shaft fractures are classified based on the location, fracture pattern, displacement, and angulation present. The Association for the Study of Internal Fixation (AO-ASIF) has proposed a classification scheme for diaphyseal fractures of the humerus, although its utilization has been limited for fractures in children and adolescents (Müller et al. 1991). The Müller AO classification involves three subgroups (A-C) based on the type of fracture (simple, wedge, or complex). The A subgroup consists of simple fractures. A1 fractures are spiral fractures, A2 fractures are oblique (>30°), and A3 fractures are transverse (<30°). The B subgroup consists of wedge fractures. B1 fractures exhibit a spiral wedge fragment, B2 fractures involve a bending wedge fragment and are considered unstable due to their short fracture zone, and B3 fractures involve a fragmented wedge pattern and are quite rare. B1 fractures are all at risk of having an associated radial nerve injury. The C subgroup consists of complex fractures and typically involves high-energy mechanisms of injury. C1 fractures contain fragments created from a spiral fracture and can extend into both the proximal or distal metaphysis. C2 fractures are rare and consist of segmental fragments. C3 fractures are complex fractures with irregular fragments and are typically the result of extremely high-energy mechanisms such as a high velocity missile injury (Fig. 4). These fractures are commonly open and oftentimes exhibit a concomitant radial nerve injury (Müller et al. 1991).


Fig. 4
(a) Anteroposterior and (b) lateral radiographs demonstrating a gunshot wound to the upper extremity resulting in a comminuted humeral shaft fracture in a 15-year-old boy (Courtesy of Joshua M. Abzug, MD)
Humeral Shaft Fracture Outcome Tools
No specific outcome tools exist to evaluate humeral shaft fractures.
Humeral Shaft Fracture Treatment Options
Nonoperative Treatment of Humeral Shaft Fractures
Indications/Contraindications
The majority of pediatric diaphyseal humerus fractures can be treated nonoperatively with immobilization alone. However, open fractures, fractures with obvious clinical deformity or significant angulation, fractures resulting in significant limb shortening, and fractures with a developing compartment syndrome should be treated operatively. An age-based algorithm is frequently utilized to determine acceptable angulation and displacement: indications for nonoperative management include children under 5 years of age with less than 70° of angulation and total displacement, children 5–12 years of age with 40–70° of angulation, and children greater than 12 years of age with less than 40° of angulation and 50 % apposition. Additionally, fractures resulting in limb shortening of less than 2–3 cm may be treated with immobilization alone (Table 1) (Beaty 1992; Shrader 2007; Carroll et al. 2012).
Table 1
Humeral shaft fractures: Nonoperative management
Indications | Contraindications |
|---|---|
Nondisplaced fractures | Open fractures |
Minimally displaced/angulated fractures | Fractures associated with a vascular injury |
Fractures with clinical deformity or significant angulation based on age | |
Under 5: 40–70° | |
5–12: 40–70° | |
Over 12: >40° and 50 % apposition | |
Fractures resulting in greater than 2–3 cm of limb shortening | |
Fractures with evidence of compartment syndrome |
Techniques
The first step in management of diaphyseal humerus fractures is administration of appropriate analgesia, as pain should be controlled prior to radiographic evaluation. Intravenous morphine should be considered for initial pain control in patients with moderate to severe pain while oral ibuprofen is typically sufficient for patients with mild pain. Infants with a humeral shaft fracture should be treated conservatively with immobilization of the arm utilizing a swathe technique, regardless of fracture displacement. Due to rapid healing in infants, immobilization is only necessary for 3–4 weeks (Fig. 5) (Shrader 2007). The neurovascular status should be evaluated prior to and following swathe application. It is important to assess for a concomitant brachial plexus birth palsy following swathe removal, as once callus is present, children will move the extremity if no brachial plexus palsy is present.
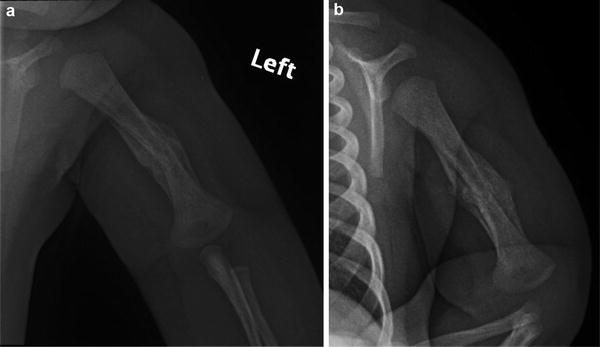
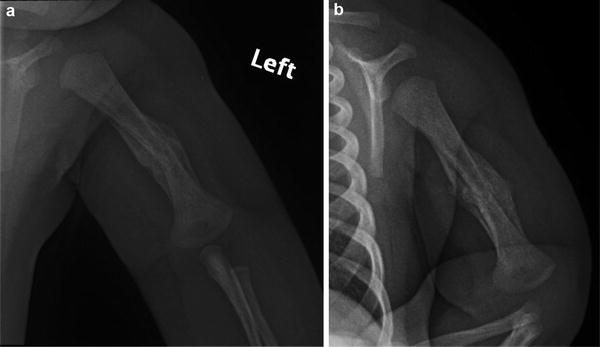
Fig. 5
(a) Anteroposterior and (b) lateral radiographs demonstrating a healing humeral shaft fracture with callous formation in a 5-week-old infant (Courtesy of Joshua M. Abzug, MD)
As the humeral shaft is enclosed in a thick periosteal sleeve that limits fracture displacement, children and adolescents who have sustained an incomplete fracture may also be managed with immobilization via a sling and swathe, collar and cuff sling, shoulder immobilizer, hanging arm cast, or fracture brace (Bachman and Santora 2006). Patients with moderately displaced or completely displaced fractures should be placed into an upper arm sugar tong splint with a supporting forearm sling or a hanging long arm cast may be utilized (Carson et al. 2006; Shrader 2007).
Closed reduction may be performed in some cases of diaphyseal humerus fractures when a clinical deformity is apparent. Following closed reduction, the correction of the clinical deformity is often believed to be of more value than the radiographic alignment (Shrader 2007). The patient is then placed in a coaptation splint for approximately 2 weeks. If after this time the fracture remains in acceptable alignment, a Sarmiento-type clamshell brace is applied for approximately 4 weeks in order for callus formation to occur (Sarmiento et al. 1990; Shrader 2007). Patients sustaining humeral shaft fractures that exhibit shortening or some anterior or posterior angulation may be treated with a hanging arm cast until acceptable healing has occurred. The hanging arm cast produces a longitudinal traction utilizing the weight of the arm and can aid in correcting anterior or posterior angulation as well as varus or valgus alignment (Fig. 6) (Caviglia et al. 2005). Radiographs should be obtained on a weekly basis for the initial 3 weeks, and shoulder range of motion exercises are generally initiated 4 weeks following the initial injury (Caviglia et al. 2005; Shrader 2007).


Fig. 6
A hanging arm cast is used to immobilize a humeral shaft fracture in a young boy (Courtesy of Joshua M. Abzug, MD)
Humeral shaft fractures that lack a plausible or documented mechanism must be investigated further by a team of child protection specialists. In the United States, it is mandatory for the treating professional to report any suspicious findings to Child Protective Services. Additionally, the patient should undergo a full musculoskeletal examination as well as a full physical, including a funduscopic, examination to assess for retinal hemorrhages, to assess for any other potential signs of abuse such as bruising. A skeletal survey should also be obtained.
Outcomes
The prognosis for skeletally immature patients who have sustained a diaphyseal humerus fracture managed nonoperatively is typically excellent, especially in younger patients, due to an increased potential for healing and remodeling (Fig. 7) (Caviglia et al. 2005).


Fig. 7
(a) Anteroposterior and (b) lateral radiographs demonstrating a healing humeral shaft fracture with callous formation in a 14-year-old boy (Courtesy of Joshua M. Abzug, MD)
Although outcomes for nonoperative management in children have not been extensively reported on, nonunion of humeral shaft fractures across all ages is rarely observed, with union rates greater than 90 % achieved with nonoperative treatment (Koch et al. 2002; Ekholm et al. 2006). Sarmiento et al. reported less than 2 % of patients with closed fractures and 6 % of patients with open fractures went on to nonunion following functional bracing. The mean time to union was 9–14 weeks in closed and open fractures, respectively. Despite a majority of patients experiencing good to excellent outcomes following nonoperative treatment of humeral shaft fractures, some studies report lower overall functional outcomes in patients with a fracture as compared to an uninjured population (Koch et al. 2002; Ekholm et al. 2006). Additional research is needed to fully understand the outcomes of nonoperative treatment in the pediatric population.
Operative Treatment of Humeral Shaft Fractures
Indications/Contraindications
Intramedullary nailing of humeral diaphyseal fractures is indicated for moderately to completely displaced fractures as well as fractures with significant angulation in adolescents approaching skeletal maturity. Open reduction and internal fixation (ORIF) of humeral shaft fractures with compression plating should be performed for open fractures, fractures with concomitant vascular injury, delayed union or nonunion, and in cases when radial nerve exploration is justified.
Surgical Procedure
Preoperative Planning
See Tables 2 and 3
Table 2
Intramedullary nailing of humeral shaft fractures: Preoperative planning
OR table: Radiolucent OR table |
Position/positioning aids: Supine or beach chair position with a small bump placed under the distal humerus
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|