Hepatic Mass in a Neonate
Alexander J. Towbin, MD
DIFFERENTIAL DIAGNOSIS
Common
Hemangioendothelioma/Hemangioma
Metastases
Neuroblastoma
Wilms Tumor
Hepatoblastoma
Mesenchymal Hamartoma
Less Common
Unilocular Cyst
Choledochal Cyst
Rare but Important
Abscess
Angiosarcoma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Hepatic tumors uncommon in perinatal period
Account for ˜ 5% of perinatal tumors
6x more likely to be benign
Most masses identified during antenatal US or neonatal physical exam
Lab tests can help to differentiate masses
CBC, α-fetoprotein (AFP), β-HCG, are markers for neuroblastoma
Biopsy or resection provide final diagnosis
Overlap of imaging and clinical finding
Helpful Clues for Common Diagnoses
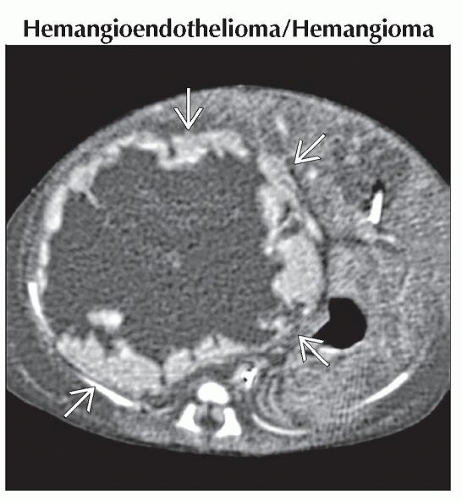
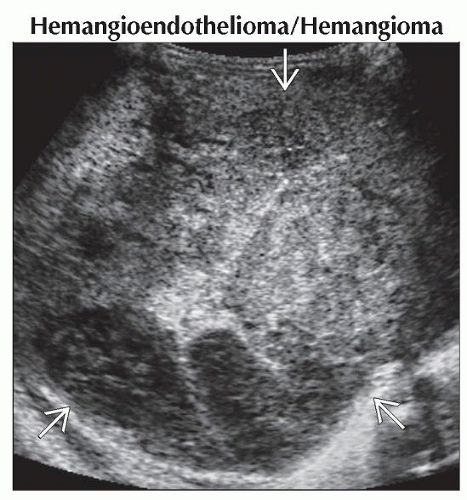
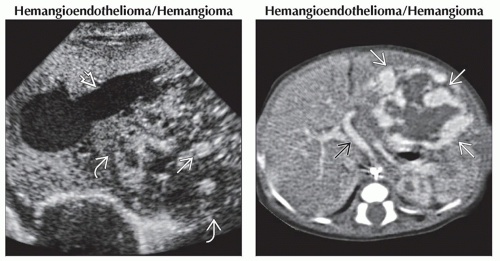
Hemangioendothelioma/Hemangioma
a.k.a. infantile hepatic hemangioma
Vascular neoplasms most common liver tumor in neonates
Account for ˜ 60% of neonatal liver tumors
Hemangioendothelioma more often symptomatic than cavernous hemangioma
Symptoms include abdominal distension, hepatomegaly, congestive heart failure, and respiratory distress
Other symptoms: Consumptive coagulopathy (Kasabach-Merritt syndrome) and rupture with intraperitoneal hemorrhage
Can be associated with hypothyroidism
˜ 50% have cutaneous hemangiomas
Large lesions have peripheral nodular enhancement on CT and MR
Multiple lesions may be present
Celiac and hepatic arteries often enlarged
Angiosarcoma and choriocarcinoma can have similar appearance
Tumor markers (AFP and β-HCG) and follow-up imaging help confirm diagnosis
Lesions should regress with age
Symptomatic lesions treated with medical or surgical therapy
Hint: High-output heart failure with liver mass
Metastases
More common than primary hepatic malignancies
Neuroblastoma most common primary tumor to metastasize to liver
Stage 4S neuroblastoma can have diffuse hepatic infiltration
Leukemia and Wilms tumor are next most common
Rare metastases include yolk sac tumor, rhabdomyosarcoma, and rhabdoid tumor
Hint: Known malignancy (i.e., neuroblastoma or Wilms tumor) with solitary or multiple liver masses
Hepatoblastoma
< 10% occur in neonatal period
Associated with hemihypertrophy, Beckwith-Wiedemann, trisomy 18, familial adenomatous polyposis coli, fetal alcohol syndrome, and extreme prematurity
Differences in neonates compared to typical age range (0.5-3 years)
Worse prognosis
Metastases occur earlier and are often systemic
Fetal circulation allows metastases to bypass lungs
Do not produce excessive AFP
Tumor rupture can occur during labor/birth
Hint: Liver mass in patient < 2 years old containing internal calcification
Mesenchymal Hamartoma
2nd most common benign hepatic mass
Typically diagnosed in 1st 2 years of life
Usually presents as palpable right upper quadrant mass
Most common in right lobe (75%)
AFP may be moderately elevated
Multiloculated cystic mass
Mixed cystic and solid
Multiple tiny cysts may appear solid
On US, septae of cysts may be mobile
Large portal vein branch may feed mass
Calcification uncommon
May ↑ in size over 1st few months
Reports of malignant transformation to undifferentiated embryonal sarcoma
Treatment is complete excision
Helpful Clues for Less Common Diagnoses
Unilocular Cyst
Usually simple cyst
No connection to biliary system
Hepatic scintigraphy (DISIDA) can prove cyst does not contain bile
Often asymptomatic and requires no intervention
Choledochal Cyst
Infantile type (patients < 1 year old)
Thought to have different etiology than childhood type
Presents with jaundice, vomiting, acholic stool, and hepatomegaly
Associated with biliary atresia in 44%
Todani type 1 cyst most common
Associated with ductal and vascular anomalies
Anomalous hepatic arteries, accessory hepatic ducts, and primary duct strictures
US is good screening test
Cyst usually in subhepatic region or porta hepatis
Distinct from gallbladder
Anechoic, thin walled, with round, tubular, or teardrop shape
MRCP or cholangiogram
Useful for showing connection of cyst to biliary system
Can see intra- or extrahepatic ductal abnormalities
Treated with excision
↓ risk of malignant degeneration if diagnosed before age 10
Helpful Clues for Rare Diagnoses
Abscess
In neonates, most small and multiple
Solitary abscess accounts for 30%
Risks include umbilical venous catheter, sepsis, and necrotizing enterocolitis requiring surgery
Other risks: Immunodeficiencies, long-term parenteral nutrition, and prematurity
S. aureus and gram-negative enteric bacteria most common organisms
Angiosarcoma
a.k.a. hemangioendothelioma, type 2
Few cases of diagnosis before age 1
Looks like hemangioendothelioma
Continued growth after treatment should raise suspicion
Image Gallery
 (Left) Transverse ultrasound shows marked enlargement of the left hepatic vein
 . Posterior to the hepatic vein is a heterogeneous mass . Posterior to the hepatic vein is a heterogeneous mass  with focal areas of increased echogenicity with focal areas of increased echogenicity  . (Right) Axial CECT in the same patient shows a large mass . (Right) Axial CECT in the same patient shows a large mass  occupying the left hepatic lobe. This mass has peripheral nodular enhancement and a central area that is hypodense. The hepatic artery is enlarged occupying the left hepatic lobe. This mass has peripheral nodular enhancement and a central area that is hypodense. The hepatic artery is enlarged  as is often the case with a hemangioendothelioma. as is often the case with a hemangioendothelioma.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|