Chapter 512 Hemolytic-Uremic Syndrome
Hemolytic-uremic syndrome (HUS) is one of the most common causes of community-acquired acute kidney failure in young children. It is characterized by the triad of microangiopathic hemolytic anemia, thrombocytopenia, and renal insufficiency (Table 512-1). HUS has clinical features in common with thrombotic thrombocytopenic purpura (TTP). The etiology and pathophysiology of the more common forms of HUS clearly delineate childhood HUS as separate from idiopathic TTP.
Table 512-1 DEFINITION OF POSTDIARRHEAL HEMOLYTIC UREMIC SYNDROME: CENTERS FOR DISEASE CONTROL AND PREVENTION, 1996
CLINICAL DESCRIPTION
Hemolytic uremic syndrome (HUS) is characterized by the acute onset of microangiopathic hemolytic anemia, renal injury, and a low platelet count. Thrombotic thrombocytopenic purpura (TTP) also is characterized by these features but can include central nervous system (CNS) involvement and fever and can have a more gradual onset. Most cases of HUS (but few cases of TTP) occur after an acute gastrointestinal illness (usually diarrheal).
LABORATORY CRITERIA FOR DIAGNOSIS
The following are both present at some time during the illness:
Note: A low platelet count can usually, but not always, be detected early in the illness, but it can then become normal or even high. If a platelet count obtained within 7 days after onset of the acute gastrointestinal illness is not <150,000/mm3, other diagnoses should be considered.
CASE CLASSIFICATION
Probable
Confirmed
COMMENT
Some investigators consider HUS and TTP to be part of a continuum of disease. Therefore, criteria for diagnosing TTP on the basis of CNS involvement and fever are not provided because cases diagnosed clinically as postdiarrheal TTP also should meet the criteria for HUS. These cases are reported as postdiarrheal HUS.
From Elliott EJ, Robins-Browne RM: Hemolytic uremic syndrome, Curr Probl Pediatr Adolesc Health Care 35:305–344, 2005.
Etiology
The various etiologies of HUS allow classification into infection-induced, genetic, medication- induced, and HUS associated with systemic diseases characterized by microvascular injury (Tables 512-2 and 512-3). The most common form of HUS is caused by toxin-producing Escherichia coli that cause prodromal acute enteritis and is commonly termed diarrhea-associated HUS. In the subcontinent of Asia and southern Africa, the shiga toxin of Shigella dysenteriae type 1 is causative, whereas in Western countries verotoxin-producing E. coli (VTEC) are the usual causes.
Table 512-2 CLASSIFICATION OF HEMOLYTIC UREMIC SYNDROME
INFECTION INDUCED
GENETIC
OTHER DISEASES ASSOCIATED WITH MICROVASCULAR INJURY
MEDICATION-INDUCED
Table 512-3 GENETIC ABNORMALITIES AND CLINICAL OUTCOME IN PATIENTS WITH ATYPICAL HEMOLYTIC-UREMIC SYNDROME
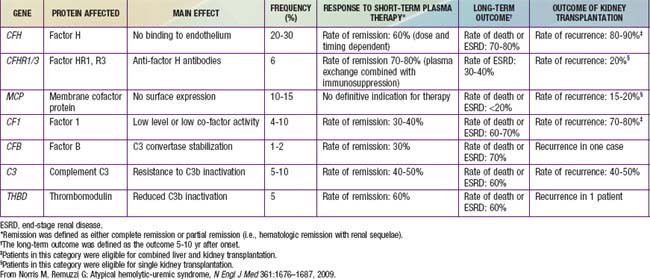
Genetic forms of HUS compose the second major category of the disease that has become clearly defined (see Tables 512-2, 512-3). Inherited deficiencies of either von Willebrand factor–cleaving protease (ADAMTS 13) or complement factor H, I, or B and defects in vitamin B12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


