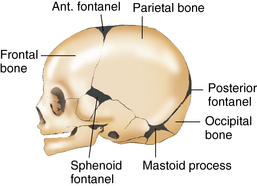
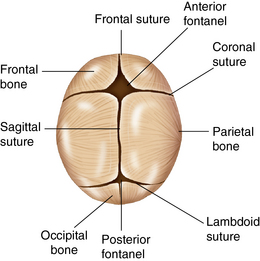
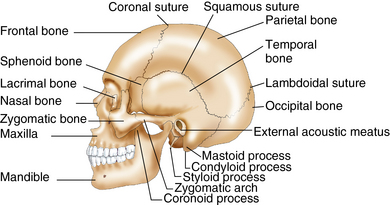
CHAPTER 9 The rapid growth of the head begins during the fifth week of embryonic life, as the brain simultaneously undergoes a similar period of rapid growth. By the eighth week, the embryo is humanlike in form, but the head size is disproportionate to the body. During this early fetal development, the head is the fastest growing part of the body and constitutes 50% of the body length at 8 weeks’ gestation. The head growth then slows during the period from the ninth to the twelfth week in the developing fetus while spine growth accelerates. During the thirteenth week, ossification of the cranium begins in the skull, which is one of the primary ossification centers of the skeletal system; the other is located in the long bones. The hair patterns on the scalp also develop during the thirteenth week of fetal development, and the scalp hair present in the term infant is established by the twentieth week.1 During the second and third trimesters of pregnancy, the head size becomes proportional to the body. The fetus continues to grow and gains 85% of its birth weight during the final period of growth. The normal growth of the skull depends on placental function, familial and hereditary factors, growth potential within the uterus, and optimum nutrition during pregnancy and early childhood. The contour of the cranium of the newborn reflects fetal positioning and the effects of the delivery presentation. The cranial bones are pliable and are loosely connected by the sutures and the fontanels, which allow the head to be molded during delivery.1 Skull fractures are rare because the cranium is adaptable, but they can occur with vacuum-assisted vaginal births, forceps delivery, or a prolonged, difficult labor. The head is slightly flattened during the normal birth process then becomes ovoid by 1 to 2 days of age. If growth retardation does occur in the fetus as a result of either intrinsic or extrinsic factors, skull growth and brain development are impacted. Depending on the timing of the insult during fetal development, the infant can suffer long-term consequences of delayed growth and development. The cranium or skull provides a protective housing for the brain and parts of the central nervous system. There are eight skull plates, or bones, in the cranium joined together by sutures (Figure 9-1). These skull plates are movable and separate at birth. The fontanels are the membranous spaces between the frontal and parietal bones and the parietal and occipital bones. The anterior fontanel lies along the coronal and frontal sutures (Figure 9-2). The posterior fontanel lies at the juncture of the sagittal and lambdoidal sutures. There are smaller fontanels located bilaterally in the lower skull. The sphenoid fontanel is located at the lower juncture of the frontal and parietal bones superior to the ear, and the mastoid fontanel is posterior to the ear at the juncture of the occipital and posterior parietal bones. The cranial sutures accommodate brain growth. The cranium is supported by the first cervical vertebra, the atlas. The atlas is a solid vertebra and rests on the second vertebra, the axis. These bones form the rotational bones of the skull. Ossification of the skull continues throughout infancy and childhood and into adulthood. The facial bones are also pliable at birth, except for the maxilla and the mandible, which are then very small and underdeveloped. The facial skeleton consists of the larger bones of the frontal area, zygomatic processes, maxilla, and mandible (Figure 9-3). The two nasal plates and the lacrimal, ethmoid, and sphenoid bones comprise the smaller bones in the head. The maxillary and ethmoid sinuses are present at birth but are small, and the sphenoid and frontal sinuses develop during infancy and childhood. Cephalhematoma is a soft, fluctuating effusion of blood trapped beneath the pericranium caused by rupture of the blood vessels. It does not cross the sagittal suture at the crown. It is usually unilateral and occurs over the parietal area. The bleeding into the periosteum of the cranium may occur slowly and therefore may not be apparent until the infant is 24 to 48 hours old. A cephalhematoma may be associated with hyperbilirubinemia. Resolution of a cephalhematoma may be slow and it may persist until 6 weeks to 2 months of age. See Table 9-1 for developmental variations in the head and neck. TABLE 9-1 Physiological Variations of the Head and Neck During Development Information Gathering for Head and Neck Assessment at Key Developmental Stages
Head and neck
Embryological development
Developmental variations
Anatomy and physiology
Physiological variations
Age
Physiological Variations
Preterm infant
Symmetrical or asymmetrical head shape with a flattened temporal/parietal region giving head an elongated shape
Craniotabes, abnormal softness of cranium, related to incomplete bone and ossification of widened sutures, is often present
Newborn
Symmetrical or asymmetrical head shape with head circumference > chest circumference; ridges over suture lines are common in neonate because of pressure on skull during vaginal birth
Craniotabes may be present until 6 months of age
Infancy
Symmetrical brain growth is reflected in occipital-frontal circumference (OFC) of skull; abnormal growth patterns of skull are indicated by a misshapen cranium and/or a rapidly increasing OFC or slow growth of skull; closure of anterior fontanel is expected by 18 months of age in healthy term infant
Early childhood
After 18 months, chest circumference exceeds head circumference by 5-7 cm; brain reaches 80% of adult size by 2 years of age; cranium continues to ossify; sutures are proximate and immobile; neck lengthens at 3-4 years of age and neck-to-body proportion is closer to adult size
Middle childhood
Nasal sinus cavities widen and deepen with skull growth, and size approximates those of an adult; thyroid gland is more readily palpable and approximates adult size
System-specific history
Age-Group
Questions to Ask
Preterm infant
History of intraventricular insult? History of maternal substance abuse? Perinatal infections?
Newborn
Vaginal or cesarean birth? Prolonged labor with prolonged third stage? Precipitous delivery? Vacuum-assisted delivery? Shoulder presentation? Respiratory distress at birth? Head tilt? Newborn screening results? History of maternal hyperthyroidism, thyroid disease, gestational diabetes?
Infancy
Newborn screening results? History of maternal infection? Neonatal infections? Meningitis? Quality of muscle tone and strength, head control? Achieving developmental milestones?
Early childhood
History of falls, clumsiness? Stable gait? Head tilt, neck pain/stiffness? Persistent lymph gland swelling? History of head trauma or falls, neck pain/stiffness? Use of bike or scooter helmet?
Middle childhood
History of headache? Onset and duration? History of head injury? Neck pain/stiffness? Use of bike or skateboarding helmet? Other protective sports equipment?
Adolescence
History of head injury? Recurrent headaches? Blurred vision? Neck pain/stiffness? Weight loss or gain? Swelling of lymph glands? Use of bike or skateboarding helmet, other protective sports equipment?
Environmental risks
Maternal exposure to hazardous chemicals or hazardous waste materials? Childhood exposure to pesticides, chemical cleaning agents, hazardous chemicals, tobacco smoke, or radiation? Limiting exposure to bisphenol A (BPA) and other plasticizers in the environment? ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Head and neck
Only gold members can continue reading. Log In or Register to continue