Chapter 1 Gynaecological and obstetric history and examination
THE WOMAN PRESENTING WITH GYNAECOLOGICAL PROBLEMS
History
Examination
The gynaecological portion of the examination should include:
Breast examination
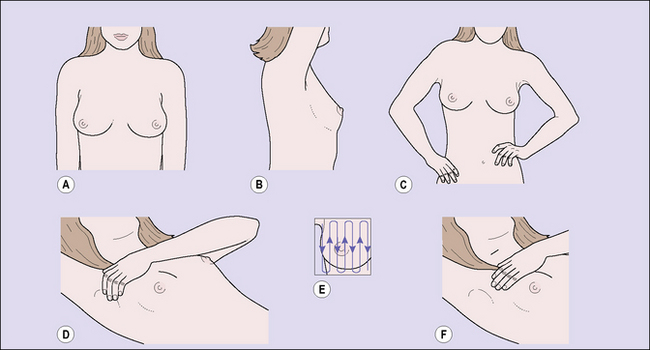
With the patient sitting facing the examiner, the breasts are inspected, first with the patient’s arms at her sides and then with her arms raised above her head (Fig. 1.1). The shape, contour and size of the breasts, their height on the chest wall, and the position of the nipples are compared, any nipple retraction being noted. The supraclavicular regions and axillae are next palpated. The latter can only be palpated satisfactorily if the pectoral muscles are relaxed. This relaxation can be obtained if the physician supports the patient’s arms while palpating the axillae. Palpation is then performed with the patient lying supine, her shoulders elevated on a small pillow. Palpation should be gentle and orderly, using the flat of the fingers of one hand. Each portion of the breast should be palpated systematically, beginning at the upper, inner quadrant, followed by palpation of each portion sequentially until the upper, outer quadrant is finally examined.
The breast self-examination that many doctors recommend to women is similar to the breast examination made by the doctor, except that the woman usually does not palpate the axillary area. Figure 1.1 demonstrates how a woman should examine her breasts. The technique can easily be taught to her by her doctor.
Pelvic examination
The patient is asked to strain down, to enable detection of any evidence of prolapse, after which a bivalve speculum is inserted and the cervix visualized. For the woman’s comfort the speculum should be warmed and the doctor’s approach sensitive and communicative. If the physician intends to take a cervical smear to examine the exfoliated cells, no lubricant apart from water should be used on the speculum. The vagina and cervix are inspected by opening the bivalve speculum (Fig. 1.2). If the patient has a prolapse, the degree of the vaginal wall or uterine descent can best be assessed if a Sims speculum is used, with the patient in the left lateral position (Fig. 1.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree