Chapter 131 Graft Versus Host Disease (GVHD) and Rejection
Acute GVHD
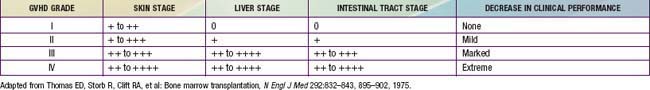
Acute GVHD usually develops from 2-5 wk post-transplantation. The primary manifestations are an erythematous maculopapular rash, persistent anorexia, vomiting and/or diarrhea, and liver disease with increased serum levels of bilirubin, alanine aminotransferase, aspartate aminotransferase, and alkaline phosphatase (Table 131-1). Diagnosis may benefit from skin, liver, or endoscopic biopsy for confirmation. Endothelial damage and lymphocytic infiltrates are seen in all affected organs. The epidermis and hair follicles of the skin are damaged, the hepatic small bile ducts show segmental disruption, and there is destruction of the crypts and mucosal ulceration of the gastrointestinal tract. Grade I acute GVHD (skin rash alone) has a favorable prognosis and often does not require treatment (Fig. 131-1). Grade II GVHD is a moderately severe multiorgan disease requiring therapy. Grade III GVHD is a severe multiorgan disease, and grade IV GVHD is a life-threatening, often fatal condition. The standard prophylaxis of GVHD relies mainly on post-transplant administration of immunosuppressive drugs such as cyclosporine or tacrolimus, often in combination with methotrexate or prednisone, anti–T-cell antibodies, mycophenolate mofetil, or other immunosuppressive agents. An alternative approach that has been widely used in clinical practice is the removal of T lymphocytes from the graft (T-cell depletion). Any form of GVHD prophylaxis in itself may impair post-transplant immunologic reconstitution, increasing the risk of infection-related deaths. T-cell depletion of the graft has also been associated with an increased risk of leukemia recurrence in patients transplanted from an HLA-identical sibling or an unrelated volunteer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree