Chapter 505 Glomerulonephritis Associated with Infections
505.1 Acute Poststreptococcal Glomerulonephritis
Pathology
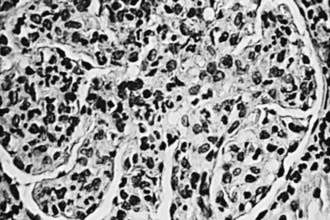
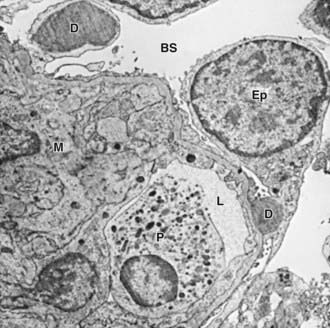
The kidneys appear symmetrically enlarged. Glomeruli appear enlarged and relatively bloodless and show diffuse mesangial cell proliferation, with an increase in mesangial matrix (Fig. 505-1). Polymorphonuclear leukocyte infiltration is common in glomeruli during the early stage of the disease. Crescents and interstitial inflammation may be seen in severe cases, but these changes are not specific for poststreptococcal GN. Immunofluorescence microscopy reveals a pattern of “lumpy-bumpy” deposits of immunoglobulin and complement on the glomerular basement membrane (GBM) and in the mesangium. On electron microscopy, electron-dense deposits, or “humps,” are observed on the epithelial side of the GBM (Fig. 505-2).