Gastroesophageal Reflux
Gastroesophageal reflux (GER) is a disease that is commonly encountered in infants and children. In general, the episodes of GER that are seen in infants and children are not clinically significant and will have no identifiable etiology. In addition, 60–65% of children with GER will undergo spontaneous symptom resolution by 2 years of life, regardless of any medical treatment.1 However, some children will have pathologic gastroesophageal reflux disease (GERD) that will result in either failure to grow appropriately, respiratory complications, or apparent life-threatening events (ALTE). This is the population that will require medical and/or surgical intervention.
History
The effects of GERD in pediatric patients have been reported for over a century.2–6 Before the introduction of proton pump inhibitors (PPIs) in the 1990s, the medical management of GERD in children and adults was relatively ineffective and based on antacids and histamine antagonists. Due to the limited spectrum of medical management in the 1950s and 1960s, several surgeons developed operative approaches for GERD management. Lortat–Jacob, Hill, Belsey, Nissen, Rosetti, and Thal all contributed greatly to the surgical management of GERD.7–14
These antireflux procedures were initially developed in adults and were effective in controlling GERD. Subsequently, they were applied to infants and children with good success.7,14,15 The overall management of GERD has progressed significantly over the past two decades with more effective PPIs and refinement in the surgical technique. One of the most important surgical advances occurred in 1991 when Dallemagne reported his experience with laparoscopic fundoplication.16 An expected evolutionary cascade led to the use of laparoscopy in children by Georgeson17 and Lobe.18 It is due to these pioneers, and the many researchers that followed, that we now know that laparoscopic fundoplication is safe and effective in treating GERD with acceptable morbidity and excellent control of symptoms in infants and children. The most daunting task currently is how to identify those children who will benefit from a fundoplication. As our diagnostic tools are being further evaluated and newer methods are being introduced, there has been renewed skepticism about who should have a fundoplication. At the same time, ongoing refinement of the operative approach has yielded even better outcomes.
Pathophysiology
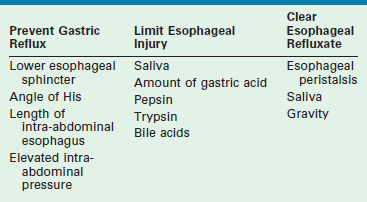
GERD is defined as the pathologic effects of involuntary passage of gastric contents into the esophagus. Ultimately, the pathophysiologic alteration that is responsible for the development of GERD is incompetence of the antireflux barriers that exist between the lower esophagus and the stomach. The result of this incompetence is the presence of gastric refluxate in direct contact with the esophageal mucosa. While initially felt to be purely acidic, research in the utility of the pH probe as a diagnostic tool has shown this is not true.19 In fact, adult literature has implicated alkaline bile reflux as a causative factor in the development of Barrett esophageal metaplasia.20 The pathologic events that occur because of GERD are due to one or multiple failures of the normal physiologic barriers that exist to prevent gastric contents from entering the esophagus, or to limit injury to the esophagus as a result of gastric refluxate, or to clear the refluxate that enters the esophagus (Table 28-1).
TABLE 28-1
Mechanisms That Either Prevent Gastroesophageal Reflux, Limit the Esophageal Injury, or Clear the Refluxate
In adults, the consequence of this refluxate in the esophagus is primarily limited to erosive esophagitis, esophageal stricture, and Barrett esophagitis. In children, its detrimental effects are much broader. Associated physiologic, anatomic, and developmental abnormalities coexist in children that make GERD and its consequences much more complex. Many children with GERD have significant neurologic impairment. These children can have increased spasticity with retching and related increased abdominal pressures. Poor swallowing mechanisms lead to gagging and choking, which add to this intermittent increased abdominal pressure. Sometimes, a hiatal hernia develops (Fig. 28-1), further predisposing to GERD. Congenital anomalies such as esophageal atresia with or without tracheoesophageal fistula (EA/TEF), duodenal and proximal small bowel atresias, congenital diaphragmatic hernia (CDH), and gastroschisis/omphalocele all predispose to the development of GERD. The consequences of GERD in children lead to the same complications seen in adults (erosive esophagitis, stricture, and Barrett esophagitis), but also include pulmonary effects (reactive airway disease and pneumonia), potential malnutrition secondary to the inability to maintain adequate caloric intake, and apneic episodes leading to ALTE spells.
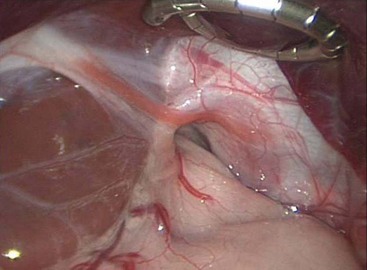
FIGURE 28-1 This intraoperative photograph depicts a de novo hiatal hernia in a 13-month-old infant. Note the enlarged hiatus. A portion of the upper stomach has herniated into the chest.
Barriers against GERD
The most important factor for preventing reflux of gastric contents into the esophagus is the lower esophageal sphincter (LES). Embryologically, the LES arises from the inner circular muscle layer of the esophagus, which is asymmetrically thickened in the distal esophagus. This thickened muscle layer creates a high-pressure zone that can be measured manometrically. In addition, this muscular thickening extends onto the stomach more prominently on the greater than lesser curvature.21 The phrenoesophageal membrane, arising from the septum transversum of the diaphragm and the collar of Helvetius, holds the LES in position. The result is an LES that lies partially in the chest and partially in the abdomen. This positioning is important for the normal barrier function against GER. Esophageal manometry can identify this transition (which is known as the respiratory inversion point) from the thoracic to the abdominal esophagus.
The LES is an imperfect valve that creates a pressure gradient in the distal esophagus. The ability to prevent GER is directly proportional to the LES pressure and its length, provided that LES relaxation is normal. In an adult study, LES pressures greater than 30 mmHg prevented GER, as documented by 24-hour pH study, whereas pressures between 0–5 mmHg correlated with abnormal pH studies in more than 80% of patients.22 Also, GER is statistically significantly more likely to develop in adults if the LES pressure falls below 6 mmHg at the respiratory inversion point or if the overall LES length is 2 cm or less.23 As noted previously, the LES is relatively fixed across the esophageal hiatus by its surrounding attachments. Malposition of the LES, which can occur with a hiatal hernia or abnormal development, causes loss of the protective function of the LES, resulting in GER. Finally, LES relaxation occurs with esophageal peristalsis initiated by the swallowing mechanism. This relaxation is normal and must occur. Inappropriate LES relaxations, referred to as transient LES relaxations, have been shown to occur sporadically, unassociated with the swallowing mechanism. Interestingly, when children with symptoms of GER were studied with pH and manometry simultaneously, reflux episodes rarely correlated with decreased LES pressures. Rather, the majority of reflux episodes occurred during transient LES relaxations, and no reflux episodes were identified during LES relaxation after swallowing with normal peristaltic sequence.24,25 There continues to be growing support that these transient LES relaxations are the primary mechanism for GER.
Another barrier to the development of symptomatic GER is the intra-abdominal length of the esophagus.26 Although no absolute effective intra-abdominal esophageal length has been identified that prevents GER, correlation between several lengths and GER have been identified. In one report, an intra-abdominal length of 3–4.5 cm in adults with normal abdominal pressure provided LES competency 100% of the time.22 A length of 3 cm was sufficient in preventing reflux in 64% of individuals, whereas less than 1 cm of intra-abdominal esophagus resulted in reflux in 81% of patients. It is believed that failure to mobilize adequate esophageal length for intra-abdominal positioning during antireflux operations can lead to less than successful results or recurrent GER in adults. However, we now know these data are not applicable in infants and children and that complete mobilization of the esophagus, in the absence of a hiatal hernia, is detrimental in infants and children through the results of a multicenter, prospective, randomized trial.27
A third barrier to reflux is the angle of His, which is the angle at which the esophagus enters the stomach. The usual orientation is that of an acute angle, which creates a flap valve at the gastroesophageal junction. Although the actual functional component of the angle of His is not well known, it has been shown to provide resistance to GER. Experimentally, when this angle is more obtuse, GER is more prone to develop. Conversely, accentuation of the angle inhibits GER.28
The ability of the angle of His to prevent GER may be diminished as a result of abnormal development or may be iatrogenic, as occurs after gastrostomy placement. When a normal angle of His is present, there is a convoluted fold of mucosa present at the gastroesophageal junction. This mucosa creates a rosette-like configuration that collapses on itself with increases in intragastric pressure or negative pressure in the thoracic esophagus, thus acting as an additional weak antireflux valve.29,30
Patients with increased abdominal pressure as a result of neurologically related retching, physiologic effects (obesity, ascites, peritoneal dialysis), or anatomic abnormalities (gastroschisis, omphalocele, CDH) are at increased risk for developing GERD owing to the effects of chronic pressure from the abdomen into the thorax.31–37 Finally, certain congenital defects such as congenital short esophagus, congenital hiatal hernia, and EA/TEF predispose to GERD. In patients with EA/TEF, the esophagus has abnormal peristalsis and the LES is incompetent. It has been reported that up to 30% of these patients will require antireflux surgery after repair of their EA/TEF.38–40 Regarding CDH, anatomic abnormalities of the esophageal hiatus and the esophagus predispose to GERD, with 15–20% of surviving patients undergoing an antireflux operation for GERD.35–37
Once the barrier to GER has been overcome (or failed), mechanisms for esophageal clearance become important in preventing damage associated with exposure of the esophageal mucosa to the gastric refluxate. The primary mechanism for esophageal clearance remains esophageal motility. However, gravity and saliva contribute to the ability of the esophagus to clear the refluxate.41,42 There are three types of esophageal contractions: primary, secondary, and tertiary. Primary contraction waves are initiated with swallowing and are responsible for the clearance of refluxed contents in 80–90% of reflux episodes. Secondary waves occur when material is refluxed into the esophagus and clearance is required, especially when the reflux occurs during sleep.43,44 Tertiary waves have nothing to do with esophageal clearance and are sporadic, non-propagating contractions. When impaired esophageal motility is present as a result of abnormal smooth muscle function, impaired vagal stimulation, or obstruction, refluxed gastric contents are not moved caudad into the stomach in a timely manner. This prolonged exposure can lead to esophageal mucosal injury and can potentiate the motility disturbance due to vagal and/or smooth muscle inflammation or injury. Saliva neutralizes refluxed material, and patients with GERD have been found to have decreased salivary function. It has also been shown that positional effects of GERD treatment may be related to gravity assisting in the clearance of esophageal refluxate.45–48
The final element for prevention of esophageal injury related to GERD is the ability to limit injury once refluxed contents have reached the esophagus. In addition to functioning as a neutralizing agent, saliva also aids in lubricating the esophageal contents, thus making it easier to clear any retained refluxate. Acid exposure has traditionally been postulated to cause the most significant injury, but more recent data has also implicated alkaline bile reflux as well.20,49 Some pediatric patients with documented GERD have been shown to have increased acid secretion.50,51 To this end, the role of PPIs in controlling GERD in this population is very important because they have the dual effect of increasing the gastric pH while simultaneously decreasing the acid volume.52–54 However, it is now recognized that some children with GERD have normal pH probe studies and acid reflux with esophageal injury is not as big an issue for this subset of patients as is poor nutrition and pulmonary complications. Other substances that increase esophageal mucosal injury include bile salts, pepsin, and trypsin. When combined with acid, bile salts are injurious to the esophageal mucosa by increasing the permeability of the esophageal mucosa to existing acid, thus further potentiating injury.55,56 Pepsin and trypsin are both proteolytic enzymes that can injure the esophageal mucosa. Both of these enzymes are more toxic at lower pH levels and, hence, are more injurious in the presence of acid.57,58
Clinical Manifestations
The presentation of GERD in infants and children is variable and depends on the patient’s age and overall medical condition. The surgeon must consider both this variability and the patient characteristics when evaluating a child with symptoms for possible GERD. Although the symptoms of GERD are variable for each patient, the actual frequency of symptoms seen in infants who have required surgical intervention for GERD has been reported (Table 28-2).59
TABLE 28-2
Frequency of Symptoms in Patients with Gastroesophageal Reflux
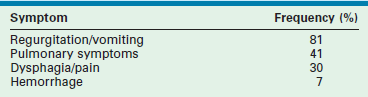
Adapted from Tovar JA, Olivares P, Diaz M, et al. Functional results of laparoscopic fundoplication in children. J Pediatr Gastroenterol Nutr 1998;26:429–31.
When considering the symptoms associated with GERD, persistent regurgitation is the most common complaint reported by parents of children with GERD.60 However, in infants, vomiting is often physiologic and can be ‘normal.’ This type of vomiting is termed chalasia of infancy and is seen early in life, usually during burping, after feeding, or when placed in the recumbent position.61 Chalasia does not interfere with normal growth or development and rarely leads to other complications. It is a self-limited process with most infants transitioning to being asymptomatic by 2 years of age or near the time of initiating solid foods.1 No treatment is necessary in patients who have chalasia, and no diagnostic evaluation should be pursued. However, when persistent regurgitation is the result of GER, it can lead to complications, including significant malnutrition and growth failure due to insufficient caloric intake.
In infants, another presenting symptom is irritability due to pain. Painful esophagitis can be the result of the acid refluxate. Discomfort leads to crying despite consoling measures.62,63 Occasionally, small volumes of feeds briefly assist in alleviating pain. However, this is generally not a lasting effect.24,25 In contrast to infants, children with GERD more often present with complaints of pain. As in adults, the pain is retrosternal in nature, and often described as heartburn. Long-standing GERD with esophagitis can lead to chronic inflammation or even ulcer formation with eventual scarring and stricture. Dysphagia develops as a result of a narrowed esophageal lumen, as well as possible esophageal dysmotility secondary to long-standing mucosal inflammation. Obstructive symptoms and pain are the two most common associated complaints when an esophageal stricture is present.64,65
Barrett esophagitis is a premalignant condition that is associated with prolonged GERD. It occurs when metaplasia develops in the esophageal squamous epithelium that is replaced with columnar epithelium. In adults, it is thought to be the result of chronic esophageal injury. Whether it develops from gastric acid injury or exposure to alkaline bile reflux is currently a controversial topic.66–68 Although uncommon in infants and children, when it does develop, serious complications often result. In addition to the increased risk for adenocarcinoma, approximately 50% of these patients will develop stricture and many patients will develop ulcers.69,70 Aggressive GERD management, along with vigilant long-term surveillance via yearly esophagogastroscopy, must be pursued to minimize these often difficult and possibly fatal complications.
Respiratory symptoms are commonly seen in infants and children. Delineating the role of GER as an etiologic agent for ongoing respiratory complaints can be difficult because of the similarity of the symptoms that are seen with other pulmonary diseases and the fact that primary aspiration from oropharyngeal dysmotility may be the inciting factor not GER. Chronic cough, wheezing, choking, apnea, or near sudden infant death syndrome (SIDS) can all be symptoms attributable to GER. Recurrent bronchitis or pneumonia can occur from aspiration of the refluxate.71 Esophageal stimulation via acidification of the esophageal mucosa causes vagally mediated laryngospasm and bronchospasm, which clinically presents as apnea or choking or mistakenly as asthma.72,73 Esophageal inflammation, as seen with esophagitis, likely enhances this mechanism.74,75 The effects of GER on premature infants with respiratory problems have been studied.76 Most of these infants were intubated for varying periods owing to respiratory distress syndrome or bronchopulmonary dysplasia. In the former group, GERD was responsible for a deteriorating pulmonary status requiring intubation. In the latter, deterioration of pulmonary status plus failure to thrive and anorexia led to the diagnosis of GERD. All improved with correction of the GERD.77
Although uncommon, hemorrhage can be a presenting symptom of GERD. Esophagitis, gastritis, and ulcer formation can lead to hematochezia or melena in a small percentage of infants or children.59
Diagnostic Evaluation
Upper gastrointestinal radiography is the most frequent initial study employed. Evidence for reflux is seen in up to 50% of the examinations.78,79 However, the absence of reflux is an extremely poor indicator of GERD as a cause of the patient’s symptoms. Furthermore, the presence of reflux on an upper gastrointestinal series does not necessarily indicate pathologic GER. The contrast study is most useful for delineating the anatomy of the esophagus and esophagogastric junction. It also evaluates esophageal clearance and assesses esophageal and gastric motility. The contrast study can identify the presence of esophageal strictures, webs, or distal obstructions, such as duodenal obstruction, antral web, or malrotation, as the cause of the reflux symptoms—which may be the case in 4% of patients.80 These correctable, anatomic causes for GER are critical to rule out before pursuing further studies.
Twenty-four hour pH probe monitoring has been considered the gold standard in diagnosing GERD since the 1980s when DeMeester established scores that correlated with the presence or absence of GERD.81–83 Boix-Ochoa later proposed a revised score that was applicable to pediatric patients aged 2 months to 3 years old that is still used today.84 Currently, the 24-hour pH probe monitoring study is recommended in infants with respiratory symptoms, especially ALTE spells or apneic events; infants who are irritable with intractable crying and anorexia; infants and children with reactive airway disease or recurrent pneumonia; and children unresponsive to medical measures in whom GER is suspected. Special considerations should be given to those children who become symptomatic after fundoplication. Conversely, the study generally is not useful or necessary for infants with uncomplicated regurgitation, children with esophagitis already diagnosed by endoscopy and biopsy, and children with dysphagia or heartburn thought to be caused by GER.
The pH study is performed by placing an electrode 2–3 cm proximal to the gastroesophageal junction and measuring the pH in the distal esophagus. The accuracy of the pH examination is dependent on the cessation of all antireflux medication: PPIs should be withheld for seven days, and histamine receptor blockers are stopped 48 hours before the study. A reflux episode is considered to have occurred if the esophageal pH is recorded as less than 4. Ideally, the examination should occur over an uninterrupted 24-hour period. The pH is continuously monitored via the esophageal electrode while the patient’s position (upright, supine, prone) and activities (awake, asleep, eating) are simultaneously recorded. The final score is calculated based on the percent of total time that the pH was less than 4, the total number of reflux episodes, the number of episodes lasting longer than 5 minutes, and the longest reflux episode.85,86
Data from the pH probe monitoring has increased our understanding of GER and taught us that not all GER is acidic. Three patterns of reflux have been described in symptomatic infants, as determined by extended esophageal pH monitoring: continuous, discontinuous, and mixed.87 Those infants with the discontinuous type rarely required an antireflux operation, whereas approximately half of those with the other two types did. One should keep in mind that medical treatment at the time of this study was much less effective than it is currently. Nonetheless, this study indicates that pH monitoring can be useful in sorting out infants with GER who may or may not require an antireflux procedure.88,89 Incidentally, all of the infants in this study, including the ‘normal controls,’ experienced reflux frequently in the first two hours after being given apple juice.
The etiology for this non-acid reflux is likely to be due to the infant diet and buffering. The infant is not capable of acidifying their gastric secretions to the extent that older children and adults are.90,91 Probe data from infants showed that gastric pH was <4 for 15% of the time in infants compared to a pH <4 for 42% of the time in older children.92 Furthermore, the infant’s milk-based diet serves as a buffer altering the pH of the gastric contents. This effect was investigated by measuring gastric pH after feeds whereby the gastric pH was >4 for a mean time of 130 minutes post-feeding.93
By using one ‘old’ diagnostic technique and one ‘new’ one, some of the disparities between pH probe observations and ‘events’ may be better understood. This is based on the observation that some reflux of acid into the lower esophagus occurs while the intraesophageal pH is still less than 4 due to a traditional acid reflux episode. This is called ‘acid re-reflux’ (ARR) and will be missed by using only pH-monitoring techniques.94 ARR is most likely to occur in patients with severe esophagitis, postprandially, and in the recumbent posture. It is now thought to be a common cause of prolonged acid contact. Detecting ARR provides a better estimation of the incompetence of the antireflux barrier than does traditional pH probe evaluations.
Two methods may be used to evaluate ARR. The first is scintigraphy, which directly measures radiolabeled liquid gastric contents flowing into the esophagus, independent of the pH of the refluxate or the esophageal lumen. The second is multichannel intraluminal impedance (MII), a method that recognizes the flow of gastric contents into the esophagus by detecting decreases in impedance from high (the esophagus) to low (the stomach) values across electrode pairs placed throughout the esophagus and in the stomach. The presence of acid, therefore, is also completely irrelevant with this diagnostic tool which can be performed at the same time as pH probe monitoring. Furthermore, MII also can distinguish liquid from gas refluxate.95–97
Recent studies using MII support the concept that measuring acid reflux (pH study) may not be the best method of evaluating GERD.98–101 These studies reaffirm that the pH probe does not simultaneously detect the majority of reflux events as defined by impedance monitoring, presumably because the re-reflux boluses are not acidic. When MII and pH monitoring are used simultaneously, there are significant reflux episodes that are not identified with pH monitoring alone because the episodes are actually non-acid reflux episodes with a pH greater than 4.99 These nonacid reflux episodes are less common in untreated GERD patients than in normal patients. MII has shown that GERD patients more commonly have liquid-type reflux events, whereas non-GERD patients generally have more gas-type reflux events.100 Additionally, MII data suggest that treatment with PPIs does not decrease the amount of reflux but rather converts the reflux to non-acid or weakly acidic in nature.101
Although essential in adults, esophageal manometry is infrequently utilized in the pediatric population. When employed, the study measures the motility of the esophagus and the pressure at the LES via a multiple-port pressure transducer placed in the esophagus and traversing the LES. The clinical data accumulated in adult patients have revealed several important points that are likely applicable to infants and children with GERD. First, it has been shown that pharyngeal swallowing and primary peristaltic contractions are responsible for the majority of the esophageal clearance of refluxed gastric contents, rather than by secondary and tertiary peristalsis as previously believed.102 Additionally, through the use of a concomitant 24-hour pH study and esophageal manometry, it has been shown that there is a direct relationship between worsening esophagitis secondary to GERD and deterioration of esophageal motility. Manometric evaluation has been particularly useful in documenting abnormal distal esophageal motility in infants after repair of EA/TEF.103 It is hoped that, as technology continues to provide more appropriately sized instruments for sophisticated manometric studies in infants and children, the usefulness and feasibility of such studies will increase our knowledge of the physiology and abnormalities associated with GERD in this population.
Endoscopic evaluation of the esophagus and stomach is occasionally needed in the diagnosis of GERD in infants and children. Hematemesis, dysphagia, irritability in infants, or dysphagia with or without heartburn in children, should prompt esophagogastroscopy to determine if esophagitis is present. Other complications, such as ulcer formation, esophageal stricture, and Barrett esophagus, can also be diagnosed during the endoscopic examination. Mucosal biopsy should be performed to stage the severity of esophagitis or to histologically exclude dysplasia or malignancy in Barrett esophagus.104,105
The relationship between delayed gastric emptying (DGE) and GERD in infants and children has been extensively studied and continues to be one of the more controversial aspects of antireflux surgery. The evaluation for DGE is undertaken using radionuclide scanning via a technetium-99-labeled meal. When documented preoperatively, DGE has not been shown to significantly improve when an emptying procedure is performed at the time of an antireflux procedure.106 In fact, one study evaluating patients with DGE undergoing fundoplication showed significantly improved gastric emptying for both solids and liquids after fundoplication alone.107 Neurologically impaired children with GERD have been shown to have DGE more often than neurologically normal children. Conflicting data regarding the benefit and complication rates for these patients undergoing emptying procedures at the time of their fundoplication have been reported as well.108 Based on these data, it is not recommended that an emptying procedure be performed for a patient with DGE and GERD unless a second operative intervention would place the patient at significant morbidity or mortality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


