Gastroenterology
Paritosh Prasad
Bradley Monash
Jess Kaplan
Garrett C. Zella
Jeffrey A Biller
Acute Abdominal Pain
Definition
(Silen W. Cope’s Early Diagnosis of the Acute Abdomen. 20th Ed. Oxford Univ. Press. 2000)
Abd pain 2/2 activation of visceral nerves (innervate hollow viscera & mesentery; poorly localizing), or somatic nerves (innervate parietal peritoneum; focal).
Parietal inflammation can be 2/2 worsening underlying visceral inflammation; presenting w/ generalized abd pain, which progressively localizes.
Pain can be referred to abd from other structures (i.e., pleuritis in lower lobe PNA, Strep. pharyngitis). (Pediatr Clin North Am 2006;53:107)
Clinical Manifestations
(BMJ 1969;1:284)
History w/ assoc sxs, signs, & physical are important to narrow differential
Concerning sx: Anorexia (appendicitis), bilious emesis (obstruction), rebound or guarding (peritonitis), assoc findings of palpable purpura (HSP) or ecchymosis on abdomen or back (pancreatitis). Fever can be concerning but nonspecific.
Localized pain can be helpful for localization, but is often nonspecific.
RUQ: Gall bladder or hepatic/peri-hepatic disease, RLL PNA
LUQ: Stomach, LLL PNA, splenic dz.
Epigastrium: Stomach, small bowel, pancreatitis, mesenteric ischemia
RLQ: Appendicitis (starts periumbilical), ovarian disease in female, colitis
LLQ: Colitis, ovarian disease in female
Suprapubic: UTI, PID
Radiating pain: To testicles or labia (nephrolithiasis), to back (pancreatitis)
Etiology
(Pediatr Clin North Am 2006;53:107)
Etiologies and working differential varies based on age. See specific topics for Rx.
Gastroenteritis (viral) & constipation most common benign causes for all ages
Appendicitis (see ED chapter); dx in 82% of children admitted w/ abd pain
Higher rates of perforation in children. Often mistaken for gastroenteritis.
Intussusception (see ED chapter); most frequent btw 3 mo–5 yr, 60% w/i 1st yr
Peak btw 6–11 mo. 60% p/w 2 of 3; abd pain, vomiting, bloody mucous stool
Small bowel obstruction: Multi etiologies, most common 2/2 adhesions from prior surgery or incarcerated hernia; p/w abd pain, vomiting (bile), distention
Incarcerated hernia: 60% inguinal (R side) in 1st yr; p/w groin bulge.
Malrotation w/ midgut volvulus: Highest incidence in 1st mo; often abd pain and bilious vomiting, but can be insidious. Surgical emergency
Necrotizing enterocolitis: Preterm but in full term as well; present in extremis
Diagnostic Studies
Evaluation is dependent on history (associated symptoms & signs) & physical exam
PMH of abd surgery raises risk of incarcerated hernia or obstruction 2/2 adhesion
Always consider the possibility of child abuse.
Peptic Ulcer Disease (PUD)
Definition
Damage to mucosal lining of upper GI tract 2/2 imbalance btw protective fxn of mucus and bicarb secretion and damage from gastric acid and pepsin, +/- external factors (NSAIDs, EtOH, other mucotoxic agents) or H. pylori infection.
Pathology
(Pediatr Rev 2001;22:349)
Acid secretion is mediated by stimulation of parietal cells by acetylcholine (vagal), histamine, and gastrin (Zollinger-Ellison syndrome).
H. pylori (gram neg spiral rod) adapted to mucous layer; infxn possibly resulting in damage of intestinal mucosa 2/2 urease secretion (hydrolyzes urea to ammonia and bicarbonate) disrupts epithelial cell fxn; +/- vacuolating cytotoxin.
Epidemiology
(J Pediatr 2005;146:S21)
H. pylori w/ ∼ 50% prevalence worldwide (from 10% [U.S. avg] to 80% w/ higher rates in lower socioeconomic groups); only 10%–15% infected develop PUD
Evidence suggests acquisition of H. pylori infection occurs in childhood (by 5–10 yo)
There is often a family history of peptic ulcer disease; unclear why
Other etiologies less common overall (can be more prevalent in inpts); stress related (severe illness, burn), 2/2 ↑ ICP (Cushing ulcer) or 2/2 NSAID and other drugs.
Clinical Manifestations
(Pediatr Rev 2001;22:349)
Generally p/w recurrent epigastric pain and can be assoc w/ postprandial or nocturnal abd pain, vomiting or food regurgitation.
In severe cases can present with failure to thrive, upper GI bleed, or chronic anemia.
Controversial whether H. pylori infxn can cause acute abd pain; NSAID- and drug-induced gastritis and ulcer formation can. (Pediatrics 1999;103:192)
Diagnostic Studies
(J Pediatr 2005;146:S21)
Initial eval w/ CBC diff (assess for anemia), ESR (IBD), LFTs, electrolytes (if recurrent vomiting), and stool evaluation for O and P (if exposure/diarrhea)
If PUD suspected, send H. pylori IgG; can’t distinguish btw current & prior infxn.
Sens 54%–94%, spec 59%–97% (assay dependent); neither sens nor spec in children 2/2 lower titer cutoffs, shorter durations of infection.
Stool antigen testing where available is highly sensitive (98%) and specific (99%)
Urea breath testing (UBT): Radio-labeled urea is ingested and then CO2 exhalation is measured; good functional test and can be used to assess for cure
Less widely used in children 2/2 concerns about radiation
Can see false +, especially <3 yo, 2/2 discoordinated swallow (oral bacteria w/ urease too) Can see false-neg if patient is already on Rx (acid suppression)
Gold standard upper GI endoscopy and bx, radiographic UGI studies less sensitive
Treatment
(J Pediatr Gastroenterol Nutr 2000;31:490)
If H. pylori +; rx w/ PPI (1–2 mg/kg/d) w/ any 2 of the following; amoxicillin 50 mg/kg/d, clarithromycin 15 mg/kg/d, and/or metronidazole 20 mg/kg/d
Studies show 75%–80% cure rate w/ 7 d of triple therapy, suggesting rx for 14 d
Complications
(J Pediatr 2005;146:S21)
Atrophic gastritis +/- metaplasia; high risk if PPI use w/o eradication; gastric CA risk
Gastric CA: Seen in 1% of H. pylori infected, likely via above mechanism
Gastric mucosa-associated lymphoid tissue lymphoma (MALT): Rarer, only 0.1%
Vomiting
Definition
Reverse peristalsis 2/2 activation of vomiting center (VC) in medulla or chemoreceptor trigger zone (CTZ) in area postrema (floor IVth ventricle).
Etiology
(Pediatr Rev 1998;19:337)
See Chart on next page
Clinical Manifestations
Assess for dehydration; Mod (5%–10% BW) w/ irritability, cool ext, dry mucous membranes, sunken eyes, dec skin turgor (1–2 sec skin pinch), Severe (>10% BW) w/ lethargy, >2 sec skin pinch, cold ext, deep acidotic breathing, HoTN, tachy.
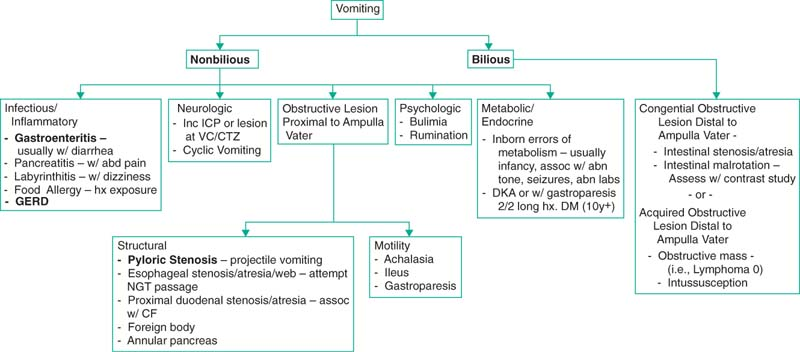 |
Diagnosis & Treatment
(Am Fam Physician 2000;61:2791; J Pediatr Gastroenterol Nutr 2001;32:S12)
Definitive management as well as diagnostic testing depends on underlying etiology.
Nonbilious emesis: Generally less concerning; some emergencies, pyloric stenosis
Bilious emesis is almost always concerning sx warranting further evaluation.
NGT placement for decompression if obstruction suspected.
Diagnostic evaluation varies but generally includes KUB and/or UGI.
W/ neonate, bilious emesis can indicate surgical disease.
Duodenal atresia: Congenital obstruction of 2nd part of duodenum, 2/2 failure to recanalize in utero, vomiting w/i hrs; pregnancy often w/ polyhydramnios
1 in 5000–10,000 and M>F, seen in 1/4 Down’s syndrome pts, 20% w/ CDH
Membranous or interrupted lesion at papilla of Vater (PV), 80% w/ PV open to proximal duodenum resulting in bilious emesis.
KUB w/ “double bubble”: Gastric air bubble and distended prox duodenum
Surgery necessary but not urgent (<48 hr) if decompressed w/ NGT and IVFs
Midgut malrotation and volvulus: Midgut rotated clockwise around SMA/V, can cause obstruction/ischemia/infarction.
Usually p/w volvulus in 1st 3–7 d w/ bilious emesis +/- abd distention; majority w/i 1st yr of life but can present at older age (recurrent abd pain)
Imaging; US w/ jejunal “spiral” or UGI w/ malpositioned SMA/V or ligament of Treitz (normally to L of spine)
Needs urgent surgery (separation of Ladd band); if early excellent prognosis
Complications: 2/2 gut ischemia → resection and short gut syndrome
Jejunoileal atresia: Mesenteric vascular accident in utero → segmental infarct
4 types abnormalities: Membranous, interrupted, apple peel, and multiple
All w/ same sx; abd distention and bilious emesis w/i 1st 24 hr.
Abdominal films w/ air-fluid levels proximal to obstruction
Can be complicated by meconium peritonitis; intense inflammation resulting in calcifications, vascular fibrous proliferation, and cyst formation
Meconium ileus: 90%–95% have CF, but only 15% pts CF have hx of mec ileus.
KUB w/ distended loops, thickened wall, filled w/ “ground glass.”
Can rx w/ Gastrograffin (successful in 16%–50%).
Treatment of nausea: (N Engl J Med 2005;352:817) based on etiology
GI tract irritation or distention: Via vagal and/or glossopharyngeal afferents (i.e., 2/2 constipation, NSAIDs, mucositis 2/2 chemo), stimulated via 5HT3R; rx with ondansetron, (5HT3R blocker) steroids to dec inflammation (mucositis)
Vestibular tract irritation (i.e., labyrinthitis): Stimulated via H1R and muscarinic receptors; rx w/ antihistamine or anticholinergics
CTZ; sampling blood for emetogens (BBB absent here): Stimulated via D2R
Emetogens can be endogenous (tumor, azotemia, HoNa) or exogenous (opioids, chemo); rx w/ haloperidol > phenothiazines (compazine)
Higher CNS center involvement: Can activate or suppress; rx anxiolytics
All stimulate VC (final common pathway): Stimulated by parasymp and H1R, acts via parasymp and motor efferents
Gastroesophageal Reflux Disease (GERD)
Definition
(Pediatr Rev 2007;3:101)
Passage of gastric contents to esophagus, can be nml (GER), or pathologic (GERD).
Pathophysiology
Intermittent relaxation of LES, acid refluxing to esophagus w/ esophagitis, chronically causes change from columnar to squamous (Barrett)
Epidemiology
Prevalence physiologic reflux ∼50% at 0–3 mo, 67% by 4 mo, 5% at 12 mo, and in children 3–17 yo, rates vary from 1.4%–8.2%
Clinical Manifestation:
Varies by age
Infants: Vomiting, FTT, irritability, asthma, ALTE, recurrent PNAs
Children/adolescent: Abd pain retrosternal CP, dysphagia, regurg, asthma/cough
Diagnostic Studies
H&P only, unless complications present or dx in question
UGI: Not sensitive or specific for GERD but identifies malro, esophageal/antral webs, pyloric stenosis, Schatzki rings, hiatal hernia.
Esophageal pH probe: Checks freq and duration of acid exposure. Reflux index = % time Ph <4 (most valid tool), upper nml 0–11 mo 11.7%, 1–9 yo 5.4%, adults 6%
Endoscopy: Visualize and bx esophagus and duodenum for inflamm and complications
Empiric Rx: widely used but not validated for any sx presentation in children
Treatment –
(J Pediatr Gastroenterol Nutr 2005;41:S41)
Evidence for 2 wk trial of hypoallergenic formula for formula fed infants
Thickening agents do not improve reflux index, do dec # of vomiting events
Positioning (if >1 yr): Left-side positioning and elevation of head of bed in sleep
Lifestyle Δ (child/adoles): No caffeine, chocolate, spicy food, tobacco, EtOH
Acid suppression: PPIs >H2RAs; if long-term PPI, check for H. pylori (risk of atrophic gastritis w/ chronic >6 mo PPI use and untreated H. pylori)
Space dosing of PPIs and H2RAs as H2RA may inhibit PPI efficacy
Majority of children develop tachyphylaxis to H2RAs
There is evidence we are over prescribing (Pediatrics 2007;120:946)
Prokinetic: Aside from cisapride (limited access) no prokinetics show benefit
Surgical Rx: Case series show generally favorable outcomes.
Prognosis:
Most outgrow sx by 12 mo; poorer prognosis w/ neuro impairment, esophageal atresia, prematurity.
Complications
Respiratory (asthma, apnea, ALTE, cough), ENT (sinusitis, dental erosions, laryngitis), esophageal strictures, Barrett, adenoCA, UGI bleeding.
∼2/3 of children w/ asthma improve to some degree w/ rx for GERD
Neurologically impaired at high risk of recurrent aspiration (PNA, pulm fibrosis)
Pyloric Stenosis
Definition
(Pediatr Rev 2000;21:249)
Gastric outlet obstruction 2/2 hypertrophy and edema of pyloric canal, and antropyloric muscle spasm → vomiting, dehydration and hypochloremic, hypokalemic, metabolic alkalosis; thought to be an acquired condition.
Epidemiology
Incidence of 1 in 250–1000, M 4–8×’s > F, caucasian predilection
Clinical Manifestations
Mean age 3 wk, but anytime birth to 5 mo; begins w/ regurgitation → nonbilious vomiting +/- projectile vomiting
Classically w/ “olivelike” mass palpated in epigastric region, pathognomonic; not always appreciable; exam enhanced by NGT decomp and prone positioning
Diagnostic Studies
US is study of choice, pyloric thickness >4 mm, length >16 mm w/ sens 89%, spec 100%; may need repeat US given operator variability.
Most common cause of metabolic alkalosis in infancy; hypochloremic metabolic alkalosis 2/2 acid loss from vomiting and decreased HCO3 secretion.
Excess bicarb can be excreted in urine w/ obligate Na loss, followed by H2O, also 2° hyperaldo 2/2 inc renin release causes distal H+ secretion and paradoxic aciduria.
Can have low or nml K but usually total body K depletion
Treatment
Reverse metabolic derangements and volume status.
Pyloromyotomy is curative, incision through serosa and mucosal layer.
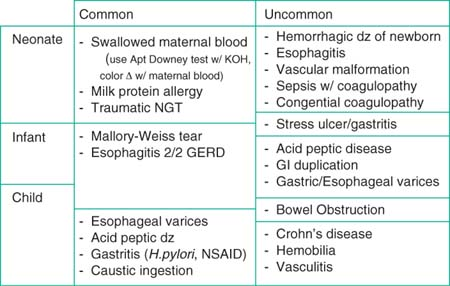
Gastrointestinal Bleeding
Definition
Intraluminal bleeding at any site from oropharynx to the anus; definition of upper GI bleed as proximal to the ligament of Treitz and lower GI bleed as distal.
Can p/w bloody vomit (hematemesis), “coffee ground” emesis, hematochezia (BRBPR; LGIB or rapid UGIB (>20% blood volume)) or melana (tarry black 2/2 digestion, darkness correlates w/ time to pass); R/o other site (nasopharynx).
Check for false coloring; red food coloring, fruit juice, beets can make vomit or stool red; Pepto-Bismol, iron, grape juice, spinach, and blueberry can make it black.
Etiology of Lower GI Bleed –
(Pediatr Emerg Care 2002;18:319)
Anal fissure: Most common cause LGIB <2 yo. Blood coated stool. Painful.
Food allergy: 3 different mechanisms; cow’s milk and soy most likely offenders
Enterocolitis: Vomiting, bloody diarrhea; +/- malabsorption, FTT
Colitis: 1st few mo of life, healthy, normal weight w/ blood in stool
Eosinophilic gastroenteritis: Infiltration w/ eos, peripheral eos, no vasculitis, p/w postprandial N/V, abd pain, watery diarrhea +/- blood, anemia, FTT
Necrotizing enterocolitis: Risk factors, prematurity, sepsis, LBW, HoTN, asphyxia
Infectious enterocolitis: Bacterial, viral, or parasitic pathogens. C. diff w/ Abx hx.
Hirschsprung disease: 10%–30% develop enterocolitis w/ fever, bloody diarrhea
Meckel diverticulum: 2/2 incomplete obliteration of omphalomesenteric duct
Painless passage of large amt of blood; otherwise healthy (2/2 heterotopic gastric mucosa in diverticulum causing adjacent ileal mucosa ulceration)
“Rule of 2s”; 2% pop, 2 inches long, 2 cm diameter, w/i 2 ft of ileocecal junction, w/ types of ectopic tissue (gastric and pancreatic), 2:1 M:F, and sx’s before 2 yo
Duplication of bowel same as Meckel but on mesenteric side, not antimesenteric
Intussusception: Usually <2 yo, colicky abd pain, “sausage shaped” abd mass w/ late finding of “currant jelly stool.” See ED Chapter.
Polyps: Outside of infant age group these are the most common source for LGIB
Painless rectal bleeding
Juvenile polyps are 90% hamartomatous (benign) usually singular but multiple seen in juvenile polyposis, Peutz-Jeghers (mucocutaneous pigmentation; higher rate GI CA but not 2/2 polyps) and Cowden syndrome
Adenomatous polyps can be premalignant; found in familial polyposis (AD but 1 in 3 new mutation; sx after 10 yo), Gardner syndrome (AD; soft tissue/bone tumors) and Turcot syndrome.
IBD: Almost all UC and ¼ of Crohn have LGIB, 1 in 4 present before 20 yo
Angiodysplasia: Vascular ectasia; assoc syndromes (Osler-Weber-Rendu, Turner)
Hemorrhoids: Rare in childhood, assess for portal HTN; common after adolescence
Henoch-Schönlein purpura: Typically 4–7 yo (but any age) systemic small vessel vasculitis w/ abd pain and bloody stools, “palpable purpura.” +/- renal and joint
GI involvement in 45%–75% cases and can precede skin findings in 15% of cases
IgA immune complex mediated
HUS: Microangiopathic hemolytic anemia, thrombocytopenia, ARF usually preceded by bloody diarrhea. (90% D+HUS w/ shiga-like toxin vs. atypical HUS/D-HUS w/o)
Clinical Manifestations
Tachycardia most sensitive sign of acute, severe blood loss
HoTN and decreased capillary refill are ominous late findings (>30% blood vol loss)
With infants who are breast-feeding, ask mother about presence of breast lesions
Hemorrhagic disease of newborn; hx. child born at home, no Vit K presents DOL 1–5
Variceal bleed 2/2 extrahepatic portal HTN; no cirrhotic stigmata, + splenomegaly
Extrahepatic portal HTN 2/2 omphalitis 2/2 neonatal umbilical vein catheter or spontaneous inflammation of umbilical vessels.
Check skin for petechiae or purpura (coagulopathy or HSP), spider angiomata (liver dz), hemangiomas or telangiectasias (Osler-Weber-Rendu).
Diagnostic Studies
Confirm w/ hemoccult for stool guaiac or gastroccult w/ vomitus
False neg w/ vit C, false + w/ red meat, veg w/ peroxidase (broccoli, radish, turnips)
NGT lavage useful if returns blood/coffee grounds = UGIB; can miss duodenal ulcer
Isolated increase in BUN can be a sign of gastric bleeding and absorption
Plain films: KUB/upright for free air (perforation), pneumatosis intestinalis (NEC), air fluid levels (obstruction).
Upper GI and small bowel follow through best for structural lesions.
Endoscopy: Indicated w/ acute UGIB necessitating transfusion or recurrent bleeding or as first step in evaluation of LGIB; contraindicated in clinically unstable patient
Retrospective studies show w/ EGD 5 most common dx = duodenal ulcer (20%), gastric ulcer (18%), esophagitis (15%), gastritis (13%), and varices (10%) in children and adolescents (Pediatrics 1979;63:408).
Rectosigmoidoscopy/Colonoscopy: Useful if not active major bleeding
Most helpful to assess IBD, angiodysplasia, polyps, pseudomembranous colitis.
Barium enema: For Hirschsprung dz, IBD, polyps, dx and rx of intussusception.
Nuclear medicine (Technetium-99 pertechnetate): Labels ectopic gastric mucosa, best for Meckel diverticulum or intestinal duplication.
Can also do Technetium-99 RBC scan for bleeding (0.05–0.1 mL/min)
Angiography: Must be >0.5 mL/min for detection
Can be used for therapeutic approach, i.e., coiling
Indicated over EGD for hemobilia (bleeding from biliary tract)
Abdominal US +/- Doppler: For specific evaluation (i.e., liver dz or portal HTN)
In immune compromised consider assessment for CMV, HSV, or Candida esophagitis
Treatment
Acute management: Volume resuscitation w/ 2 large bore IVs, IV bolus w/ NS or LR, transfusion, if present correct coagulopathies (FFP, platelets)
UGIB: Basically 2 sources (1) Mucosal (-itis, ulcers, Mallory-Weiss) (2) Variceal
Mucosal: Neutralize/decrease acid production (PPIs > H2RA); w/ Mallory-Weiss can coagulate w/ thermal probe or inject dilute epinephrine
Variceal: Acute bleeding stops spontaneously in 50% w/ rebleed in 40%
Stop bleeding (band ligation > sclerotherapy by risk profile)
Decrease portal pressure and splanchnic blood flow: octreotide > vasopressin
LGIB: Etiology specific (stool softeners for fissure, Abx for infectious colitis)
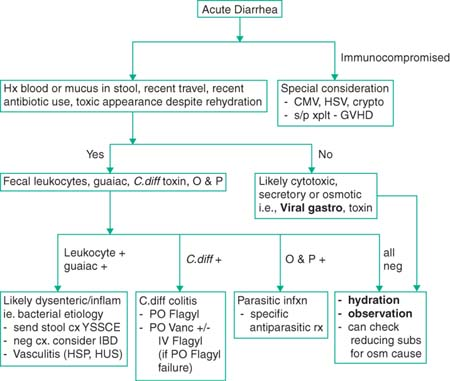
Acute Diarrhea
Definition
(Pediatr Rev 1989;11:6)
> nml stool output (>10 cc/kg/d), usually ↑ # BMs/d; WHO crit >3 stools/d.
Young infants have intestinal mucosa permeable to water; have greater net fluid loss.
80% fluid absorption at small bowel; processes affecting SB have rapid dehydration
Pathophysiology
(Arch Dis Child 1997;77:201)
4 basic processes: secretory, cytotoxic, osmotic, and inflammatory
Secretory: 2/2 infectious enterotoxin (cholera), metabolic/endocrine (hyperthyroid, VIPoma, ZES), or exogenous toxic agent (colchicines)
Enterotoxin → ↑secretion fluids/lytes via mucosal crypt cells or blocks villi absorp
Cytotoxic: 2/2 destruction of mucosal cells of small intestine, generally 2/2 viral infection (rota, Norwalk), similar underlying changes in celiac disease
Osmotic: Seen in malabsorptive conditions, unabsorbed substance in lumen reaches osmotically active concentration causing water influx. (i.e., lactose intolerance)
Determined by fecal osmotic gap (FOG) = serum osm – 2(stool Na + stool K)
FOG >100–120 is osmotic diarrhea; use serum osm to avoid error 2/2 transit time. If serum osm unavailable, can use stool Osm but less accurate
Inflammatory: 2/2 damage to intestinal lining w/ bloody stools, fecal leukocytes, and tenesmus, generally involves large intestine and terminal ileum
Invasive organisms: Yersinia, Campylobacter, Salmonella, Shigella, EHEC
History
Hx recent consumption raw milk, salad, undercooked meat/poultry, unpurified H2O, recent Abx, immunocompromise, sick contacts, FHx GI dz (IBD), blood in stool
Clinical Manifestation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree