Trey and Davidson [1]
England [10]
France [13]
International Association for the Study of the Liver 15
Acute liver failure (occurrence of HE within 4 weeks after onset of symptoms) [11]
Fulminant hepatic failure: development of HE within 8 weeks of onset of symptoms
Acute liver failure (includes only patients with encephalopathy)
Acute hepatic failure: a rapidly developing impairment of liver function
Subclassification
Acute liver failure, hyperacute: within 10 days
Acute liver failure, fulminant: 10–30 days
Acute liver failure, not otherwise specified
Subclassification depending on the interval between jaundice and HE
Severe acute hepatic failure: prothrombin time or factor V concentration below 50 % of normal with or without HE
Subacute liver failure (development of ascites and/or HE from 5 to 24 weeks after onset of symptoms)
Subclassification by etiology
Hepatitis A–E
Other viruses
Hyperacute liver failure: 0–7 days
Subclassification
Fulminant hepatic failure: HE within 2 weeks of onset of jaundice
Acute liver failure: 8–28 days
Subfulminant hepatic failure: HE between 3 and 12 weeks of onset of jaundice
Subacute liver failure: 29–72 days
Late-onset acute liver failure: 56–182 days
Hepatic encephalopathy usually sets in fulminant hepatic failure in all classifications and has transition from a severe condition to a deadly disease. The interval between the onset of symptoms or jaundice and the appearance of encephalopathy enables grouping of patients with similar etiologies, clinical characteristics, and prognosis. Liver disorders in pregnancy encompass a wide spectrum, but FH is the condition which has the most alarming and devastating course.
Acute liver failure is a broad term that encompasses both fulminant hepatic failure and subfulminant hepatic failure (or late-onset hepatic failure). Fulminant hepatic failure is generally used to describe the development of encephalopathy within 8 weeks of the onset of symptoms in a patient with a previously healthy liver. Subfulminant hepatic failure is reserved for patients with liver disease for up to 26 weeks before the development of hepatic encephalopathy.
Etiology
The most common etiology implicated in FH is viral hepatitis. The viruses have different geographic distribution. Thus, hepatitis B virus (HBV) is a common cause of FHF in the Far East, and hepatitis E virus (HEV) is relevant in India [14].
Studies carried out in India, Iran, Africa, and the Middle East have found the incidence of fulminant hepatitis to be higher in pregnancy [3, 4].
Occurrence of FHF within the larger number of patients with viral hepatitis, however, is rare (0.2–0.4 % for hepatitis A, 1–4 % for hepatitis B) [15]. Pregnant women infected by HEV seem to have a special propensity for developing FHF.
Epidemiology
Hepatitis E virus infection is highly endemic in certain countries. It causes frequent waterborne outbreaks and around 50 % of all cases of acute viral hepatitis in many countries and is contributed by factors like rapid urbanization, with limited access to safe drinking water and food and proper sanitation, which subsequently augments the risk of these infections. Thus, hepatitis viruses have a significant disease burden in the Southeast Asia Region, in the form of both acute and chronic hepatitis, with approximately 500,000 deaths annually in the region. Available data from the region on rates of infection with hepatitis viruses, rates of clinical disease caused by these viruses, and the associated morbidity and mortality are limited and may not reflect the true picture. Also the data available on the social and economic impact, expenditure on medical care, etc., of these infections in the region is not available [12].
Hepatitis E is caused by infection with the hepatitis E virus (HEV), a non-enveloped, positive-sense, single-stranded RNA virus [16–18], with four genotypes, 1, 2, 3, and 4. Each HEV genotype appears to have a specific geographic distribution. Genotype 1 HEV has been isolated from human cases of epidemic and sporadic hepatitis E in parts of Asia and Africa, where the disease is highly endemic. Outbreaks of HEV infection of up to several hundred to several thousand persons have been reported frequently in the Indian subcontinent, China, Southeast and Central Asia, the Middle East, and northern and western parts of Africa [2, 19].
Hepatitis E outbreaks are characteristically associated with a high disease attack rate among pregnant women. Further, affected pregnant women are more prone to develop fulminant hepatitis [19–23]. Hepatitis E outbreaks are characteristically associated with a high disease attack rate among pregnant women. Further, the affected pregnant women are more likely to develop fulminant hepatitis (15–22 %) or to have a fatal outcome. Fulminant hepatitis E infection has been reported among 40.3 % of pregnant women who were coinfected with chronic hepatitis B [24–26].
Hepatitis E during pregnancy is also associated with prematurity, low birth weight, and an increased risk of perinatal mortality [22].
Hepatitis E
Self-limiting – the overall mortality rate in FHF is 1–3 %; in pregnant women the rate is 15–25 %.
Pathology
Encephalopathy
Hepatic encephalopathy is a reversible neuropsychiatric dysfunction associated with acute or chronic liver failure preceded by agitation, hyperkinesis, and delusions with rapid progression to coma.
Grades of encephalopathy
Grade I | Grade II – | Grade III – | Grade IV – |
Diagnosis in retrospect, mild personality changes, fine tremor | Mild obtundation, drowsiness, lethargy, tremor ++, asterixis | Stupor, somnolence, arousal to voice, tremor if cooperative, hyperreflexia | Coma, response to pain (A) or no response (B), posturing |
Precipitating factors include gastrointestinal bleeding, SBP, sepsis, drugs, dietary protein load, alkalosis, diuretics, dehydration, constipation, and azotemia.
Cerebral Edema
Cerebral edema is detected in 75 % of grade IV encephalopathy and is the leading cause of death. It occurs secondary to loss of cell membranes and BBB integrity. Cushing response, hypertonia, posturing, and brain stem respiratory patterns are late signs.
Coagulopathy
Decreased II, V, VII, IX, and X
Decreased PLT
FFP are of no value in absence of bleeding
Renal and CV
Distributive hemodynamic
Hypotension, decreased SVR
Hepatorenal syndrome
Oxygen Transport and Delivery
Severe peripheral shunting may result from peripheral PLT plugs, interstitial edema, and abnormal vasomotor tone – diminished O2 extraction.
Metabolic Changes
Hypoglycemia is common (defective gluconeogenesis, decreased glycogen stores); dextrose 10 % may be required.
Hypokalemia.
Hyponatremia.
Hypophosphatemia.
Infections
Risks – decreased level of consciousness, immunocompromise (diminished opsonic activity, PMN function, phagocytosis, impaired CMI, humoral immunity). Portosystemic collaterals allow bacteria to bypass the hepatic reticuloendothelial system. Bacteremia and fungemia are common. Patients with GPC (S. aureus and epidermidis, strep) and GNR infection do not benefit from prophylactic ATB but empiric broad-spectrum antibiotic therapy is indicated if there are signs of sepsis. Pneumonia and UTI were the most common signs of infection; bacteremia was documented in 26 % of patients.
Pathologenesis
The mechanism of severe liver injury in pregnant women with hepatitis E is not known.
Immunological Factors
The immunological changes during pregnancy are of such nature that they help the rejection of the fetal allograft by suppressing T-cell-mediated immunity. The cellular immunity clearly alters the ratio of Th1/Th2 cell with definite increase in Th1 than Th2 which is the reverse occurring in normal pregnancy. This increase in Th2 is required for the survival of the fetus and thus explains the higher fetal morbidity observed in fulminant hepatitis. When HEV infection occurs, a cytotoxic immune response (Th1) is likely to be elicited in the Th2-biased pregnant women. Fulminant hepatic failure is always associated with high HEV load. For that a strong Th1 response is required. If this elevated Th1 immune response remains insufficient to fight with such a high HEV load, there is a possibility that Th1 response goes on increasing, but in the due process, the cytotoxic immune response may result in reduced fetal protection and eventually fetal demise. Opinions differ over the maternal and fetal outcome of pregnancies associated with viral hepatitis. Poor prenatal care and maternal nutrition appear to have contributed significantly to the increased severity of infection.
Hormonal Factors
Viral replication is promoted in pregnancy due to the high levels of steroid hormones. The direct inhibition on hepatic cells predispose to hepatic dysfunction/failure when exposed to infectious pathogens [27]. Steroid hormones are immunosuppressive [28] Figs. 8.1, 8.2 and 8.3.
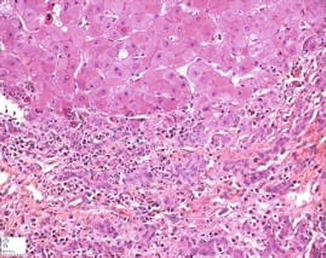
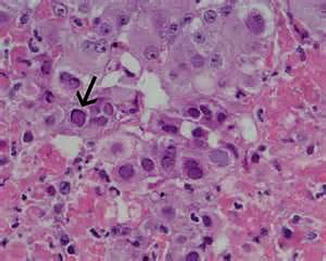
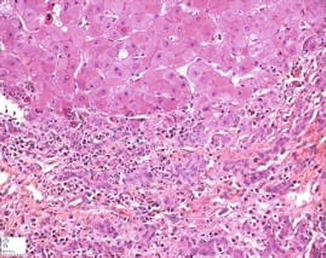
Fig. 8.1
FHF
Fig. 8.2
Submassive hepatic necrosis,3 FHF
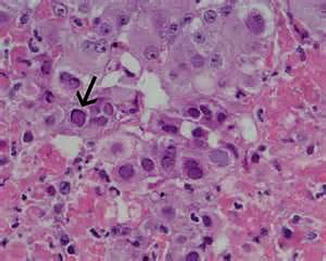
Fig. 8.3
Pathogenesis of severe hepatic injury in hepatitis E
Management of Fulminant Hepatitis
The management of fulminant hepatic failure demands the availability of a critical care setup and the involvement of critical care specialists. In normal pregnancy the liver is difficult to palpate due to the enlarged uterine size and also the signs of liver pathology like telangiectasia and palmar erythema may be observed in 60 % of normal pregnancies, the hormone estrogen being the cause for the same.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


