Fragile X Syndrome
Randi Hagerman
I. Description of the problem. Fragile X syndrome (FXS) is the most common inherited form of mental retardation. It causes a spectrum of developmental problems, ranging from learning disabilities and emotional problems (in those with a normal IQ) through all levels of mental retardation. The fragile X premutation can also be associated with developmental problems including attention-deficit/hyperactivity disorder (ADHD) and social deficits in addition to problems with tremor and balance difficulties in aging.
A. Epidemiology.
Causes intellectual disability in approximately 1 in 2500-4000 in the general population.
Responsible for approximately 20%-30% of all cases of X-linked mental retardation.
Approximately 1 in 130-259 females and 1 in 250-810 males in the general population carry the premutation (55-200 CGG repeats).
No known racial or ethnic differences; identified in all racial groups tested.
Both males and females can be unaffected carriers although ADHD, anxiety, and social deficits including autism spectrum disorders (ASDs) can occur in premutation carriers. Approximately 40% of older male carriers and 16% of older female carriers can develop the fragile X-associated tremor ataxia syndrome (FXTAS). Primary ovarian insufficiency (POI) occurs before 40 years of age in about 20% of female carriers.
B. Genetics. FXS is caused by a mutation in the fragile X mental retardation-1 gene (FMR-1), which is located on the bottom end of the X chromosome. The mutation causes a fragile site or break in the chromosome at that location. The FMR-1 gene was identified and sequenced in 1991. An unusual expansion of a cytosine, guanine, guanine (CGG) nucleotide repetitive sequence was found to be the mutation. Within the FMR-1 gene, normal individuals have a nucleotide CGG sequence that repeats up to 45 times, carriers with a premutation have an expansion of the CGG sequence between 55-200 repeats, and individuals affected with FXS have a CGG repeat number greater than 200 (termed a full mutation). When this occurs, the gene usually becomes methylated or turned off so that little or no FMR-1 protein (FMRP) is made, and the full FXS occurs.
A carrier male will pass only X chromosome to all of his daughters, who will be obligate carriers and pass the mutation to 50% of their offspring. A significant expansion of the mutation will often occur in their children so that males and females with intellectual disability are common. A detailed family tree must be drawn to sort out possible carriers and other extended family members who may be affected by FXS or by premutation involvement including FXTAS and POI.
II. Making the diagnosis. Both behavioral and physical features are included in the fragile X checklist (Fig. 45-1), which serves as a reminder for clinicians of the signs and symptoms of FXS.
A. Signs and symptoms in males.
1. Early signs and symptoms.
Infants with FXS may appear to be normal, although behavior and feeding difficulties have been described including recurrent vomiting.
Recurrent otitis media begins in the first year of life for the majority of males affected by this syndrome.
Hypotonia is also notable in young boys, with subsequent mild delays in motor milestones.
Most boys with FXS and significantly affected girls with fragile X are delayed in the onset of language. Phrases or short sentences are usually delayed until the age of 3 years or older. The language delays in addition to hyperactivity or tantrums are the typical initial concerns leading to medical consultation.
Prominent ears with occasional ear cupping, hyperextensible finger joints, double-jointed thumbs, flat feet, and soft skin are seen in the majority of boys
with fragile X in early childhood. These physical findings are considered to be part of a connective tissue dysplasia that is related to the absence of FMRP.
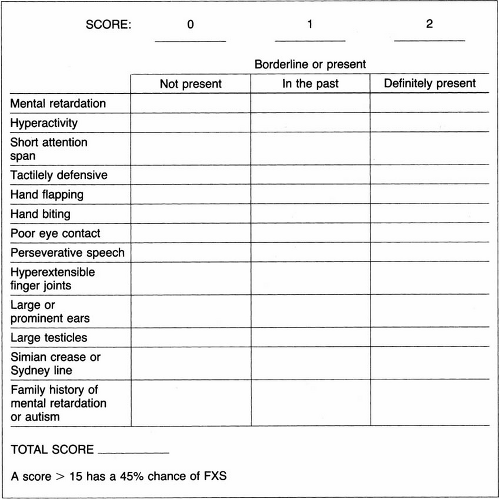
Figure 45-1. Fragile X Checklist. (Modified from Hagerman RJ, Amiri K, Cronister A. Fragile X checklist. Am J Med Genet 38:283-287, 1991.)
Young boys with FXS may also have a broad or prominent forehead and a large head circumference.
2. Later signs and symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


