Fig. 1
A nine-year-old female sustained a Monteggia fracture dislocation (plastic deformation of the ulna and radial head dislocation, AP-a and lateral-b). Reduction of the radial head was achieved by correction of the ulnar bowing using an osteotomy and plate fixation (AP-c and lateral-d)
Greenstick Fracture
In greenstick fractures, one to three cortices may be disrupted on radiographs. The remaining cortex is in continuity but is angulated (Fig. 2). A torsional force is typically involved with the mechanism of injury; therefore, displaced greenstick fractures nearly always have a rotational component. Apex dorsal fractures are caused by hyperpronation, and apex volar fractures are due to hypersupination during the injury. The intact cortex helps to maintain length of the fracture and facilitates reduction.
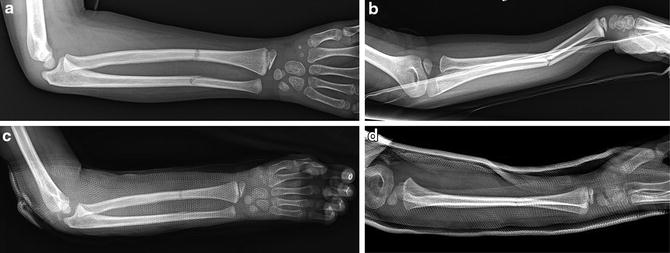
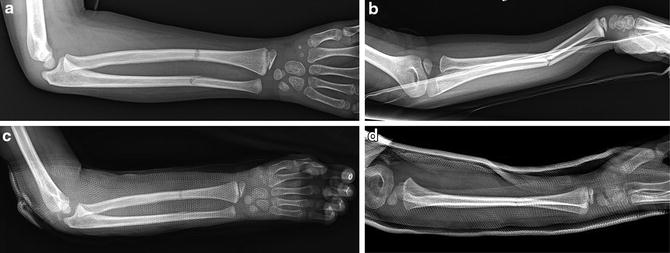
Fig. 2
A seven-year-old male fell from a standing height and sustained a greenstick both-bone forearm fracture (AP-a and lateral-b). The remaining cortex is in continuity but is angulated. A torsional force is typically involved with the mechanism of injury; therefore, greenstick fractures usually have a rotational component associated with the angulation. The patient underwent closed reduction and application of a sugar-tong splint (AP-c and lateral-d)
Complete Fractures
Complete fractures occur when all cortical contact is lost between two fragments of bone. These fractures are further described by the fracture pattern. Transverse and short oblique non-comminuted fractures of the radius and ulna are most common in pediatric patients. Comminuted and segmental fractures are relatively uncommon, as they result from high-energy mechanisms. The most difficult fractures to reduce and cast in acceptable alignment, i.e., the most unstable fracture patterns, are both-bone complete forearm fractures. The degree of displacement of complete fractures reflects the severity of the injury and the amount of soft tissue disruption that occurs. Complete fractures may remain reasonably aligned if the periosteum and muscle attachments are not completely disrupted and stripped from the bones at the sites of fracture.
Fracture Displacement: Angulation, Translation, and Malrotation
The displacement of forearm fractures is described based on radiographic measurements of the AP and lateral radiographic projections. Angulation is determined by measuring the angle created by the fracture fragments at the apex of the deformity and is assessed separately for each bone and in orthogonal planes. Translation quantifies the amount of cortical or bony contact between the fragments. Fragments may have a percentage of bone contact, or they may be completely translated relative to one another with no end-on cortex-to-cortex contact. Additionally, fragments with no contact that then rest overlapped one on top of another are said to be in “bayonet apposition,” a reference to the shape of the swordlike weapon (Fig. 3). The degree of shortening of each bone may then be determined by measuring the length of cortical overlap.


Fig. 3
A twelve-year-old male fell while skateboarding and sustained a distal third both-bone forearm fracture which was completely translated and shortened in “bayonet apposition” (AP-a and lateral-b)
Malrotation is more difficult to assess. Fracture fragments that are not malrotated relative to each other appear on radiographs to have similar diameters in both the AP and lateral projections. A more reliable way to assess rotation is to compare the relative positions of the bicipital tuberosity of the radius proximally and the radial styloid distally as viewed on an AP radiograph with the forearm neutrally rotated. In the normal radius, the bicipital tuberosity and the radial styloid point 180° from each other. The degree of malrotation can be estimated based on the radiographic appearance of these landmarks.
Outcome Assessment
Many studies define outcomes based on radiographic alignment of the fracture at healing and by the clinical outcome, typically determined by measuring forearm range of motion and the occurrence of complications. In order to determine more consistently the effectiveness of forearm fracture treatment methods, Flynn et al. proposed the Children’s Hospital of Philadelphia Forearm Fixation Outcome Classification. In this classification, the results of fixation may be labeled as being “good,” “fair,” or “poor.” A “good” outcome is classified as being one where the child has full range of motion (<10° loss of supination and/or pronation) and no postoperative complications. A “fair” outcome is defined as the child having minimal loss of range of motion (<30° supination and/or pronation) and/or minor, resolving postoperative complications. A “poor” outcome occurs with loss of range of motion (>30° supination and/or pronation) and/or major postoperative complications, such as infection, compartment syndrome, or delayed union (Flynn et al. 2010).
Another similar outcome assessment was described by Price et al., with categories being labeled as “excellent,” “good,” “fair,” or “poor.” To be classified as “excellent,” the patient must have no complaints and a loss of range of motion <10°. “Good” results include those having mild complaints with vigorous activity and loss of motion between 11° and 30°. A result is recorded as “fair” if complaints occur with daily activities and loss of motion is between 30° and 90°. If complaints are more severe or there is greater loss of motion, the outcome is considered “poor” (Price et al. 1990).
Nonoperative Treatment
Most pediatric forearm fractures are best treated with closed reduction and long-arm cast immobilization (Zionts et al. 2005; Jones and Weiner 1999). In one study of over 730 forearm fractures, of which 300 were displaced significantly, only 22 failed initial closed reduction and casting (Jones and Weiner 1999). The trend toward operative fixation over the last 15 years has helped to define operative indications. Surgical treatment is indicated as the primary treatment for those patients with open fractures, vascular injuries, a “floating elbow,” and severe soft tissue complications such as a compartment syndrome or tissue loss. Only after an unsuccessful attempt at closed fracture management is surgery indicated for the remainder of patients, with few exceptions. Certain fractures have a high risk of closed treatment failure including displaced proximal third radius fractures, displaced fractures in children over 10 years of age, and mid-diaphyseal fractures with initial ulnar angulation greater than 15° (Bowman et al. 2011). An attempt should be made to treat children and adolescents with forearm fractures nonsurgically at the outset, even if they fall into these “risk of failure” categories.
Nonoperative Management of Forearm Fractures | |
|---|---|
Indications | Contraindications |
An attempt should be made to treat children and adolescents with forearm fractures nonsurgically | Vascular injury |
Open fracture | |
Compartment syndrome | |
Severe soft tissue injury | |
“Floating elbow” | |
Emergency Department Management
Closed reduction and immobilization of forearm fractures is the preferred treatment option. After adequate patient assessment and review of the radiographs, the surgeon must define the degree of displacement. Children with nondisplaced or minimally displaced fractures are placed into a long-arm cast or a sugar-tong plaster splint with the elbow flexed 90° and neutral rotation of the forearm. Sedation is rarely needed and patients are discharged from the emergency department after fracture care instructions are given to the child and the family.
Analgesia/Sedation
Intravenous ketamine provides excellent sedation and analgesia enabling a closed reduction . This method induces a trancelike state that combines sedation, analgesia, and amnesia with little cardiovascular depression (McCarty et al. 1999). Intravenous conscious sedation methods are effective for closed fracture management but demand an experienced sedation team and safety protocols. Complications, such as an adverse reaction, can occur with sedation. Therefore it is mandatory the emergency department staff be trained to properly dose medications based on the child’s weight, the use of pediatric cardiovascular monitoring, and, most importantly, resuscitation techniques (Cameron et al. 2000). Other methods of analgesia for upper extremity fracture management include alternative intravenous sedation drug regimens, such as fentanyl-midazolam, and regional anesthetic techniques, such as a Bier block or axillary block. A hematoma block may be plausible for distal forearm fractures; however, this technique is less effective for proximal fractures. Also, children may be anxious and/or uncooperative, making it a challenge to inject the fracture site. One report utilized inhaled nitrous oxide to obtain sedation, and then a hematoma block was performed allowing for fracture reduction (Hennrikus et al. 1995).
Fracture Manipulation
Plastic Deformation
Fractures that are plastically deformed with an unacceptable degree of angulation can typically be managed in the emergency department. After adequate sedation and analgesia has been provided, the fractured forearm may be gently manipulated straight by three-point bending forces centered at the apex of the deformity. For small children, the physician places his or her thumb at the apex and applies steady pressure at the ends of the bone. Alternatively, a rolled towel or cushioned bump is placed on the stretcher, and the apex of the deformity is placed on top of it, allowing the physician to apply downward pressure at the bone ends and gently rock the fracture around the fulcrum over a period of 3–5 min to achieve correction (Fig. 4). The goal is not to complete the fracture but instead to restore alignment, ideally achieving anatomic alignment but generally no more than 15–20° of residual angulation (Vorlat and De Boeck 2003). After reduction, a three-point molded long-arm cast is applied. If the fracture does not reduce, operative reduction under anesthesia, either with the above technique or by percutaneous drill osteoclasis at the apex of the deformity, may be indicated (Blackburn et al. 1984).
Fig. 4
Plastic deformation of the forearm may be reduced by applying gentle pressure proximal and distal to the apex of the bow while the forearm rests on a bolster or bump that acts as the fulcrum for deformity correction (From Sanders and Heckman 1984b)
Greenstick Fractures
Similar to plastic deformations, greenstick fractures are usually treated with a closed reduction and well-molded cast placed under conscious sedation. In order to reduce these fractures, the force opposite to the mechanism of injury is applied. As greenstick fractures result predominantly from torsional forces that occur as the arm is axially loaded, reduction is often easily achieved by merely applying gentle traction and rotating the distal forearm and thumb toward the apex of the deformity (Noonan and Price 1998), often referred to as the “rule of thumbs.” Therefore, apex volar fractures are reduced by pronating the forearm while apex dorsal fractures are reduced by forearm supination. A topic of controversy when treating these fractures is whether or not the fracture should be completed. Advocates for completing the fracture argue that this will help prevent re-angulation or diminish the risk of refracture (Rang 1983). In contrast, many believe that the intact cortex helps maintain the alignment of the fracture after reduction (Alpar et al. 1981). After reduction, the arm is immobilized in a well-molded long-arm cast in neutral rotation with the elbow flexed 90°.
Complete Fractures
After adequate sedation and analgesia is achieved, longitudinal traction is applied to the forearm. This may be achieved by placing the fingers of the affected extremity in finger traps and suspending them from an intravenous pole. The weight of the arm provides a traction force allowing the fracture fragments to realign as muscle forces are overcome. Additional traction can be achieved by applying small weights to a cuff wrapped around the upper arm. Without cortical contact, the bone fragments are susceptible to displacement by muscle forces acting on the bone. Alternatively, an assistant may apply longitudinal traction across the fracture by grasping the upper arm proximally and the hand distally while the physician manipulates the bone fragments. Muscle forces influence rotation of the fragments and must be taken into account when reducing complete fractures to avoid malrotation (Fig. 5). Due to the forces of the biceps and supinator, complete proximal radius fractures are best immobilized in supination. In the middle third of the forearm, the rotational forces are relatively balanced so neutral rotation is appropriate. For fractures of the distal third of the forearm, the pronator quadratus is acting on the distal fragment. Therefore, these fractures are best reduced and held in some pronation. The forearm should not be placed in extreme positions of supination or pronation, as significant stiffness can occur after fracture healing. A fixed supination deformity from a contracture is particularly debilitating and a challenge to manage.
Fig. 5
Rotational displacement of the radius is caused by muscle forces acting proximal and distal to the fracture: (a) proximal fractures and (b) distal fractures (Adapted from Cruess, R.L. Orthop Clin North Am 1973; 4:969)
Immobilization After Reduction
Careful application of a well-molded circumferential cast after reduction is critical for maintenance of alignment and to prevent complications. If there is a concern for severe swelling, the cast is bivalved and overwrapped with an elastic bandage prior to discharge or the child is admitted and observed overnight. Alternatively, the child may initially be placed into a non-circumferential splint, such as a sugar-tong splint (Younger et al. 1997), and casted upon outpatient follow-up. The ideal long-arm cast applied to treat forearm fractures must have a three-point mold about the fracture sites and be oval in shape at the middle of the forearm with an indent between the radius and ulna to create an interosseous mold. The upper arm part of the cast should be tapered just above the supracondylar area of the humerus, and the ulnar and posterior humeral borders should be essentially flat to limit the distal migration or shifting in the cast (Fig. 6).
Fig. 6
Finger traps may be used to provide traction while the long-arm cast is applied. The ideal cast has an interosseous mold resulting in an oval shape in the mid-forearm combined with flat ulnar and posterior humeral borders
Acceptable Reduction
After cast application, high-quality AP and lateral radiographs are taken and analyzed. Acceptable reduction parameters vary based on the chronological age and, more importantly, the estimated years of growth remaining, the location of the fracture, and the postreduction alignment. The ideal reduction parameters that reliably yield satisfactory clinical results are controversial. Even small degrees of residual angulation have been correlated with some loss of forearm rotation (Alpar et al. 1981; Noonan and Price 1998; Kasten et al. 2003). In addition to bony malunion, soft tissue fibrosis, especially about the interosseous membrane, may lead to limited forearm motion after fracture healing (Nilsson and Obrant 1977). Angulation of the radius, especially when the radial bow has been lost, correlates with loss of forearm rotation while ulnar angulation has a greater influence on the cosmetic or aesthetic appearance of the forearm (Dumont et al. 2002). For children under the age of 8 years, up to 20° of diaphyseal angulation may remodel while angulation of as little as 10° may not in those older than 10 years of age (Jones and Weiner 1999). To confound the issue, residual radiographic angulation does not always have a direct correlation with functional outcomes and patient satisfaction (Price et al. 1990). Shortening is well tolerated in patients younger than 10 years of age, with up to one centimeter being acceptable after failed closed reduction (Do et al. 2003). Even fractures in bayonet apposition treated with casting and no analgesia, sedation, or a formal reduction can result in excellent clinical outcomes (Crawford et al. 2012).
Children Younger than 10 Years of Age
The recommended acceptable forearm reduction parameters for children younger than 10 years of age include residual angulation of the radius or ulna measuring 20° or less. There are two exceptions: radius fractures in the proximal third and radius fractures with apex ulnar angulation. Proximal radius fractures with angulation of 10° or more and radius fractures with any apex ulnar angulation are at risk of rotation loss even in this young age group. Complete translation, bayonet apposition with shortening of 1 cm or less, and malrotation less than 30° are other acceptable parameters of reduction.
Children 10 Years of Age and Older
Children who are 10 years of age and older have less capacity for fracture remodeling. Greater than 10° of angulation of either bone in any plane, greater than 50 % translation, shortening or bayonet apposition, and greater than 30° of malrotation are unacceptable reduction parameters. Individuals with less than 2 years of growth remaining have minimal remodeling capability; therefore, near-anatomic alignment must be obtained for acceptable reduction.
Complications of Nonoperative Treatment
Stiffness
The most common complication to occur after a forearm shaft fracture is significant forearm stiffness, with a decrease in pronation more common than loss of supination (Högström et al. 1976; Holdsworth and Sloan 1982). This most commonly occurs in patients with malunited fractures but may occur even after anatomic healing. Avoiding extreme positions of either pronation or supination in a cast and permitting motion as soon as fracture healing occurs are some ways to limit functional loss of rotation after cast treatment of forearm fractures.
Malunion
Malalignment after healing occurs in 10–25 % of patients (Davis and Green 1976). This complication is cast related and mostly due to poor molding after acceptable reduction. Occurrence of this complication can often be remedied by repeating the closed reduction and casting (Davis and Green 1976; Voto et al. 1990). A small percentage of children will experience a malunion, but the deformity is mostly cosmetic and may or may not cause loss of functional forearm motion (Daruwalla 1979). Close follow-up with serial AP and lateral radiographs within the first 2 weeks postreduction is critical to prevent this complication. Cast wedging may be used to improve unacceptable angulation if it is noticed in a timely manner. Osteotomies of the radius and ulna are salvage options for those patients with healed malunions (Price and Knapp 2006).
Refracture
Diaphyseal forearm fractures are the number one location of refracture in children, with most occurring at the original site (Landin 1997). Up to 8 % of patients will experience a refracture. Children are at highest risk for this complication up to 1 year following union of the initial fracture; refractures are much less common during splint wear (Chung and Spilson 2001). Most refractures occur in the proximal and distal third of the forearm (Baitner et al. 2007).
Uncommon Complications
Delayed union and nonunion are very rare complications. Nonunion occurs most commonly in the ulna in patients between 13 and 16 years old (Adamczyk and Riley 2005). Synostosis, although rare, may result in complete loss of forearm rotation. Compartment syndrome is rare after closed reduction and cast treatment of forearm fractures but must be suspected if a child is not comfortable 3–4 hrs postreduction (Crawford 1991). A non-circumferential splint may be applied or the cast may be bivalved. The treatment for compartment syndrome is emergent fasciotomies. Finally, cast complications may occur. Skin breakdown, skin burns from hot dipping water, and cuts and/or burns from the cast saw occur but are easily preventable if proper techniques are utilized (Halanski and Noonan 2008). Refer to Table 1 for tips on safe fiberglass cast application.
Table 1
Pearls for safe and effective fiberglass cast application
Avoid excessive padding to enhance molding and reduce the risk of loss of fracture reduction |
Maintain joints in the same position while applying cast to avoid pressure points at joint creases |
Use cool dipping water to avoid excessive heat generation and potential burns under the cast |
Use stretch-relaxation of the fiberglass to avoid excessive cast constriction after cast curing |
Do not trim or bivalve fiberglass cast until it has cooled to avoid cast saw burns of the skin |
Part B: Operative Treatment
Indications
Fractures of the forearm are typically treated successfully with closed reduction and cast immobilization. Surgical treatment is indicated for open fractures (Greenbaum et al. 2001; Luhmann et al. 2004), severe soft tissue injury or compartment syndrome , vascular injuries, and floating elbow injuries (ipsilateral fractures of the distal humerus and forearm) (Ring et al. 2001). The inability to obtain acceptable alignment via a closed reduction necessitates surgical reduction and fixation. Also, unstable fractures that have lost alignment at follow-up may require repeat closed reduction or operative fixation.
Surgical Procedures
Options for surgical treatment include closed or open reduction and intramedullary nailing, open reduction and internal fixation utilizing plates and screws, and in rare circumstances external fixation. Intramedullary nailing has become the standard operative treatment method for skeletally immature patients and has demonstrated good results (Lascombes et al. 1990; Till et al. 2000; Flynn et al. 2010; Martus et al. 2013).
Intramedullary Nailing
Preoperative Planning
Intramedullary nailing can be done percutaneously or with minimal surgical exposure using flexible nails (1.5–2.5 mm diameter) or smooth wires/pins (0.062 or 5/64th inches diameter). The nail diameter should fill approximately two thirds of the canal isthmus. The implant is advanced across the fracture site via a closed or limited open reduction. Dual bone fixation is most common, but occasionally single-bone fixation provides adequate stabilization of the fracture reduction.
Positioning
The patient is positioned supine and general anesthesia is provided. A radiolucent hand table is used to support the operative extremity. A non-sterile pneumatic tourniquet is placed on the upper arm, ensuring access to the elbow. The extremity is then draped and prepped in sterile fashion including the elbow, forearm, and hand. Fluoroscopy is stationed at the distal end of the hand table. Prior to draping, the adequacy of imaging should be assessed (Table 2).
Table 2
Preoperative planning for intramedullary nailing of radius and ulna shaft fractures
OR table | Standard OR table with radiolucent hand table on operative side |
Position | Supine with the patient located close to the edge of the OR table to provide sufficient mobilization of the operative extremity and unobstructed fluoroscopic visualization |
Fluoroscopy | Positioned at the distal end of the hand table |
Tourniquet | Non-sterile; placed on upper arm close to the axilla |
Draping | Ensure the elbow, forearm, and hand are accessible |
Equipment | (a) Flexible nails (1.5–2.5 mm diameter) or smooth wires (0.062 or 5/64th size) |
(b) Drill or awl | |
(c) T-handled chucks | |
(d) Nail bender | |
(e) Small fragment set if open reduction is needed |
Approach
Antegrade and retrograde intramedullary nailing techniques have been described for the ulna, while retrograde nailing is standard for the radius. The order of bone fixation is variable between surgeons and may be determined based on which bone is the most difficult to reduce and most unstable. The ulna is the first bone to be nailed, as it is classically easier to reduce.
Technique
Antegrade nailing is utilized for the ulna , with insertion across the olecranon apophysis. The antegrade insertion site is directly posterior to the olecranon, which provides a direct path to the canal. Alternately, insertion can be done through the metaphysis just distal to the apophysis on the lateral aspect of the ulna (anconeus starting point). Significant complications have not been reported with either entry site.
The tourniquet can be kept deflated during fixation of the ulna if an open reduction is not required. A small incision is made over the tip of the olecranon process. Fluoroscopic guidance is used to drill a starting hole across the apophysis into the intramedullary canal. A flexible nail is inserted using a T-handled chuck. Alternatively, if a smooth wire/Steinmann pin is used, the sharp end can be used to drill the starting point and then advanced. The nail or wire is positioned just shy of the fracture site; traction is applied and a closed reduction obtained. The implant is moved past the fracture site until the far tip terminates in the distal metaphysis of the ulna. Sufficient length should be allotted for the implant to be tamped into final position, ensuring it does not violate the distal physis of the ulna. This is done by advancing the nail to its final position and then withdrawing it 1–2 cm. The nail is cut to the appropriate length and gently readvanced to its final position. The cut proximal end should terminate beneath the skin. Some surgeons may elect to leave the implant percutaneous for early removal in the office setting, but this can be challenging for younger patients (Table 3).
Table 3
Surgical steps for intramedullary nailing of the ulna
Flex the elbow to 90° |
Fluoroscopy used to confirm location of apophyseal starting point – in line with intramedullary canal of the ulna |
1 cm longitudinal incision over olecranon followed by blunt dissection down to bone |
2.7 or 3.2 mm drill or awl used to penetrate the cortex |
Insert nail using T-handled chuck and advance to fracture site |
Combine traction and rotation, also anterior/posterior compression if needed, to obtain reduction |
Advance nail past fracture to appropriate length in distal ulna |
Confirm ulnar styloid and coronoid process are 180° from each other on full-length lateral fluoroscopic image |
Withdraw the nail 1–2 cm, cut the nail leaving 1–2 cm proud, and then impact the nail to final position |
Close the skin with absorbable sutures and apply Steri-Strips |
Attention is then directed to the radius , which is fixed in a retrograde fashion. If the tourniquet has yet to be inflated, the limb is exsanguinated and the tourniquet is inflated. The dorsal physeal sparing entry site is located at the proximal aspect of Lister’s tubercle. This location is approached utilizing a 1–2 cm longitudinal incision approximately 1 cm proximal to the distal radial physis in the midline of the metaphysis between the third and fourth dorsal extensor compartments. Fluoroscopy may be used to confirm proper placement of the incision proximal to the physis. Dissection is continued through the retinaculum, and the interval between the third and fourth dorsal extensor compartments is used to expose the distal radius at Lister’s tubercle. Transposition of the extensor pollicis longus tendon may be necessary for a safe starting point. Alternatively, a lateral entry point may be used via the floor of the first dorsal extensor compartment. An awl or drill is used to create a unicortical entry hole after fluoroscopic verification of the planned insertion position. The hole is enlarged at a 30° angle by directing the drill or awl proximal obliquely across the radius. Once the starting point has been created, the flexible nail or smooth wire is pre-contoured to a gentle “C” shape to accommodate the radial bow. Direct visualization of the bone surface is needed to prevent tendon injury during insertion and advancement. The implant is positioned just shy of the fracture site. A closed reduction is performed, and the nail is moved across the fracture ensuring the contour of the nail is aligned with the bow of the radius. The nail should be advanced to its final position short of the radial neck physis. Subsequently, the nail is withdrawn 1–2 cm, cut to its proper length and tamped into final position. It is important to verify the cut end is not abrading the extensor tendons. Once the tendons are visualized as being away from the cut nail, the incision is closed with the implant tip beneath the skin (Table 4). A nail or wire placed using a lateral starting point can be left percutaneous for office removal. Figure 7 exemplifies a standard both-bone forearm fracture treated with flexible intramedullary nails, and Fig. 8 demonstrates a similar fracture treated with K-wire fixation using a radial styloid starting point.
Table 4




Surgical steps for intramedullary nailing of the radius
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


