Forceps Delivery
Using forceps for operative vaginal delivery is increasingly less common. While many of today’s young obstetricians are taught techniques of ultrasonography, they may be poorly trained in forceps use and unfamiliar with the indications, risks, and possible complications of operative vaginal delivery (Gilstrap, 1994). The reclassification of the use of forceps by the American College of Obstetricians and Gynecologists in 1988, as well as subsequent studies showing that the new classification accurately stratifies risk for both mother and fetus (Hagadorn-Freathy and associates, 1991), should serve as an impetus for continued and even increased use of forceps under appropriate clinical conditions.
PRACTICE OF FORCEPS DELIVERY
Use of obstetric forceps has been controversial since their invention. William Smellie in 1752 recommended using forceps in his Treatise on the Theory and Practice of Midwifery. The instrument then became widely available and was used by unskilled practitioners, resulting in injury to mother and child. By the early nineteenth century, forceps had been almost abandoned, but the case of Princess Charlotte in 1817 figured in their reemergence (Holland, 1951). The princess had a 24-hour second stage of labor. Her obstetrician, Sir Richard Croft, was the son-in-law of Sir Thomas Denman, one of the most influential physicians in England. One of Denman’s maxims was that instrumental delivery not be attempted until the fetal head had rested on the perineum for 6 hours. Ultimately, through delay and questionable advice from a consultant, the never-to-be prince remained on the perineum for 10 hours and was stillborn. The princess died of a postpartum hemorrhage, and the inconsolable Dr. Croft committed suicide 6 weeks later. The consensus was that this “triple obstetric tragedy” could have been avoided by a timely forceps delivery.
This event in part accounted for a resurgence in forceps use that lasted for more than 100 years. The development of obstetric anesthesia in the mid-nineteenth century further increased the popularity of forceps and patient acceptance. The concept of the prophylactic use of forceps, introduced by DeLee (1920), contributed to a nearly 70 percent incidence of forceps deliveries by the late 1940s. Since this record-high incidence, the more difficult forceps deliveries have prudently been eliminated in favor of cesarean section. This trend has continued to the present; but along the way, many not-very-difficult forceps deliveries also were abandoned. Furthermore, the liberal use of cesarean section in the first stage of labor has led to a generation of obstetricians inexperienced and uncomfortable with forceps use. For example, in a recent survey of residency and fellowship training program directors, Hankins and colleagues (1999) reported that although these directors taught and expected proficiency in outlet and low-forceps operations, they did not expect proficiency in midforceps delivery. Ramin (1993), Bofill (1996), and their colleagues also reported a significant decline in operative vaginal deliveries, especially midpelvic deliveries. This is despite the economic cost, the morbidity of cesarean delivery, and that the minimal fetal morbidity of properly selected cases had refocused attention on operative vaginal deliveries (Hagadorn-Freathy and associates, 1991).
MODERN FORCEPS INSTRUMENTS
In the last 200 years, the design of the basic instrument has changed only slightly. Although over 600 varieties of forceps have been catalogued, only a few features are important, and these can be obtained with the use of relatively few basic instruments, which are described in this chapter.
ANATOMY OF THE FORCEPS
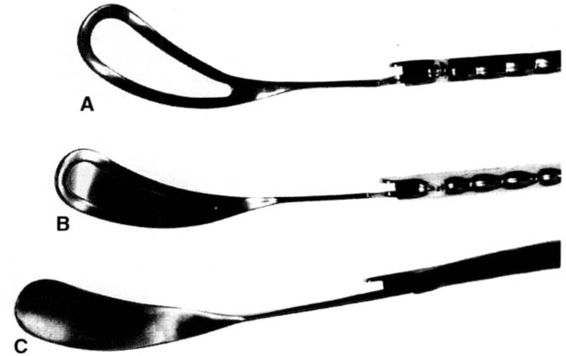
Except when used at cesarean delivery, obstetric forceps are a paired instrument. The two members are customarily referred to as the left and right blades. However, because each distal end of the forceps is also referred to as a blade, we use the less common terms left branch and right branch throughout this chapter. The left branch is grasped by the operator’s left hand and applied to the left side of the maternal pelvis, while the right branch is grasped by the right hand and introduced into the right side of the maternal pelvis. Prior to the application of the forceps, they should be examined for symmetry. In addition, the operator should ascertain that the blades are a matched set by examining the inside of the handle of the instrument: the Arabic numerals on each blade should be identical. Both the right and left branch of the forceps can be further subdivided into four parts: handle, lock, shank, and blade (see Fig. 6-1). Some forceps, such as the DeLee, are fitted with an additional device known as an axis-traction bar (see Fig. 6-2). While each half of the forceps is customarily referred to as a left or right blade, the “blade” is actually limited to the widened, curved portion that is applied to the head of the fetus. As shown in Figure 6-3, forceps blades may be either fenestrated (Simpson), pseudofenestrated (Luikart-Simpson), or solid (Tucker-McLane). The open blades facilitate traction but are prone to injure maternal soft tissue if significant degrees of rotation are required. In contrast, solid blades are well designed for rotation; they cause less maternal soft tissue injury, but increase the risk of slippage on the fetal head.
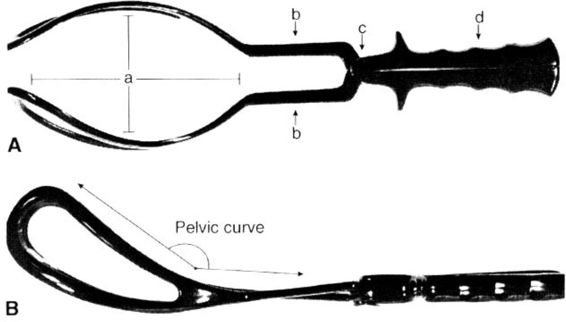
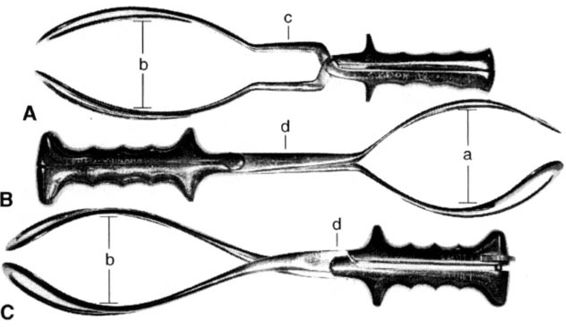
FIGURE 6-1. A. Simpson forceps as viewed from above demonstrating the cephalic curve of wide radius (a), parallel shanks (b), English lock (c), and corrugated handles (d). B. Lateral view of Simpson forceps. Note the upward curve of the blade of the forceps from the shank of the forceps such that the anterior tip of the toe of the forceps rests well above the handle of the forceps.
FIGURE 6-2. A Bill axis-traction device. This device is designed so that it will fit on the handle of many forceps including the Simpson, Luikart-Simpson, Elliot, and Bailey-Williamson forceps. When properly used, the hinge adjoining the handle to the arm extending to the forceps will be at approximately a 90-degree angle.
Articulated, the forceps present two curves in planes at right angles to each other. The curve that corresponds to the fetal head is known as the cephalic curve (see Figs. 6-1 and 6-4), which varies from one forceps to another. The cephalic curve should be well shaped and measure approximately 7.5 cm in its widest diameter. All forceps can be subdivided into two groups. The first consists of elongated and bayonet-shaped blades with a shallow curve, which is well suited for application to the molded head. The Simpson forceps and the DeLee forceps are examples of instruments ideally suited for delivery of the molded head (Figs. 6-1 and 6-5). The second grouping of forceps has a shorter and more rounded cephalic curve and is ideal for delivery of the fetal head with little or no molding. The Bailey-Williamson forceps are excellent in this clinical setting (Fig. 6-5).
FIGURE 6-3. Forceps demonstrating A. a fenestrated blade (Simpson); B. pseudo fenestrated blade (Luikart-Simpson); and C. solid forceps blade (Tucker-McLane).
FIGURE 6-4. The Kielland forceps as viewed from above. The cephalic curve has a wide radius. The shanks overlap (a) and are connected by a sliding lock (b). The two elevations (c) on the handle near the finger guards serve for orientation of the forceps and are usually directed toward the fetal occiput.
FIGURE 6-5. Top view of A. Simpson, B. Bailey-Williamson, and C. Elliot forceps. Note the more rounded cephalic curve of the Bailey-Williamson forceps (a) relative to the Simpson (b) or the Elliot forceps (b). Also note the parallel shanks of the Simpson forceps (c) as compared to the overlapping shanks of the Bailey-Williamson or Elliot forceps (d).
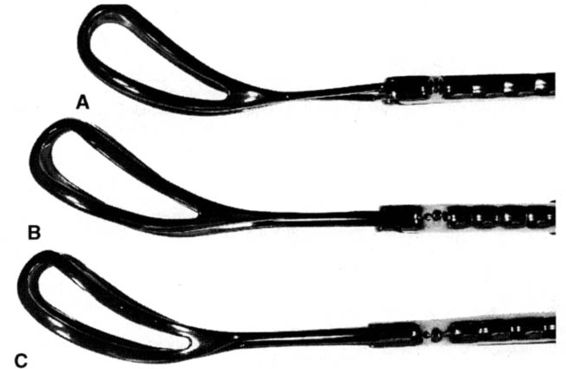
The second curve of the forceps, which corresponds to the curve of the pelvis, is known as the pelvic curve. In conventional forceps, the pelvic curve is directed upward so that when the forceps are applied to the fetal head presenting in an occiput anterior (OA) position, the curve of the instrument approximates the pelvic curve of Carus (Fig. 6-6). The tips of the blades of classical instruments, such as the Simpson and Elliot forceps, rise from 2.75 to 3.5 inches above the level of the handles (Fig. 6-7). When the head lies in a transverse position, however, as frequently occurs with midpelvic arrest, the pelvic curve is no longer desirable. The Kielland forceps were designed so that the pelvic curve is almost entirely eliminated (Fig. 6-4). In contrast, Piper forceps have a reverse pelvic curve (Fig. 6-8).
FIGURE 6-6. The cavity of the true pelvis is comparable to an obliquely truncated, bent cylinder with its greatest height posteriorly. Note the curvature of the pelvic axis, the curve of Carus.
FIGURE 6-7. Lateral view of the A. Simpson, B. Bailey-Williamson, and C. Elliot forceps demonstrating the pelvic curve.
FIGURE 6-8. Piper forceps in lateral projection. Notable is the reverse pelvic curve of these forceps. Accordingly, axis-traction generally is in line with and parallel to the handle of the forceps.
The intervening shank connects the handle and blades of the forceps. The shank is longer in instruments such as the Kielland and Bailey-Williamson forceps, which are designed for midpelvic delivery. The shanks may be parallel (Simpson forceps) or may overlap (Elliott and Tucker-McLane forceps).
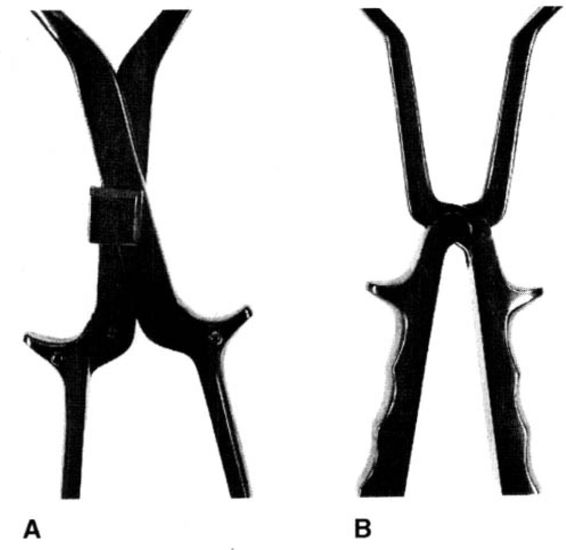
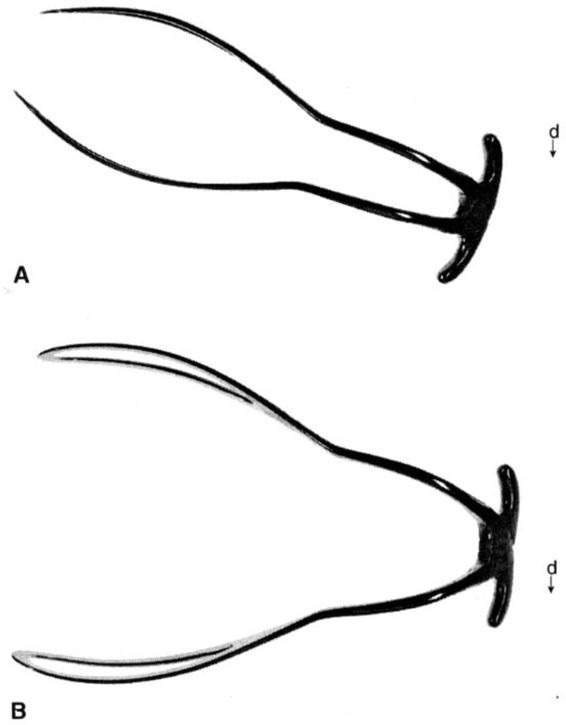
Each forceps has a locking mechanism located either on the shank or where the shank joins the handle. By convention, the lock is built into the left branch. The most commonly used locks are shown in Figure 6-9 and include the sliding lock (Kielland forceps) and the English lock (Simpson forceps). The English lock is a groove or slot lock at a fixed point for each member; articulation is rapid and easy. In comparison, the sliding lock of the Kielland forceps is built exclusively into the left branch and is not fixed when articulated. This lock is of the slot-type flanged design and is particularly useful where ideal application cannot at first be made because one unit must ride higher than its partner (Fig. 6-10), as often occurs with transverse arrest with asynclitism. The Laufe and short Piper forceps both use a pivot lock mechanism. The pivot lock is incorporated into the finger grip handles of the forceps and traction tends to cause the blades to diverge, minimizing compressive forces on the fetal head (see Fig. 6-11).
FIGURE 6-9. Shown is A. the sliding locking mechanism of the Kielland forceps and B. the fixed English lock of the Simpson forceps.
FIGURE 6-10. The Kielland forceps as viewed from above. This view could easily represent the forceps as applied to a right occiput transverse position with asynclitism. In this situation, the anterior blade is inserted higher into the pelvis than the posterior blade. The asynclitism is corrected by adjusting the shanks of the forceps after the sliding lock is engaged.
FIGURE 6-11. A. The Laufe divergent forceps are shown as viewed from above. They are characterized by parallel shanks and by a locking mechanism incorporated into the handle. B. When traction is placed upon the finger guards of the forceps, the blades tend to diverge, minimizing compressive forces on the fetal skull. When viewed in lateral projection, the forceps are notable for a pronounced reverse pelvic curve.
The final portion of the forceps is the handle. Finger grips or lateral flanges are incorporated into the majority of forceps in contemporary use.
The principle of axis-traction has been incorporated into the design of some instruments, such as the Hawks-Dennen forceps, and can be obtained with others by use of a traction bar (Fig. 6-2). The Bill axis-traction device can be attached to the handle flange of several forceps instruments. It assists the operator in applying traction in the proper plane by maintaining the vector force in an out and downward direction (Bill, 1925).
CONTEMPORARY INSTRUMENTS
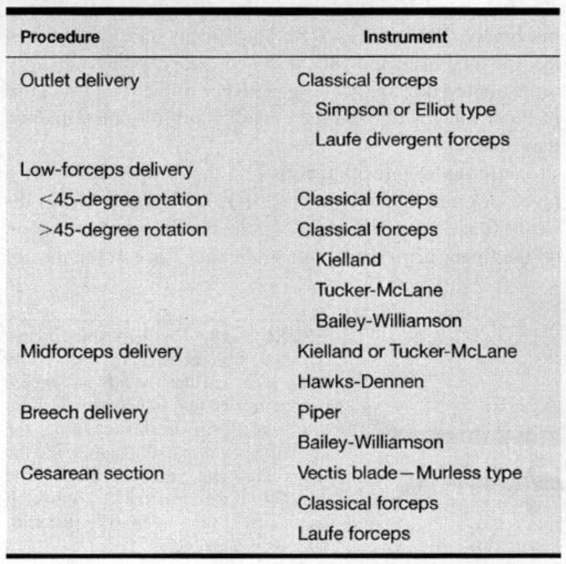
CLASSICAL INSTRUMENTS. The forceps selected depends upon the nature of the procedure and the clinical indications (Table 6-1). The Simpson and Elliot forceps are considered all-purpose or classical instruments. These forceps have English locks, which allow locking only at one point and only when the shank of the right branch overlies the left. The Simpson forceps have parallel shanks, fenestrated blades, and a long, tapered cephalic curve designed to fit the molded fetal head. Elliot forceps have overlapping shanks and short, fenestrated blades with a shorter and more rounded cephalic curve that is somewhat better suited for application to the unmolded head. A wheel-and-screw device is built into the handle of the instrument to avoid compression of the fetal head if the handles are squeezed (Fig. 6-12). The Tucker-McLane forceps, a variant of the Elliot type, have short, solid blades. The overlapping shanks and solid blades make this a popular instrument for rotations.
FIGURE 6-12. A close-up view of the handle of the Elliot forceps demonstrating the set screw between the handles, which is designed to reduce cephalic compression.
SPECIALIZED INSTRUMENTS. Specialized forceps have been developed to effect delivery in situations not amenable to solution with the classical instruments. The Kielland forceps, with no pelvic curve and a sliding lock (Fig. 6-4), originally were designed for use in midpelvic arrest, but they have been used extensively for rotations. The sliding lock is useful to correct asynclitism, a common problem in transverse arrest. Kielland forceps also are occasionally used to effect delivery of the face presentation.
Piper forceps have long shanks with a reverse pelvic curve for ease of application to the after-coming fetal head in a breech delivery (Fig. 6-8). The forceps stabilize and protect the fetal head and neck during delivery. When difficulty is encountered in spontaneous delivery of the fetal head, use of Piper forceps may produce lower morbidity than manual maneuvers.
Laufe-outlet forceps incorporate the unique design of a pivot lock and finger grips (Fig. 6-11). Divergent blades diminish the compressive force on the fetal head, and traction on the finger grips applies no additional force at the toes of the blades. The short length of the instrument makes it easy to apply at cesarean section. The Laufe forceps may also be useful for delivery of the after-coming head of the preterm breech fetus.
TABLE 6-1. Forceps Delivery—Instrument Type
Barton forceps, which consist of a hinged anterior blade, a posterior blade with an acute curvature, and a sliding lock, were developed for high-transverse arrest. Although not recommended by most obstetricians, there has been renewed interest in their use for delivery at cesarean section (Megison, 1993).
CLASSIFICATION OF FORCEPS OPERATIONS
A primary reason that forceps have remained controversial is the lack of agreement regarding classification of the operation. It is clear that different categories of forceps operations are associated with significantly different morbidity for mother and baby. The forceps operation has classically been described according to the station of the fetal bony head in the pelvis. There was disagreement as to whether the leading bony edge or the biparietal diameter (BPD) should determine station, as well as whether the pelvis should be divided by centimeters or by thirds.
TITUS CLASSIFICATION
In 1949, Titus, Greenhill, McCormick, and Eastman formulated a classification of forceps operations that they felt was simple, practicable with or without x-ray pelvimetry, and safe (Dennen, 1952). The major purpose of their system was to identify instances in which general practitioners could perform an instrumental delivery without consulting a specialist. Their system divided the pelvis from the spines to the inlet into “negative thirds” and from the spines to the outlet into “positive thirds.” This resulted in a narrow definition of low forceps, a broad definition of midforceps, and a well-accepted definition of high forceps.
DENNEN CLASSIFICATION
In 1952, Dennen proposed an alternative classification system based on the four major obstetric planes of the pelvis. He defined high forceps as the BPD in the plane of the inlet and the leading bony edge slightly above the ischial spines. The term “midforceps” described operations with the BPD through the inlet, the leading bony part at or just below the ischial spines, and with the hollow of the sacrum not yet filled. A low-midforceps delivery was one in which the BPD was in the plane of the spines, the leading bony point within a fingerbreadth of the perineum between contractions, and with the hollow of the sacrum filled. Outlet forceps referred to operations in which the BPD was below the plane of the spines and the sagittal suture was in the anteroposterior diameter, with the head visible during a contraction. The major points of contention with Dennen’s scheme were the confusing references to the plane of the BPD and the category of low-midforceps, which was later specifically disapproved in the 1965 classification scheme by the American College of Obstetricians and Gynecologists.
AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS-1965 CLASSIFICATION
In 1965, the American College of Obstetricians and Gynecologists (ACOG) adopted the Titus scheme for high, mid-, and outlet forceps operations. The term “outlet forceps” was used in preference to “low forceps,” but was defined equivalently. This classification was not well accepted, even at the time, because the definition of outlet forceps was too restrictive and resulted in the classification of many relatively simple operations as midforceps. The midforceps category included all instrumental deliveries commencing from the ischial spines down to the level of the pelvic floor as well as those in which rotation was required. Many clinicians felt that this distance in the pelvis (from the ischial spines to the perineum) was too great to be classified as a single operation.
AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS-1988 CLASSIFICATION
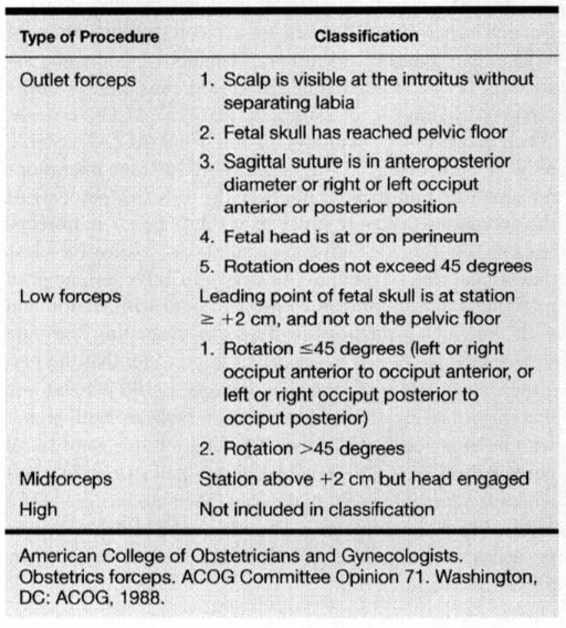
In 1988, ACOG issued a new classification that emphasized two factors. First, the station of the fetal head in the pelvis was estimated in centimeters. The pelvis from the spines to the outlet was divided into “negative 5 cm” and the lower pelvis from the spines to the outlet into “positive 5 cm.” Station referred to the level of the leading bony point of the fetal head at or below the level of the maternal ischial spines (Table 6-2). Engagement implied that the BPD had passed through the pelvic inlet, and that the leading bony edge of the fetal head was usually at the level of the ischial spines (0 station). The fetal head was classified as +5 cm when crowning. The category of high forceps was eliminated. Under virtually no circumstance were forceps to be applied to an unengaged presenting part, a fetus with intact membranes, or if the cervix had not dilated completely. The second important factor emphasized in the new classification was the degree of rotation, which was classified as ὄ45 degrees and >45 degrees.
TABLE 6-2. Classification of Forceps Deliveries According to Station and Rotation
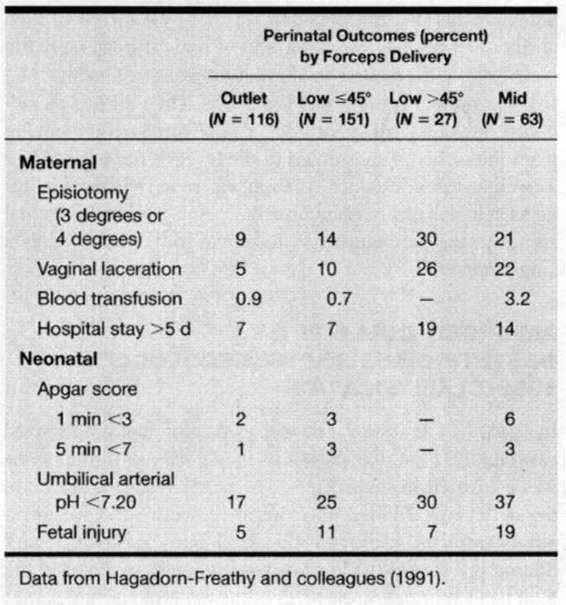
The 1988 classification was modeled closely after the Dennen scheme and has led to a clearer stratification of risks among types of operations. Hagadorn-Freathy and associates (1991) reported on 281 midforceps and 76 outlet forceps deliveries as classified by the 1965 ACOG criteria. When reclassified according to the 1988 ACOG criteria, only 22 percent of the original 281 midforceps operations remained as midforceps. Importantly, 178 (63 percent) of the operations that were previously classified as midforceps became low-forceps deliveries, and all but 27 involved less than 45 degrees of rotation. As shown in Table 6-3, adverse maternal and fetal outcome correlate both with station and with amount of rotation involved. In evaluating the data shown in Table 6-3, it is important to consider that the maternal injury rate with cesarean delivery is 100 percent and that maternal infection and transfusion rates are both higher with cesarean section. Further, the fetal injuries were facial nerve palsies (n = 10), brachial plexus palsy (n = 3), clavicular fracture (n = 5), and cephalohematoma (n = 24); most of these injuries resolved within days of delivery with no permanent sequelae, and all of the injuries resolved by 5 months of age.
TABLE 6-3. Maternal and Fetal Outcome by Forceps Operation
INDICATIONS
Indications for forceps delivery have changed little since early in the twentieth century. Forceps delivery may be indicated for maternal or fetal reasons, or both.
MATERNAL INDICATIONS
Maternal indications include disease states that impair the ability to push and conditions that may be worsened by prolonged voluntary expulsive effort. Examples of the former include neurologic disorders associated with weakness and certain pulmonary diseases; maternal cardiac disease is the classic example of the latter. Collectively, these diseases are uncommon. More often forceps delivery is indicated by maternal fatigue or by a dense regional block that inhibits motor fibers. The latter was common when saddle block anesthesia was used for vaginal delivery, but a properly dosed epidural block usually does not interfere with muscular control and expulsive efforts to the same degree.
FETAL INDICATIONS
Fetal indications include nonreassuring fetal heart-rate patterns. In the first stage, provided that the pattern cannot be resolved by intrauterine resuscitative measures, cesarean section is the only management option. In the second stage of labor, the obstetrician must carefully evaluate the clinical situation to determine whether abdominal or operative vaginal delivery will produce the best maternal and perinatal outcome. Forceps delivery may be more expedient than assembling an operative team for cesarean section. Conversely, a traumatic instrumental delivery from the midpelvic cavity may be avoided by judicious selection of cesarean delivery. These decisions require judgment, skill, and individualization on the part of the operator.
COMBINED MATERNAL AND FETAL INDICATIONS
Two other indications for forceps delivery are probably best classified as combined maternal and fetal indications. The first indication is termination of a prolonged second stage of labor. In the 1991 ACOG Technical Bulletin, prolonged second-stage labor is defined as lasting more than 3 hours in the nulliparous woman with a regional anesthetic, or more than 2 hours without a regional anesthetic. In a multiparous woman, a prolonged second stage is defined as exceeding 2 hours with, and 1 hour without, regional anesthesia. These recommendations are intended to serve as guidelines rather than as strict rules. The times can be exceeded safely if there is continued, albeit slow progress in descent without evidence of fetal or maternal compromise. Less often, arrest of descent may be diagnosed before these suggested time limits have been reached.
EPIDURAL ANALGESIA
Two important questions have been raised about the use of epidural analgesia: (a) Does it affect maternal expulsive efforts and duration of the second stage of labor? and (b) Does paralysis of the pelvic diaphragm result in fetal malposition? Hoult and colleagues (1977) prospectively studied the frequency of instrumental deliveries and the incidence of malposition in women with epidural analgesia. They found that nulliparous women were three times as likely to have malposition of the vertex and to require instrumental delivery. Institution of epidural blockade before cervical dilatation of 5 cm was not responsible for the increased incidence of operative vaginal delivery. However, when the anesthesia level was reduced and the woman’s sensation returned, the need for instrumental deliveries declined. The results of this study may have been influenced by the use of 0.5 percent bupivacaine in contrast to the 0.25 percent or 0.125 percent often used today. Still, Chestnut and colleagues (1987) found that 0.125 percent bupivacaine prolonged the second stage of labor and increased operative vaginal deliveries.
Philipsen and Jensen (1989) prospectively randomized women to regional analgesia or intravenous opiates in the first stage of labor. The epidural analgesic effect was allowed to wear off in the second stage, and women were not redosed after reaching 8 cm of dilation. With this protocol, the investigators found that there were an equal number of instrumental and spontaneous deliveries in each group. In contrast, when Thorp (1989) studied laboring women with epidural analgesia in whom the anesthesia had not been decreased or turned off, Thorp found that 25 percent had been delivered by forceps as compared with 7 percent of those women who had not had epidural analgesia. Kaminski and coworkers (1987), controlling for fetal size and malposition, reported a twofold increase in instrumental deliveries, as well as an incidence of midforceps deliveries that was three times greater in women with epidural analgesia. The incidence of malposition, such as persistent occiput posterior, was tripled.
Sharma and colleagues (1997) reported no increase in operative vaginal delivery in women receiving epidural analgesia during labor compared with patient-controlled intravenous narcotic. In a meta-analysis of epidural versus opioid analgesia, instrumental delivery was more likely if a woman received epidural analgesia (Halpern and colleagues, 1998). As discussed, many of these studies have involved intermittent bolus doses of local anesthetic agents administered in higher concentrations than currently used. The Practice Guidelines for Obstetrical Anesthesia of the American Society of Anesthesiologists Task Force on Obstetrical Anesthesia (1999) states that “the literature indicates a reduced incidence of spontaneous vaginal delivery associated with single-bolus epidural local anesthetics.” Proponents of epidural analgesia emphasize reports that low concentrations of anesthetic agents given by continuous infusion do not result in increased instrumental delivery (Wittels, 1991).
PREREQUISITES FOR FORCEPS APPLICATION
The decision to perform a forceps operation is at least as important as a decision to perform a cesarean operation. The following are the minimum prerequisites for an operative forceps delivery:
• The fetal head is engaged at 0 station or lower.
• The membranes are ruptured.
• The cervix is fully dilated and effaced.
• The exact position of the fetal head is known.
• The pelvis has been assessed for adequacy and the maternal-fetal size relationship evaluated.
• Appropriate maternal anesthesia is available.
• Necessary personnel and support equipment are available.
• The surgeon is knowledgeable about the instruments and technique and possesses the skills necessary to use them.
• There is a willingness to abandon attempts if the forceps delivery does not proceed readily.
• Informed consent has been obtained orally or preferably in written form.
Far more critical than technical proficiency is the knowledge of when forceps should be used and when they should not.
ANESTHESIA REQUIREMENTS FOR FORCEPS DELIVERY
Adequate levels of anesthesia are important to ensure the safest delivery for both mother and the fetus. Generally, pudendal block analgesia is sufficient for outlet forceps and for low forceps operations involving rotation ≤45 degrees. For low-forceps operations with rotation >45 degrees and for midforceps operations, regional analgesia is preferred. General anesthetic agents also may be used for forceps deliveries.
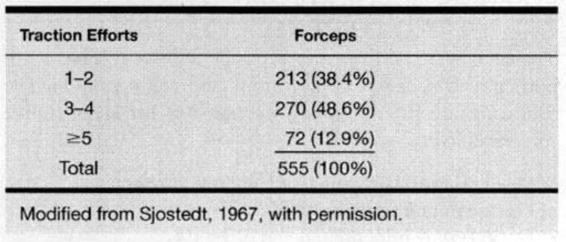
TRAINING
An important prerequisite for the conduct of a forceps delivery is a skilled operator. The physician must be able to adequately assess the capacity of the bony pelvis and any soft-tissue obstruction; determine that the cervix is fully dilated and that the fetal vertex is engaged; and must know unequivocally the fetal position and station. Also important is the physician’s ability to determine flexion, asynclitism, caput, and molding. The forceps must be properly applied to the fetal head (cephalic placement) because incorrect application increases the risk of injury. Finally, the operator must properly apply traction by using the minimum amount of force in the direction of least resistance. Station should be gained with each application of traction. An earlier study (Table 6-4) reported that the majority of deliveries usually required five or fewer “pulls” (Sjostedt, 1967).
TABLE 6-4. Number of Traction Efforts Required to Achieve Vaginal Delivery
A survey of 144 United States and Canadian residency programs was conducted in the early 1980s to determine existing attitudes on the use of forceps (Healy and Laufe, 1985). Of the 73 percent of programs that responded, all still used outlet forceps. Furthermore, all but one program reported that they still performed midforceps procedures. In 1990, Ramin and colleagues repeated this survey to assess the impact of the 1988 classification system on practice patterns. Ninety-nine percent of responding residency programs stated they were aware of the new definitions and 80 percent were using them. Although all programs continued to use outlet forceps, 14 percent no longer performed midforceps deliveries. The trend was toward fewer operative vaginal deliveries and increased reliance on cesarean section. In half of all programs, less than 5 percent of all deliveries were performed by outlet or low forceps. The decline in midforceps use probably reflects the more stringent new definitions; less than 1 percent of all deliveries are by midforceps in 75 percent of training programs; the rate is probably lower in private practice (Ramin and associates, 1993).
The decrease in the actual number of forceps deliveries in part reflects the attitude of the residency program directors. In 1990, 75 percent of the directors believed that outlet forceps operations were “important” or “extremely important” and 40 percent believed midforceps were “important” or “very important”; 20 percent of the directors thought midforceps training was of no importance. In the more recent survey by Hankins and colleagues (1999), 47 percent of the fellowship directors and 38 percent of residency program directors expected proficiency in midforceps delivery. All expected proficiency with outlet forceps delivery! Training should occur at the podium and in the delivery room. Experienced operators should supervise application of forceps by trainees.
FETOPELVIC RELATIONSHIP
An important prerequisite for forceps deliveries is an accurate assessment of fetopelvic relationships. An essential component of training for instrumental vaginal deliveries is clinical evaluation of the pelvis.
THE FETUS. The exact position of the fetal head can be diagnosed by vaginal examination. It is, however, not always simple. Caput and molding, redundant maternal soft tissue, and reliance on palpation of the fontanelles may contribute to incorrect diagnosis.
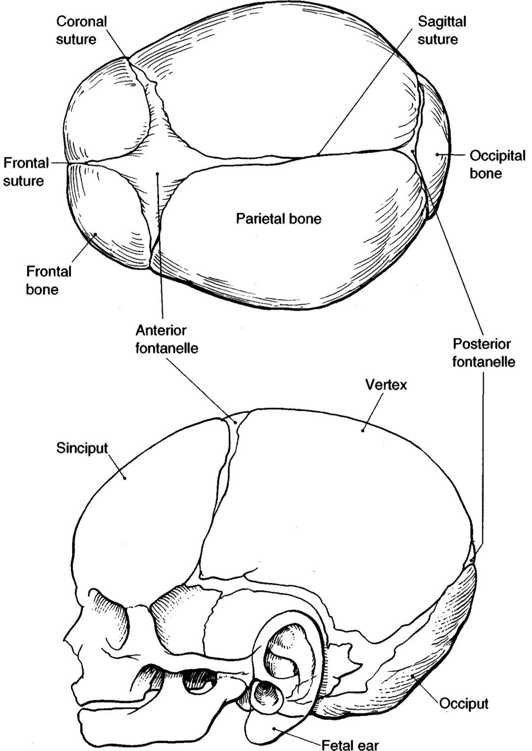
Using a systematic approach, the examiner should first attempt to locate the sagittal suture (Fig. 6-13). This suture should be traced in both directions, the shape of each fontanelle assessed, and the number of lines of intersection counted. At the posterior fontanelle, the two lambdoid sutures and the sagittal suture account for three intersecting lines. At the anterior fontanelle, the right and left halves of the coronal suture intersect with the frontal (metopic) suture and the sagittal suture, producing a total of four intersecting lines (Fig. 6-13). Sometimes the shape of the fontanelle (the posterior is triangular, the anterior is diamond shaped) will suffice for diagnosis; but meticulous counting of sutures is preferable. If diagnosis of position remains in doubt, the examiner should locate a fetal ear. The posterior ear is usually more readily accessible, and both the external auditory meatus and the pinna should be sought. Knowing the relative position of these two structures should lead to a correct assessment of position.
FIGURE 6-13. The landmarks of the fetal skull necessary for determining fetal position.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree