Fluids and Electrolytes
Paritosh Prasad
Avram Z. Traum
Body and Parenteral Fluids
Composition of Basic Fluids and Replacement Solutions
| [Na] | [Cl] | [K] | [HCO3] | pH | |
|---|---|---|---|---|---|
| Gastric | 70 mEq/L | 120 mEq/L | 5–15 mEq/L | 0 mEq/L | Acidic |
| Pancreatic | 140 mEq/L | 50–100 mEq/L | 5 mEq/L | 100 mEq/L | Basic |
| Bile | 130 mEq/L | 100 mEq/L | 5 mEq/L | 40 mEq/L | Acidic |
| Diarrhea | 50 mEq/L | 40 mEq/L | 35 mEq/L | 50 mEq/L | Variable |
| Ileostomy | 130 mEq/L | 120 mEq/L | 15–20 mEq/L | 25–30 mEq/L | Basic |
| NS (0.9%) | 154 mEq/L | 154 mEq/L | 0 mEq/L | 0 mEq/L | 5.5 |
| ½ NS (0.45%) | 77 mEq/L | 77 mEq/L | 0 mEq/L | 0 mEq/L | 5.5 |
| ¼ NS (0.23%) | 38 mEq/L | 38 mEq/L | 0 mEq/L | 0 mEq/L | 5.5 |
| Ringer Lactate | 130 mEq/L | 109 mEq/L | 4 mEq/L | 28 mEq/L | 6.5 |
Calculation of Maintenance Fluids and Electrolyte Needs
(Pediatr Rev 2001;22:380)
Basal state maintenance fluid needs determined by basal metabolic rate; amt of fluid needed to dissipate heat via respiratory tract and skin.
Multiple methods; BSA method, basal calorie method, and Holliday-Segar system. Only last (Holliday-Segar) does not require a table of values.
Holliday-Segar formula equates kcal with mL (1:1) of fluid needed for dissipation
Electrolyte maintenance needs (not for neonates): Na 2–4 mEq/kg/d, K 1–3 mEq/kg/d, Ca 2–3 mEq/kg/d, Phos 0.5–1.5 mEq/kg/d, Mg 0.1–1 mEq/kg/d.
D5 1/2 NS usually used for maintenance w/ 20 mEq/L KCl added once pt has urinated; for pts <1 yo consider D5 1/4 NS (now controversial; does not apply to neonate) (see NICU section). (Arch Dis Child 2008;93:335)
Dehydration and Rehydration
Definition
(Pediatr Rev 1996;11:395; JAMA 2004;291:2746)
Fluid deficit 2/2 imbalance btw fluid losses (nml or ↑) and fluid intake (nml or ↓).
Dehydration is a leading cause of morbidity & mortality in kids, esp in 3rd world
Though often used interchangeably, strictly, dehydration ≠ hypovolemia
History and Exam
(JAMA 2004;291:2746)
Hx fever (insensible losses), ↓ oral intake, types of intake (H2O alone predisposes to HoNa), freq of urination (↑ UOP w/ dehydration → diabetes insipidus), diarrhea (frequency), other sites or sources of loss (ostomies, biliary tubes, etc.).
Assessment of weight loss via H&P as above or from actual documented weights.
Weight loss (kg) = fluid deficit (L); based on radio-labeled albumin experiments
Inaccurate in setting of “3rd spaced fluids” (nephrotic syndrome, CHF, cirrhosis) where patient is intravascularly deplete but weight is up.
Capillary refill; compress and release superficial cap bed (palmar finger-tip w/ arm heart level), varies as fxn of temperature, site, lighting, meds, & autonomic Δ.
Skin turgor; skin pinch at lateral abd wall at umbilical level. Less accurate w/ hyperNa (false nml) and w/ malnutrition (falsely prolonged). Complicated in 1° skin dz.
Can assess dehydration clinically based on history, exam, & assessment of weight loss.
Dehydration
Mild
Moderate
Severe
Sens/Spec*
Weight loss – infant
5%
10%
>15%
————
Weight loss – child
3%–5%
6%–9%
>10%
————
HR/BP
Nml
Nml-Tachycardic and orthostatic
Tachycardiac and orthostatic-shock
0.52/0.58 (for inc HR)
RR
Nml
Nml-increased
Hyperpnea (deep rapid breathing)
0.43/0.79
Anterior fontanelle
Nml
Sunken
Very sunken
0.49/0.54
Mucous membranes
Nml
Dry
Cracked
0.86/0.44
Tears
Nml
Decreased
Dry, sunken eyes
0.63/0.68
Skin (less accurate if HyperNa or <2 yo)
Cap refill (CR) <2 sec
Cap refill 2–4 sec, dec skin turgor (ST)
Cap refill <4 sec and skin tenting, cool and mottled
CR 0.60/0.85 ST 0.58/0.76
Urine output and SG
>1.020
>1.020 +/- oliguria
Oliguria to anuria
Behavior
Nml
Irritable
Lethargic/obtunded
0.80/0.45
Total fluid deficit
30–50 cc/kg
60–100 cc/kg
>100–150 cc/kg
*tested for assessment of 5% dehydration
Most sens for dehydration are dry mucous memb & irritability/lethargy
Most spec; poor cap refill, poor skin turgor, hyperpnea (rapid deep breaths w/o evidence resp distress)
Diagnostic Studies
(Pediatrics 2004;114:1227)
Chem7, U/A w/ spec grav, serum pH, calculate anion gap, serum Osm. Urine Osm and urine electrolytes can help clarify complex situations.
One study showed HCO3 ≤13 mmol/L predicted admission in pts 6 mo–13 yo p/w acute gastroenteritis and dehydr receiving IVFs. (Ann Emerg Med 1996;28:318)
Another study looked at lytes in pts 2 mo–9 yo w/ acute gastro & dehydr; Only 1/10 had abn labs effecting care. Bicarb did not effect need for admit.
Pts <1 yo had lower HCO3 than older pts w/equiv dehyd (Pediatrics 2004;114:1227)
Review of lab abn and their sens and spec for dehydr in meta-analysis of studies of pts aged 1–5 yo p/w dehydration. Adapted from JAMA 2004;291:2746
Lab parameters
Sensitivity
Specificity
BUN/Cr >40
0.23
0.89
Bicarb <17 mEq/L
0.83
0.76
Bicarb <15 mEq/L
0.93
0.40
pH <7.35
0.43
0.80
Anion gap >20 mmol/L
0.46
0.74
If additional sensible losses (ostomy, biliary drain, etc.) check fluid lytes to guide repletion; also Ulytes and UOsm
Gastric losses: Can generally replace 1:1 w/ 1/2 NS + 10 mEq/L KCl
Diarrhea/biliary/ostomy output: Can generally be replaced 1:1 w/ LR
Management
(Arch Dis Child 2007;92:546; Pediatr Rev 2001;22:380)
Correct hemodynamic compromise with 20cc/kg boluses of NS until improved.
Assess fluid loss by weight Δ or H&P as above and subtract boluses for remaining fluid deficit
Remaining fluid deficit given in 1 of 2 ways (applies if no severe [Na] abn noted, if significant hypo/hyper Na present see specific management) given as D5 1/2 NS; add 20 mEq KCl once UOP established
Make sure to account for ongoing losses as well q2–4h.
Classic approach:
Remaining deficit = Total volume deficit (% weight loss) – initial boluses
Provide ½ of remaining deficit over first 8 hr + hourly maintenance rate
If 5 kg pt w/ 10% wt loss, deficit = 500 cc, if given 20 cc/kg bolus, remaining deficit is 400 cc. Give 200 cc over 8 hr (25 cc/hr) + maintenance (4 cc/kg * 5 kg = 20 cc/hr); so 45 cc/hr for first 8 hr
Provide other ½ of remaining deficit over next 16 hr + hourly maintenance.
For pt above, give remaining 200 cc over next 16 hr (12.5 cc/hr) + maintenance (20 cc/hr); so 32.5 cc/hr (round to 33 cc/hr) for next 16 hr.
Short hand approach:
Remaining deficit calc as above, and all given over 1st 8 hr w/o maintenance
For same pt above, give all 400 cc over 8 hr (50 cc/hr) and no added fluid for maintenance; so 50 cc/hr for first 8 hr
Then give total 24-hr maintenance over remaining 16 hr (accounts for that not included for 1st 8 hr); equivalent to 1.5× maintenance for 16 hr.
So for same pt above, give 1.5× maintenance for next 16 hr (maintenance 20 cc/hr; 1.5 maintenance is 30 cc/hr); so 30 cc/hr for 16 hr.
First-line therapy for mild to moderate dehydration remains use of oral rehydration.
Pretreat nausea then start w/ 5–10 cc q5min w/ goal 50–100 cc/kg in 1st 4–8 hr.
Aggressive ORT (100 cc/kg in 8 hr) shown to result in prompt resolution of [Na] abn; 90% did not require IVFs, and though solutions are hypoNa they did not result in HoNa. (Am J Clin Nutr 1980;33:637)
ORT composition
Glucose
Na
Cl
HCO3
K
Pedialyte
140 mmol/L
45 mEq/L
35 mEq/L
30 mEq/L
20 mEq/L
WHO-ORS
110 mmol/L
90 mEq/L
80 mEq/L
30 mEq/L
20 mEq/L
RCT comparing IVF to ORT for mod dehydr demonstrated noninferiority of ORT at 4 hr w/ shorter time to initiation w/ ORT and <1/3 of ORT pts required hospitalization vs. ½ of IVF treated pts. (Pediatrics 2005;115:295)
Still ORT is used <30% of the time that it is indicated in the United States.
Hyponatremia
Definition
(Pediatr Rev 2007;28:426)
Serum sodium <135 mEq/L; most common electrolyte abnormality in pediatrics
Pseudohyponatremia is lab abnormality 2/2 ↑ serum lipid or protein (nml Posm) if gas chromatography used to assess [Na]; diff than true dilutional hyponatremia 2/2 osmotic shifts (inc Posm) 2/2 hyperglycemia, IVIG, mannitol, etc.
Pathophysiology
(Rose & Post. Clinical Physiology of Acid-Base & Electrolyte Disorders 2001. p 696)
Water follows Na; fluid losses (diarrhea, vomiting) often isosmotic to plasma; HoNa results when lost volume is replaced w/ water.
Nml response to ↓ volume is antidiuretic hormone (ADH) secretion; upregulates aquaporin channel insertion into collecting tubules (CT) → ↑ H2O reabsorption, ↑ circulating volume and production of concentrated urine.
Once euvolemia is restored, ADH secretion suppressed resulting in decreased urine concentration, increased urinary H2O excretion, and normalization of [Na]
For HoNa to be sustained, need continued inapprop intake/admin of hyposmotic fluid, inhib of NaCl reabsorp 2/2 diuretics (or channelopathies), cont ↓ circ volume, inapprop ADH secretion or inapprop H2O permeability of CTs (2/2 hypothyroid or AI), or renal failure.
W/ HoNa, relative H2O excess in serum (↓ serum osm) → cell swelling (esp brain edema).
If rapid, ↑ risk herniation or apnea; if subacute or chronic, brain cells respond by upregulation/synthesis of cell products, mitigating fluid shifts
2/2 cell response, correction of acute HoNa can be done acutely, whereas correction of subacute/chronic HoNa should be slow.
Clinical Manifestations
(Pediatr Rev 2002;23:371)
Symptoms 2/2 HoNa all neurologic dysfunction 2/2 brain cell swelling
Hx of volume loss (source), fluid repletion (type of fluid used, how formula made, esp w/ powdered formulas), meds (diuretics, IVIG, mannitol), underlying illness (DM, hypothyroid, adrenal insufficiency, renal channelopathy).
Attempt to define chronicity if possible
Symptoms 2/2 HoNa usually only present at levels <120 mEq/L, and can be asymptomatic (or w/ subtle cognitive defects) at this level if achieved slowly.
Can be nonspecific; malaise/lethargy, N/V, HA, confusion/agitation, muscle cramps, szr (2/2 pressure against rigid skull), ↓ reflexes, muscle weakness, hypothermia, irregular resp (2/2 impending herniation), coma, and even death.
Primary goal of clinical exam is assessment of volume status
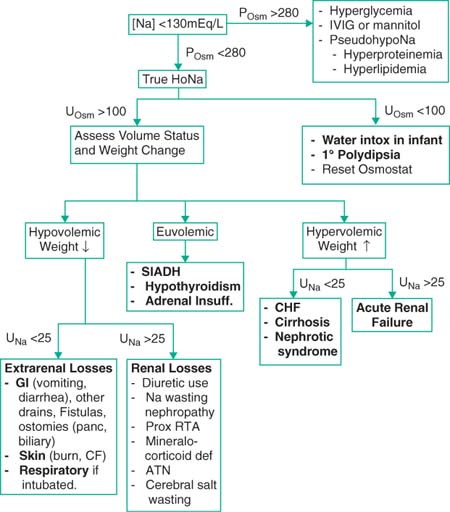
Etiologies and Diagnostic Studies
(Pediatr Rev 2007;28:426; Pediatr Rev 2002;23:371)
Electrolytes, serum Osm, UOsm, UNa, can check lipids and protein? pseudohypoNa
If hyperglycemia, hyperlipidemia, or hyperproteinemia, can correct [Na]
Hyperglycemia: Correct up [Na] 2.4 mEq/L for each 100 mg/dL glucose above 200
Hyperproteinemia: Correct up [Na] 0.25× [protein (g/dL) – 8]; only if Tot Prot >8
Hyperlipidemia: Correct up [Na] 0.002× [triglyceride(mg/dL)]
1° Polydipsia and water intoxication: 2/2 excess water intake either 2/2 psychiatric condition w/ excess H2O consumption, or in populations unable to control intake (infants), admin of excess H2O. Rx’d w/ free water restriction.
SIADH: Release of ADH not stim by hypovolemia or hyperosmolality (pt cannot be hypovolemic for this dx), resulting in inapprop enhanced water reabsorption but minimal edema formation (kidney responds by inc Na secretion)
Multiple\etiologies
Neuro: Meningitis/encephalitis, SAH/subdural/epidural, neoplasm, pituitary surgery, psychosis, HIV, Guillain-Barré
Drugs: Cyclophosphamide, vincristine, vinblastine, SSRIs, Haldol
Pulmonary: PNA, TB, asthma, pneumothorax
Severe nausea or pain
Ectopic ADH 2/2 small-cell lung CA (highly unlikely in pediatric patient)
Management of SIADH is with free water restriction (if needed, can use ½ maintenance or just restrict to replacement of insensible losses (40 cc/kg/d))
 |
Management
(Rose & Post. Clinical Physiology of Acid-Base & Electrolyte Disorders 2001.p696)
Correction of HoNa is driven by patient’s symptomatology and chronicity of HoNa
If hemodyn compromise 2/2 vol depletion, rx w/ IV NS 20 cc/kg boluses until stable.
If pt seizing, significant ΔMS, impending resp arrest, correct [Na] rapidly, otherwise rx slowly if unclear chronicity. (symptoms 2/2 HoNa rare unless [Na] <120)
Hypovolemic HoNa: Correct HoNa by providing sodium, don’t need to normalize [Na] and don’t correct >12mEq/24 hr
Total Na def = (% body H2O × lean body weight(kg)) × (goal Na – measured Na)
% body water as above; generally can use 60% (0.6) in pediatric patient
So for 25 kg pt w/ Na 110; total Na deficit = (0.6 × 25) × (120 – 110) = 150 mEqNa
Choose Na solution for repletion and do not replace at >12 mEq/24 hr
If asymptomatic, replace 0.5 mEq/hr over first 24 hr
If severe neuro sx, can replace at 1.5–2 mEq/hr for first 3–4 hr or till sx Resolve, but still try not to correct >12 mEq over the first 24-hr total.
3% NaCl has 513 mEq/L; 0.9% NaCl (NS) has 154 mEq/L
So for above pt could give ∼1L NS over 24 hr (∼40 cc/hr), or 292 cc of 3% NaCl over 24 hr (∼12 cc/hr) for a rough correction of 0.4 mEq/L/hr, may round down to avoid over correction.
Make sure to account for insensible losses and maintenance as well
Rough correction of severe HoNa is w/ 0.5 cc/kg/hr 3%NaCl to achieve raise in Na of 12 mEq in 24 hr. 1.0 cc/kg/hr to achieve in 12 hr.
Correction is never perfect, so serum [Na] should be followed q2–4h.
Hypervolemic HoNa: Generally Rx’d w/ Na and free H2O restriction, unless severe neurologic sx. due to HoNa in which case replace Na as above.
Can also use diuresis (CHF and cirrhosis), or if anuric in renal failure then dialysis
Complications
(Pediatr Rev 2002;23:371)
Untreated severe HoNa can result in severe neuro dysfxn, szr’s, herniation, coma, and death as previously discussed; in presence of significant neuro sx, must treat aggressively.
Overrapid HoNa correction (>∼12 mEq/24 hr) can result in central demyelinating lesion (particular at pons; central pontine myelinosis) presents one to several days after correction w/ paraparesis/quadriparesis, dysarthria, dysphagia, coma, or szr. Confirmed by CT or MRI; can take 4 wk + before radiologically detectable.
Hypernatremia
Definition
(Pediatr Rev 2002;23:371)
Sodium concentration >145 mEq/L; seen in hospitalized pts w/o access to free water or receiving hypernatremic IVFs, can also be seen in infants unable to obtain free water.
Pathophysiology
(Rose & Post. Clinical Physiology of Acid-Base & Electrolyte Disorders 2001.p746)
Hypernatremia is 2/2 either inappropriate water loss (>Na loss) or Na retention
Free water loss can occur from skin and respiratory tract or w/ dilute urine (diuretics or osmotic diuretic agents [glucose, mannitol]), diarrhea is variable in composition but can see excess water loss w/ osmotic or malabsorptive diarrhea.
Body attempts to correct HyperNa w/ inc ADH release → concentrated urine (occurs at POsm >280 mOsm/L) and by driving thirst (rare for pt to be hypernatremic w/ access to H2O)
Hypernatremia (w/ resultant hyperosmolality) → cellular dehydration, particularly at brain resulting in the symptoms assoc w/ HyperNa.
Acutely can be severe enough to cause subdural bleed or SAH. (Pediatr Rev 1996;17:395)
Subacute or chronic HyperNa allows brain cells to adapt by production of intracellular osmoles to balance gradient (w/i 1 hr); overrapid correction → cerebral edema.
Hypernatremia w/ [Na] >160 mEq/L has mortality of 10%–15%.
Epidemiology
(Pediatr Rev 2002;23:371)
High risk include debilitated pts w/ acute or chronic illness, infants, and particularly preterm (small mass: BSA ratio) and reliance on caretakers for fluids (ineffective breast-feeding).
Clinical Manifestations
(Pediatr Rev 2002;23:371)
Assess patient’s access to free H2O, hx of polyuria (DI, DM, nephropathy), absence of thirst (in setting of hyperNa and inc POsm, this reflects hypothalamic lesion)
Patients are generally irritable but can progress to lethargy, seizures, coma, or death
Neurologic exam may reveal increased tone, brisk reflexes, or nuchal rigidity.
HyperNa can result in “doughy” skin texture; falsely normalizes skin turgor
Etiologies and Diagnostic Studies
Check basic electrolyte panel, U/A, serum Osm, urine Osm, urine sodium.
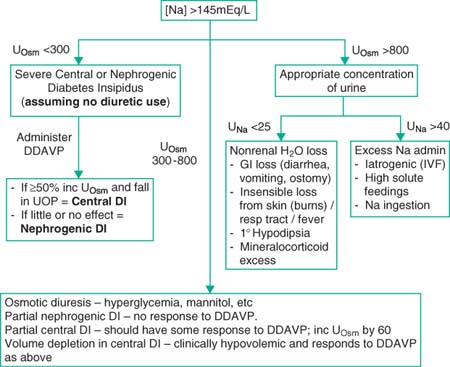
Diabetes Insipidus (DI): Complete or partial failure in secretion of (central) or response to (nephrogenic) ADH
Renal water absorption decreases, resulting in elimination of dilute urine
P/w symptoms of polyuria and polydipsia before developing sx of HyperNa
Central DI (responds to exogenous ADH); can be idiopathic, 2/2 neurosurgery (transsphenoidal surg), neoplastic (craniopharyngioma), 2/2 hypoxic/ischemic encephalopathy (Sheehan syndrome, s/p arrest), or other (Neurosarcoid, anorexia nervosa, histiocytosis X)
Nephrogenic DI (no/minimal resp to ADH); congenital, ifosfamide (chemo), other drugs (Li, demeclocycline), sickle cell, pregnancy, 2/2 hyperCa or hypoK.
Management
(Pediatr Rev 1996;17:395)
Rapid correction of HyperNa can result in cerebral edema, seizures, permanent CNS sequelae, or death; unless pt is significantly symptomatic, correct slowly.
If pt hemodyn unstable 2/2 hypovolemia, rx w/ IV NS 20 cc/kg boluses until stable
Maximum safe rate for lowering [Na] is 0.5 mEq/L/hr over 24 hr or 12 mEq/L/d
If significant sx from HyperNa (seizing), lower sodium more rapidly until sx resolve (1.5–2 mEq/L/hr for 3–4 hr), then try not to lower >12 mEq/L/d over all.
Calculation of water deficit as follows:
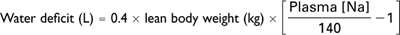
Total body water calculated as 0.4 (40%) of lean body weight (instead of usual 60%) as assumes pt somewhat dehydrated (water deplete)
So for 25 kg pt w/ [Na] 160; water deficit is (0.4 × 25) × ((160/140)- 1) = 1.4 L H2O
Assume correct 10 mEq/d; so needs to correct over 2 d; approx 30 cc/hr H2O
Seizure may occur during correction (may reflect cerebral edema); if occurs, rate of correction should be slowed or administer hypertonic saline. Usually self-limited and not reflective of long-term sequelae. (Pediatr Rev 2002;23:371)
Make sure to account for insensible losses and maintenance as well.
A rough rule of thumb is that 4 cc/kg of free H2O will dec [Na] by 1 mEq/L
Water deficit is the amount of positive water balance needed to correct sodium to 140
Provide such that correction is <0.5 mEq/L/hr; ideal w/ change [Na] <10–12 mEq/d.
If patient has central DI, cannot correct [Na] w/o administration of DDAVP
If nephro DI, mgmt involves use of thiazide diuretic and low Na and low-protein diet.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


