Fever of Unknown Origin
Russell W. Steele
The definition of FUO requires an immunologically normal host with oral or rectal temperature ≥38.0°C (100.4°F) at least twice a week for more than 3 weeks, a noncontributory history and physical examination, and 1 week of outpatient investigation.6-9 Early diagnostic studies normally include a complete blood cell count; lactate dehydrogenase (LDH); uric acid; urinalysis and culture; chest roentgenogram; tuberculin skin test; erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP); and, in the older child, a titer of antinuclear antibodies. Management of patients with comorbidity factors such as acquired or congenital immunodeficiency, neutropenia, and occurrence of fever during prolonged hospital stays is not considered in the following discussion.
The greatest clinical concern in evaluating FUO is identifying patients whose fever has a serious or life-threatening etiology for whom a delay in diagnosis could jeopardize successful intervention. Cancer and severe bacterial infections are the causes most frequently discussed and most likely to influence diagnostic and management approaches. However, the vast majority of children with prolonged FUO resolve their illnesses without a diagnosis and do not exhibit long-lasting effects. Therefore, it appears appropriate for most children to delay extensive diagnostic evaluation until the child has remained febrile for at least 6 weeks.
Because of the ready availability of more sensitive serologic assays and more precise radiographic scanning procedures, the etiologies of FUO in children, as well as in adults, have changed over the past three decades (Table 228-1). The most striking change has been the virtual elimination of laparotomy as a final step in evaluation, a procedure routinely recommended in the 1970s, but now eliminated due to advances in radiologic imaging technology.
Three newly defined infectious diseases now account for a moderate number of cases: Epstein-Barr virus infection, cat-scratch disease, and Lyme disease. All three can be confirmed with serologic assays showing both IgM and, later, IgG antibodies to the respective pathogens. Cat-scratch disease can also be confirmed with compatible liver lesions documented by abdominal sonograms or CT scans.
Two-thirds of children who now present with fever of unknown origin resolve their fever without determination of a cause, in contrast to only 10% to 20% in a series published 20 to 30 years ago.7-12 In addition, a higher percentage of children with malignancies is now definitively diagnosed earlier in the course of illness, and such cases lead to an overall reduction in total cases of fever of unknown origin. A greater percentage of the remainder likely have viral illnesses that are more difficult to diagnose but more likely to resolve without intervention.
Table 228-1. Etiology of Fever of Unknown Origin in Children
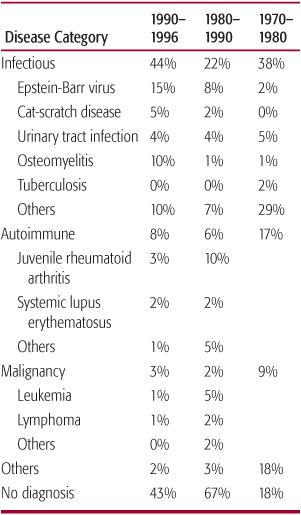
Infectious diseases now account for approximately 40% of identified etiologies with the most common being Epstein-Barr virus infection,7 cat-scratch disease,11 and urinary tract infection.12 All three can be confirmed with simple laboratory studies.
CLINICAL EVALUATION
An oral or rectal temperature ≥38°C (100.4°F) is two standard deviations above the average for normal children and most appropriately defines fever. Rectal recordings are preferred for younger children. Tympanic temperatures are so unreliable that they cannot be used to monitor febrile patients. Many parents believe that any temperature above the average—that is, 37°C (98.6°F)—is abnormal and seek consultation for these observations. Unless there are other clinical findings, either historically or during physical examination, reassurance is the only intervention warranted for temperatures <38°C (100.4°F).
For “subjective” fevers, usually meaning that the child feels warm to the parent or another caregiver, a diary recording of morning and afternoon rectal temperature measurements for at least 1 week should be obtained before initiating diagnostic evaluation. Children often feel warm, particularly when environmental temperatures are high enough to induce flushing or perspiration. Despite widespread public perceptions, few parents (or grandparents) can determine low-grade temperature elevations by simply touching their children’s forehead. However, core temperatures >39.4°C (103°F) consistently produce skin temperature changes that can be recognized by most caregivers.
The number of documented febrile recordings during a 21-day observation period considered abnormal is arbitrarily suggested as two per week. However, cases should be individualized. Well-defined events such as otitis media or limited viral illnesses can account for some febrile periods. Conversely, antipyretic therapy might mask significant temperature spikes. In cases of factitious fever (Munchausen syndrome by proxy), potential underlying family psychopathology should be assessed and managed with appropriate professional evaluation and counseling.
Common viral or bacterial pathogens that present atypically are much more frequent than exotic or unusual diseases. Therefore, epidemio-logic information and history of exposure prior to illness are major components of the initial evaluation. Diagnoses quite common in one area of the United States might not even be considered in other locations. Examples include Lyme disease (Northeast and certain areas of the Midwest), tularemia (Midwest and far West), coccidioidomycosis (Southwest), and tuberculosis (urban).
Age is the next critical factor. Leukemia peaks in early childhood, whereas lymphomas are unusual before age 8 years. HIV infection presenting as fever of unknown origin is more prevalent during the first year of life or after adolescence. Most autoimmune disease is seen in school-age children and adolescents, so screening tests for this category would usually be limited to this older age group.
Patient history should be more detailed than that obtained for acute illnesses, carefully examining family history, previous illnesses, recent symptoms, current medications, travel, and exposure to pets or humans with potential communicable pathogens. Weight loss, failure to thrive, or decreased activity during afebrile periods are more ominous systemic signs that will usually require a more rapid diagnostic evaluation. Prolonged fever and bone pain may be the only manifestations of bone tumors, leukemia, osteomyelitis, syphilis, cat-scratch disease, tuberculosis, or Langerhans cell histiocytosis. In the presence of documented fever and constitutional symptoms, a history of abdominal pain necessitates evaluation for autoimmune diseases, pyelonephritis, Crohn disease, and hepatitis, as well as abdominal abscesses and tumors.
Of all symptoms, the presence of pain is the single finding that is likely to suggest specific laboratory studies. Therefore, pain should be completely characterized by its severity, location, periodicity, precipitating factors, and response to attempted therapy.
Physical examination occasionally provides the first diagnostic clue, especially when directed toward areas where abscesses or solid tumors are less apparent. Thorough abdominal and rectal exams are essential because the abdomen and pelvis represent the largest area for such masses. Bones and joints can be adequately evaluated if the child is cooperative. Transillumination of sinuses is only useful in the older child and adolescent; younger children require selective CT scans to diagnose sinusitis.
Table 228-2. Initial Evaluation and Rationale for Screen



