Fetal Imaging: Ultrasound and Magnetic Resonance Imaging
Dorothy I. Bulas
Advances in high-resolution sonographic imaging and rapid sequencing magnetic resonance imaging (MRI) have provided exquisite detail regarding the fetus and intrauterine environment. The ability to assess the health of the fetus and identify anomalies has changed the practice of both obstetrics and neonatology. By identifying the fetus with anomalies or at risk for intrauterine compromise, management can be guided by appropriate specialists with resultant improved outcome.
ASSESSMENT OF FETAL AGE, GROWTH, AND MATURITY
Accurate assessment of fetal age is crucial for perinatal management. Overestimating the age of a fetus can result in the delivery of a premature infant, whereas underestimating the age of a growth-retarded fetus can result in a fetal death.
Fetal age can be determined based on obstetric history and clinical data, but estimations can be inaccurate in up to 40% of patients (1). The use of ultrasound provides a method of significantly improving the accuracy of gestational age determination. Measurements used to assess age have been chosen on the basis of their relationship with gestational age and ease in obtaining these measurements and reproducibility. The fetal biparietal diameter (BPD) measurement was the first measurement used because the cranium was the most easily visualized body part (2). There are many tables and nomograms that describe the normal growth of various fetal organs. Most predictions of gestational age are based on the 50th percentile measurement with a wide range of normal values. At the various gestational ages, each fetal dimension differs in how easily and reliably it can be measured. Thus, a combination of measurements is superior to a single measurement, with computer software that permits instantaneous calculation of fetal age and weight estimates and plotting growth curves. Functional studies of the fetus, such as breathing patterns, can also aid in the determination of gestational age.
DETERMINING FETAL AGE
First-Trimester Assessment
In the first trimester, fetal imaging using a transabdominal approach is often difficult because the uterus is low within the maternal pelvis and may be obscured by overlying gas. Transvaginal ultrasound transducers greatly improve fetal visualization in early pregnancy. The probe is placed into the maternal vagina in close proximity to the uterus and fetus. High-resolution fetal images can thus be obtained for accurate assessment of fetal morphology. By use of transvaginal scanning, a gestational sac can be seen by 5 weeks menstrual age, and fetal heart activity by 6 weeks menstrual age. With abdominal scanning, these findings are first identified reliably a week later, at 6 and 7 weeks, respectively.
Crown-rump length is the most accurate dimension for assessing gestational age in the first trimester, with a 95% confidence interval of 6 2 to 3.5 days (3). Measurement of the gestational sac diameter can also be used to estimate age, although it is not as accurate as a result of variability in the shape of the sac. Fetal biparietal diameter and abdominal circumference are also relatively good predictors of menstrual age in the first trimester (4).
TABLE 12-1 RELATIONSHIPS AMONG SELECTED FETAL INDICES AS MEASURED BY ULTRASOUND AND GESTATIONAL AGE AS DETERMINED BY MENSTRUAL WEEKS | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Second- and Third-Trimester Assessment
After 12 weeks of gestation, the crown-rump length is difficult to obtain accurately. In the second and third trimesters, the main parameters of fetal age are the BPD, head circumference, abdominal circumference, and femoral length (Table 12-1).
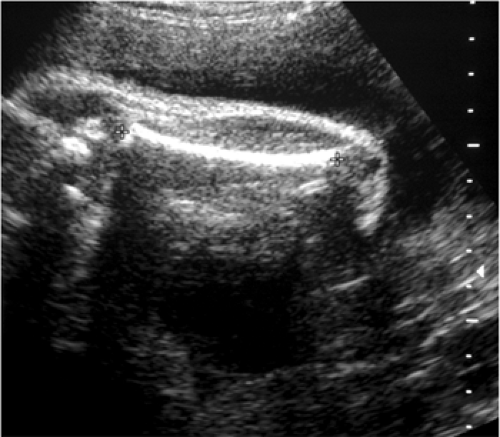
The fetal BPD is quick, reliable, and easy to obtain. It measures the transverse diameter of the upper midbrain at the level of the thalamic nuclei and cavum septum pellucidum from the external surface of one proximal parietal bone to the inner surface of the contralateral parietal bone (Fig. 12-1) (5). The earlier the gestational age the greater the predictive accuracy of this measurement.
Inaccuracies in measurements of the BPD may result from improper selection of the measurement plane (6). In late pregnancy, the fetal head may be too low in the pelvis to measure. Cranial molding, either from fetal position or oligohydramnios, may result in BPD measurements that do not accurately reflect true gestational age (Fig. 12-2).
The cephalic index, which measures the relationship between the short and long axes of the fetal head, should be measured if the head shape appears abnormal. If this index is below 70 or above 86, the biparietal diameter should not be used in the age and weight estimates (7). The accuracy of BPD measurements decreases with advancing gestational age. In the second trimester, a BPD measurement carries a predictive accuracy of ±7 days, whereas in the late third trimester it carries a predictive accuracy of ±3 weeks (7). Serial measurements of BPD can improve the predictive accuracy (8). The fetal head circumference is obtained from the same axial image used for the BPD. This measurement is more accurate than the BPD in the third trimester, as it is less affected by shape (7).
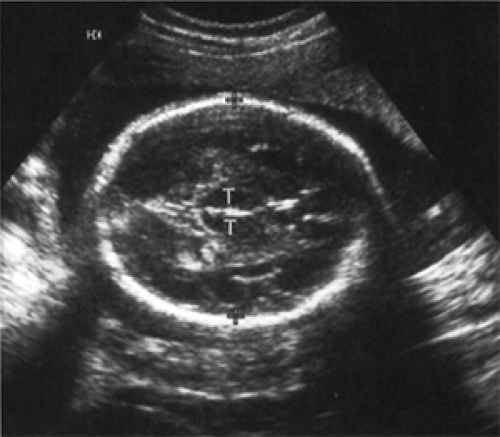 Figure 12-1 Fetal biparietal diameter (BPD). Axial scan of the head at the standardized level for BPD measurement shows the thalami. |
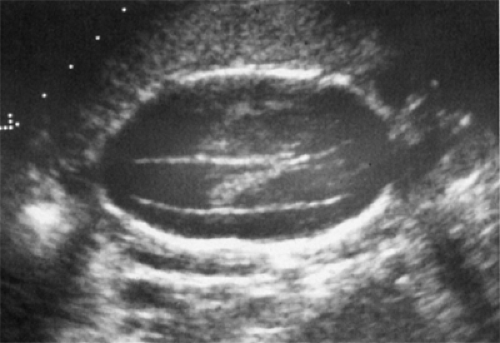 Figure 12-2 Transverse image of the brain of a 23-week fetus with severe oligohydramnios demonstrates a narrow and elongated skull. Cephalic index was abnormally low. |
The measurement of the fetal abdominal circumference is made from an axial image of the abdomen at the level of the portal vein. The circumference of the head is typically larger than the abdominal circumference up to 34 weeks of gestation, and the abdomen becomes larger thereafter. In the presence of intrauterine growth retardation (IUGR), head size tends to be preserved compared to abdominal size altering the head circumference to abdominal circumference ratio.
Femur length is defined as the distance between the greater trochanter and the distal end of the femur (Fig. 12-3) (9). Gestational age prediction from femur length is subject to error either from measurement difficulties caused by difficulty in visualizing the ends of the bone or from biological variation. The predictive accuracy of femur length ranges from ±1 week at 12 weeks of gestation to ±3 weeks at 36 weeks of gestation (10).
Estimation of fetal age is best accomplished using a composite assessment of multiple fetal measurements. A combination of head size (BPD or head circumference), femur length, and abdominal circumference is most commonly used. Estimates have an error of ±1.46 weeks between 24 and 30 weeks of gestation and increase to 2.3 weeks at 36 weeks of gestation (11). Individual measurements should not be used for assessing gestational age when they are affected by a pathological process; for example, head measurements in a hydrocephalic fetus or long bone measurements in the fetus with a bone dysplasia. After 22 weeks, age-independent fetal body ratios are useful in identifying asymmetric measurements. If the cephalic index is normal, the ratio of femur length to BPD can be measured, with normal results ranging between 71 and 87. The ratio of femur length to abdominal circumference should range between 20 and 24 (12).
FETAL WEIGHT ESTIMATES
It would be helpful in the assessment of fetal age, growth, and maturity if an accurate, reproducible method of determining fetal weight were available. Ultrasonographic estimates of fetal weight have been derived from single measurements such as BPD or abdominal circumference (13) and by a combination of measurements such as abdominal circumference and BPD (14). All ultrasonographic methods for fetal weight estimations, however, contain inherent error. Measurement of abdominal circumference yields an average error of 18% (13). The BPD and abdominal circumference yield a similar error (20%) (15). The absolute estimated error decreases as birth weight decreases.
The use of multiple parameters, especially head, abdomen, and femur measurements, provides the most accurate measurement of fetal weight. However, it is still not accurate in extremely low or high birth weight fetuses. Because fetal weight estimates remain imprecise, estimation of fetal age based solely on estimates of fetal weight should not be used. Incremental fetal weight change can be determined with serial ultrasounds and is one way of detecting abnormal fetal growth (10). In the future, three-dimensional fetal MRI reconstruction and volume estimates may improve the accuracy of fetal weight determination (16).
ASSESSMENT OF FETAL GROWTH
Fetal growth abnormalities are often associated with increased risk of perinatal morbidity and mortality. The rate of growth in the normal fetus varies with gestational age, with an increasing exponential curve in the first trimester, a linear curve in the second and most of the third trimester, and a decreasing exponential curve after 36 weeks of gestation (17). Serial ultrasonographic measurements can be plotted to evaluate fetal growth and may include weight estimates derived from a combination of these variables.
Intrauterine Growth Retardation
The infant whose birth weight is below the tenth percentile for gestational age is considered small for gestational age (SGA). The population of SGA infants whose weight falls below the tenth percentile is heterogeneous. Normal but small fetuses represent up to 60% of the SGA group, fetuses with congenital anomalies account for up to 15%, and fetuses with true IUGR account for 25% (18). Management varies among these groups. The normal but small fetus is not at increased risk and does not require intervention. The small fetus with true growth restriction may be at high morbidity or mortality risk and may require immediate intervention. The small infant with congenital abnormalities may or may not require intervention. It can be difficult determining which group an SGA fetus falls into, particularly when the true gestational age is unknown.
Ultrasound’s ability to identify the truly IUGR fetus is variable and is most successful when the disease state is severe. A slowing of the rate of head and femur growth is apparent with severe IUGR (19,20) but is more difficult to identify when the retardation is mild or early. Growth-adjusted sonographic age determination based on BPD or abdominal circumference (6,20) uses serial ultrasonographic measurements. This method assumes that fetal growth should remain within a narrow percentile band and that deviation from this may be an early sign of growth disorders (21). Because of the inherent errors, serial estimation of fetal weight identifies only the most severe growth disturbances. Asymmetric growth suggests IUGR. Abnormal ratios of head circumference to abdominal circumference, as a result of loss of liver mass with normal head growth, can be seen in severe IUGR but may not be present in milder cases (22).
Secondary signs aid in assessing the presence and severity of IUGR. Oligohydramnios often develops during episodes of uteroplacental insufficiency, most likely because of decreased fetal urine production and pulmonary fluid during episodes of fetal hypoxemia (23). Amniotic fluid volume may be assessed subjectively or by the semiquantitative method of measuring the vertical diameter of the largest visible pocket of amniotic fluid. The amniotic fluid index (AFI) is calculated by adding the vertical depths of the largest pocket in each of four equal uterine quadrants (24). Oligohydramnios has been defined by the absence of identifiable amniotic fluid pockets or when the maximum vertical pocket measures less than 2 cm in two perpendicular planes or when the amniotic fluid index measures less than 5 cm. Oligohydramnios as defined by any one of the methods is predictive of increased peripartum morbidity and mortality (24,25,26). Milder cases of IUGR, however, may not be associated with oligohydramnios (27).
Assessing fetal condition using the biophysical profile score (BPS) or Doppler velocity ratios of the umbilical artery and/or fetal middle cerebral artery are additional useful adjuncts in the diagnosis of IUGR (see Doppler Assessment of Blood Velocities in Umbilical and Fetal Vessels) (28). If a fetus who is being followed for IUGR has no signs of asphyxial compromise, continued observation rather than intervention may be reasonable.
Macrosomia
The infant whose birth weight is above the 90th percentile for gestational age is labeled large for dates (LGA) or macrosomic. This group of large infants is heterogeneous, composed of normal but large infants and infants with abnormally increased growth. Macrosomia is usually associated with maternal glucose abnormalities. Macrosomia may lead to obstetric complications such as shoulder dystocia, although maternal diabetes may cause neonatal complications such as hypoglycemia, polycythemia, and cardiac abnormalities (29). Detection of macrosomia sonographically includes serial assessment of growth and the relationship of the variables. The ratio of abdominal circumference to head circumference is particularly useful in identifying an enlarging abdomen indicative of excessive weight gain. Other measurements have been proposed to aid in the diagnosis of macrosomia, including soft tissue thickness of the humerus or femur and cheek-to-cheek diameter (30).
Fetal Maturity
The sonographic assessment of fetal maturity is useful in the optimal timing of perinatal management. The perinatologist must maintain a balance between the risk of fetal death and the risk of neonatal death based on an estimate of whether a fetus has reached an age and weight at which lung maturity is possible. Fetal age and weight determinations, evaluation of placental architecture, and the biophysical profile have been used to assess fetal maturity. Studies on elective deliveries based on BPD, or weight estimates based on BPD and abdominal circumference, have shown good results (31,32 and 33). The grading of placental maturity sonographically, however, has not been shown to be as accurate in assessing lung maturity as examination of the amniotic fluid (34).
FETAL ANATOMY
Congenital anomalies are present in 2% to 5% of newborns and account for 20% to 30% of perinatal deaths (35). High-resolution ultrasonography has produced significant
changes in the diagnosis and management of these anomalies, including the potential for therapeutic intervention. Factors to be considered in the counseling of these cases include gestational age, effect on maternal outcome, and neonatal prognosis with or without therapy. Amniocentesis should be considered in cases at risk for a chromosomal anomaly.
changes in the diagnosis and management of these anomalies, including the potential for therapeutic intervention. Factors to be considered in the counseling of these cases include gestational age, effect on maternal outcome, and neonatal prognosis with or without therapy. Amniocentesis should be considered in cases at risk for a chromosomal anomaly.
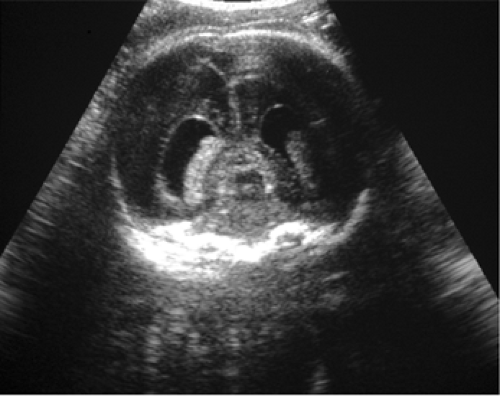 Figure 12-4 Transvaginal scan of the fetal brain in the coronal plane clearly demonstrates mild dilatation of both occipital horns. |
Ultrasound is the initial imaging modality of choice for the assessment of the fetus as it is safe, inexpensive, and easily performed. A comprehensive sonographic review includes a survey of the fetus, followed by evaluation of amniotic fluid volume, cord structure, and the placenta. A functional review of the fetus including hand clenching and swallowing is informative. Because some anomalies may not become evident until later in gestation (such as progressive hydrocephalus, congenital diaphragmatic hernia), follow-up evaluation of the fetus at risk is important. Transvaginal sonography and three-dimensional sonographic imaging have provided a means of improved visualization of fetal anomalies, particularly of the face and brain (Fig. 12-4).
Fetal Magnetic Resonance Imaging
Factors such as fetal lie, maternal obesity, and oligohydramnios may interfere with the sonographic evaluation of fetus. MRI is an alternative modality to evaluate the fetus as it uses no ionizing radiation, has excellent tissue contrast, large field of view and multiplanar capabilities (Fig. 12-5) (36,37). The development of faster scanning techniques now allow studies to be performed without sedation in the second trimester with superior contrast, and without significant motion artifact.
Although there currently is no evidence that the use of clinical MRI produces deleterious effects on human embryos, the safety of MRI during pregnancy has not been definitively demonstrated (37,38). While there has been concern that prolonged exposure to electromagnetic radiation may be linked to deleterious effects on embryogenesis, animal studies on embryos have so far demonstrated no growth abnormalities (40,41). Limited follow-up studies on children exposed to fetal MRI also have not demonstrated developmental abnormalities (40,42,43). Due to the possibility of unknown effects, MRI currently is used as a complementary study only when ultrasound results are inadequate for diagnosis or when MR imaging is expected to provide important additional information.
 Figure 12-5 Large field of view T2 weighted sagittal image demonstrates the brain, chest, abdomen, and leg of a 20 week fetus. |
With advances in the diagnosis and treatment of fetal abnormalities there is an increasing need for precise depiction of abnormalities. Fetal MRI not only confirms the presence of lesions noted by ultrasound, but also can demonstrate additional subtle anomalies. This information helps appropriate specialists, including the neonatologist, counsel families when difficult decisions must be made regarding early and potentially invasive intervention and allows for optimal delivery planning.
Fetal Central Nervous System Abnormalities
Fetal central nervous system (CNS) abnormalities may be detected in the first trimester in severe cases such as anencephaly. The most favorable time to evaluate the fetal neural axis, however, is 18 to 24 weeks of gestation, when resolution is sufficient to identify most structures including the spine. Abnormal measurements of BPD and head circumference may be the first suggestion of a CNS abnormality. Structural evaluation includes the shape and size of the head, ventricles, and posterior fossa and an evaluation of the spine. If a CNS anomaly is identified, careful evaluation for other anomalies, especially of the face, heart, and kidneys, follows.
The ventricular diameter normally measures less than 10 mm throughout the second and third trimesters
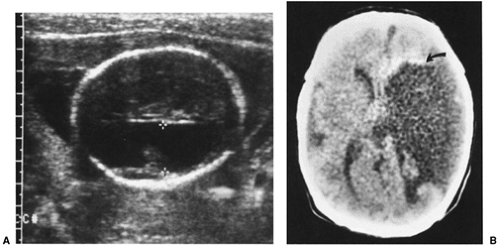
(44,45). Other criteria of ventriculomegaly include separation of choroid plexus from the medial ventricular wall. If the diagnosis of ventriculomegaly is established, a search for its etiology should be made. A differential diagnosis ranges from cerebral atrophy (hydranencephaly, porencephaly) (Fig. 12-6), dysgenesis (holoprosencephaly, agenesis of the corpus callosum), to true hydrocephalus.
(44,45). Other criteria of ventriculomegaly include separation of choroid plexus from the medial ventricular wall. If the diagnosis of ventriculomegaly is established, a search for its etiology should be made. A differential diagnosis ranges from cerebral atrophy (hydranencephaly, porencephaly) (Fig. 12-6), dysgenesis (holoprosencephaly, agenesis of the corpus callosum), to true hydrocephalus.
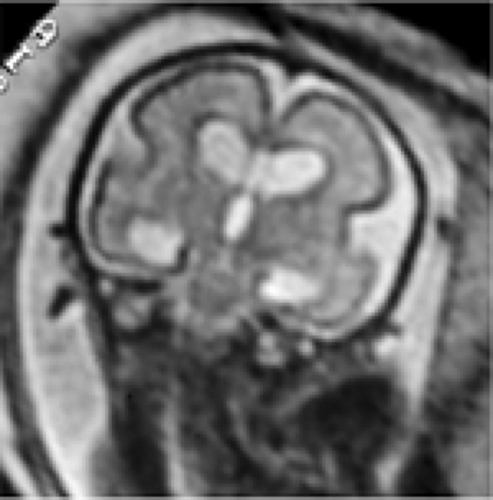
There are significant limitations in the sonographic evaluation of the fetal brain as a result of refraction artifact from the skull and low sensitivity to cortical malformations. MRI better defines anomalies of the posterior fossa, corpus callosum, and developing gray and white matter. Three planes of the brain can be obtained with excellent delineation of the extraaxial spaces (Fig. 12-7). Sulcal and gyral development can be assessed allowing for estimation of brain maturity (Fig. 12-8) (46,47 and 48).
Hydrocephalus
Hydrocephalus can be caused by an increased rate of cerebrospinal fluid (CSF) formation as in choroid plexus papilloma, decreased resorption of CSF after hemorrhage, or obstruction of CSF flow as a result of tumor or aqueductal stenosis (49). In many cases, the etiology of hydrocephalus remains unknown. Up to 85% of cases are associated with other neurological, cardiac, renal, gastrointestinal (GI), or skeletal anomalies. Up to 10% are associated with chromosomal abnormalities (50). Fetuses with other anatomic or chromosomal abnormalities have a grim prognosis for long-term development. When ventriculomegaly is mild, and no associated abnormalities are identified, outcome is less severe. Up to 20% of these cases, however, may demonstrate neurological abnormalities later in life (51,52 and 53).
 Figure 12-8 Oblique T2 weighted image through the brain of a 32 week fetus with trisomy 21 demonstrates moderate ventriculomegaly with a more mature sulcation pattern. |
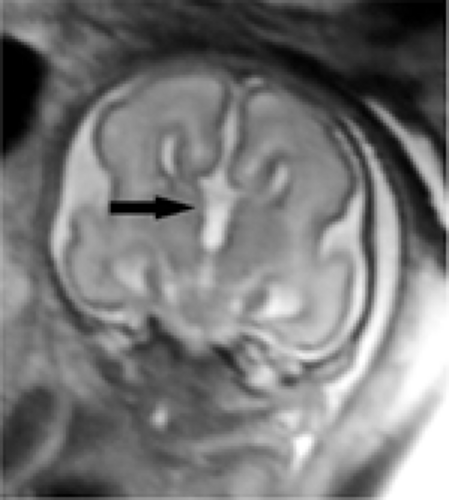 Figure 12-9 Coronal T2 weighted image through the brain of 19 week gestation demonstrates agenesis of the corpus callosum and high riding third ventricle. |
MRI is useful in confirming the presence of ventriculomegaly, and can assess symmetry of ventricular size and contour. Irregularity of the ventricular wall and adjacent parenchymal abnormalities may indicate post inflammatory and destructive changes. Atrophy, hemorrhages, or masses may be identified (48). Identifying the etiology for ventriculomegaly, however, may still be difficult as subtle gyral abnormalities and parenchymal changes may be impossible to detect by MRI in the second trimester.
Multiplanar views are particularly useful in the evaluation of the corpus callosum, which develops between 8 to 17 weeks gestation (Fig. 12-9). When severe, holoprosencephaly can be identified by ultrasound; less severe semilobar and lobar types are more difficult to diagnose even by MRI.
The posterior fossa and brain stem are well delineated by MRI and can help differentiate Dandy Walker malformation for posterior fossa arachnoid cysts or mega cisterna magna (Fig 12-10).
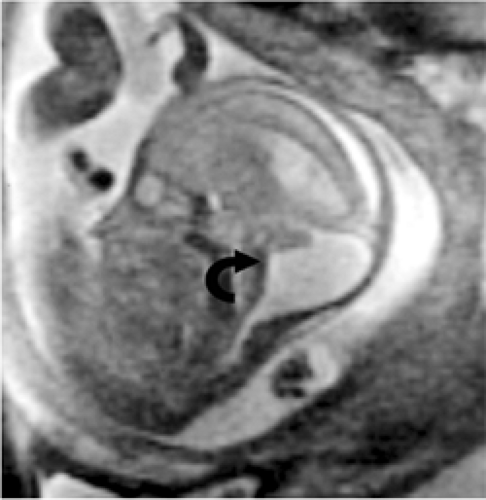 Figure 12-10 Sagittal T2 weighted image of a 22 week gestation demonstrates a Dandy Walker cyst with absent inferior vermis. |
Vascular CNS anomalies including vein of Galen aneurysms are well demonstrated by MRI. Hemorrhage and or encephalomalacia suggests a poorer prognosis and is better demonstrated by MRI.
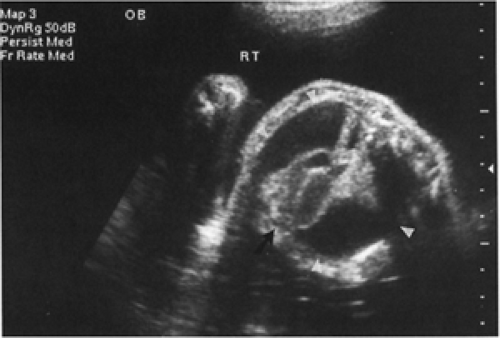
Neural Tube Defects
The most common condition leading to ventriculomegaly is spina bifida. Evaluation of the fetal spine and cerebellum allows prenatal identification of over 95% of fetuses with meningomyeloceles. Screening programs using maternal serum α-fetoprotein identify pregnancies at risk for neural tube or ventral wall defects. Sonographic findings of meningomyelocele include splaying of pedicles, presence of a cystic collection posterior to the fetal spine with absent skin covering, and scoliosis. Because of the difficulty in identifying small spinal defects prenatally, the association of cranial abnormalities is useful in evaluating cases at risk. The Arnold-Chiari malformation, which often accompanies spina bifida, results in the herniation of the cerebellum through the foramen magnum into the upper cervical spinal canal. Cranial sonographic findings of this malformation include frontal bone scalloping (lemon sign), abnormal curvature of the cerebellum (banana sign), and obliteration of the cisterna magna (54,55). MRI is useful in the confirmation of Chiari malformations, with amount of tonsillar herniation measured (46).
Cranial defects involving brain (encephalocele) or meninges (meningocele) may present with ventriculomegaly (Fig 12-11). Typically on ultrasonography there is a posterior paracranial mass that is cystic or solid. It is important to identify a true skull defect because the diagnosis can be confused with scalp edema, cystic hygroma, or scalp hemangiomas, which carry a better prognosis (56). MRI is particularly useful in identifying intracranial anomalies associated with encephaloceles. Because encephalocele is a feature of other syndromes including Meckel-Gruber, additional anomalies should be excluded (57).
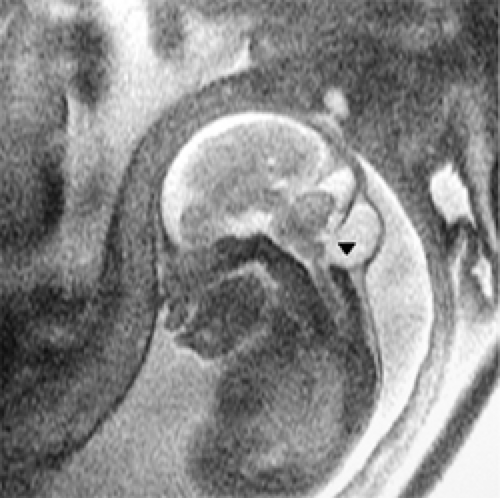 Figure 12-11 Sagitta T2 weighted image of a 24 week fetus demonstrates an occipital meningocele with microcephaly and sulcation anomalies. |
Fetal Chest Abnormalities
Many major intrathoracic structures can be identified sonographically by the second trimester. A small chest circumference suggests pulmonary hypoplasia in the presence of oligohydramnios or skeletal dysplasia (58). Pleural effusions appear as fluid collections surrounding collapsed echogenic lung (Fig. 12-12). Effusions may be primary in chylothorax or secondary in nonimmune hydrops. In the presence of effusions, prognosis is variable, with 15% mortality if an effusion is isolated but up to 95% mortality if it is associated with severe hydrops (59,60).
The normal fetal mediastinum lies in the center of the chest, anterior to the spine, with the cardiac interventricular septum forming a 45-degree angle with the midline. Deviation of this axis or shift of the heart suggests a mass effect or cardiac pathology.
Fetal lung parenchyma should be homogeneously echogenic. If it is heterogenous and/or there is shift of midline structures, a chest mass is likely. Sonographic findings will vary depending on the type of chest mass. Cystic adenomatoid malformations (CCAM) type 1 are the most common and appear as a single or multiple macrocysts. Type 2 CCAM contain small cysts less than 1 cm in size and are often associated with other anomalies. Type 3 CCAM contain multiple microcysts that appear sonographically as a homogeneously echogenic mass (Fig. 12-13) (61,62). Sequestrations are intralobar or extralobar masses of pulmonary tissue that lack a tracheobronchial communication and have a vascular supply from the aorta. They present as a solid or mixed solid and cystic mass in the inferior portion of the chest (63). Up to 25% have a CCAM component that may be cystic. With color Doppler, a vessel can often be seen coursing from the aorta to feed the mass, confirming the diagnosis. Bronchogenic cysts typically present as a simple mediastinal or lower lobe cyst without a feeding vessel (64).
MRI is particularly valuable in the evaluation of fetal thorax. Fetal lungs are homogeneously intermediate in signal and clearly delineated from mediastinal structures, liver, and bowel (64,65). Cystic lung masses are typically higher in signal as a result of the high fluid content and can be separated from normal surrounding lung parenchyma (Fig. 12-14a and b) (67,68).
Prognosis depends on the size of the intrathoracic mass because marked lung compression during fetal development leads to hypoplastic lungs. Polyhydramnios, ascites, and hydrops are likely secondary to compression of the esophagus and vena cava and correlate with poor outcome (61). Type 3 CCAM tend to have the worst prognosis. The prenatal placement of shunts in cysts or pleura has resulted in some success in lung reexpansion (68). Spontaneous resolution of pleural effusions and pulmonary masses in utero has been reported (Fig. 12-13) (60,61,62). Prenatal therapy is reserved for those cases at highest risk for poor outcome (e.g., hydrops) (61,69,70,71). A fetus with a lung mass has an excellent prognosis if there is no hydrops and only minimal pulmonary hypoplasia (71).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree