Baseline Rate
The normal fetus exhibits an overall constancy in its heart rate that can be considered comparable in nature to the resting heart rate of an adult. Most people maintain a certain average heart rate at rest. Although that rate changes with activity or excitement, it is expected to return to its usual rate when such stimuli are not present. This is also true of the fetus.
As explained in more detail in
Chapter 1, the FHR is controlled by a number of mechanisms. These include the central nervous system (CNS), the autonomic nervous system (ANS), baroreceptors, chemoreceptors, and the endocrine system. As was also explained (see
Chapter 2), the recorded trend of the FHR on the strip chart is calculated from the time intervals that elapse between successive beats of the fetal heart. Normally, this interval varies slightly from one beat to the next, causing a certain degree of fluctuation to appear in the trend of the baseline FHR. The bulk of these fluctuations, however, are contained within a constant range that is recognized as the FHR
baseline. According to the
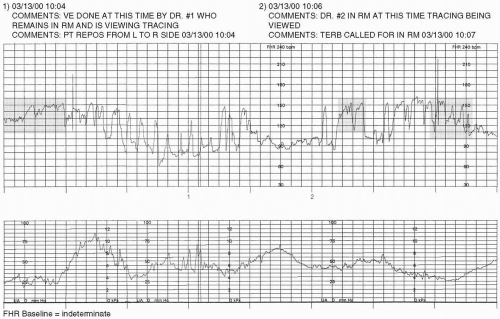
NICHD (1997), “Baseline FHR is the approximate mean FHR rounded to increments of 5 bpm during a 10-minute segment, excluding periodic or episodic changes; periods of marked FHR variability; and segments of the baseline that differ by more than 25 bpm.” For example, if the range of the baseline FHR is visualized to be 132 to 140 bpm, the mean FHR would be arrived at by adding these two integers (132 + 140)
and dividing the result by 2 (272 ÷ 2). The mean (in this case, 136) would then be rounded to the nearest increment of 5 (in this case, 135), if necessary. This is not intended to entail an intricate mathematical calculation, but rather a simple visual assessment and interpretation. It is also important to know that there are periods during which the FHR baseline cannot be assessed and/or interpreted. “In any 10-minute window, the minimum baseline duration must be at least 2 minutes or the baseline for that period would be indeterminate” (1997). In this case, one may need to refer to the previous 10-minute segment(s) to determine the baseline (
NICHD, 1997).
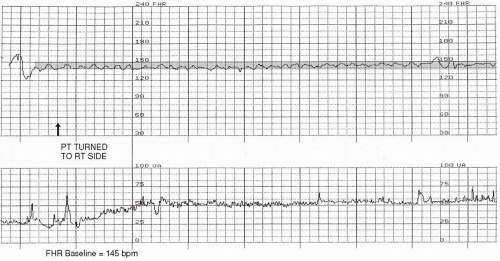
The baseline is the first characteristic of the FHR to be evaluated, because it is the parameter against which all other facets of the interpretation process are based. The baseline is assessed only when the patient is not experiencing contractions and when the FHR is not exhibiting signs of periodic/episodic changes (ie, accelerations or decelerations, which will be detailed later in this chapter). It is necessary to have a minimum of 10 minutes of FHR recorded to determine the baseline. The FHR baseline is expected to be maintained between a range of numbers that are within the limits of 110 to 160 bpm (
NICHD, 1997;
ACOG, 2005) (
Fig. 3-1).
Finding the FHR baseline is more than just looking at a segment of the strip chart and noting the lowest and highest points where the FHR was recorded. It requires critically evaluating the trend of the FHR at the appropriate times (between contractions and between periodic/episodic changes) to determine the integers between which the bulk of the relevant data are contained. Once the baseline FHR is initially identified for the particular portion of the tracing that is being evaluated, it is useful to reconfirm that finding at other points within the relevant segment of the tracing to ensure accuracy.
Variability
As has been mentioned in
Chapters 1 and
2, there are normal physiologic variations in the time intervals that elapse between each fetal heart beat. When the FHR is displayed on the strip chart,
these variations are visually apparent in the recorded trend of the FHR (see
Appendix F). Fluctuation of the FHR baseline is referred to as
variability. Variability is a component of baseline FHR data and, therefore, can only be assessed during the same time periods that it is appropriate to assess the baseline FHR (ie, between contractions and between periodic/episodic changes).
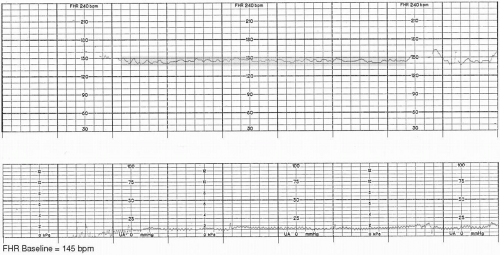
Moderate Variability
The presence of a moderate amount of variability indicates that the autonomic and central nervous systems of the fetus are well developed and well oxygenated. Its presence is also a reassuring indication that the fetus is maintaining a measure of tolerance to the changes in blood flow that occur during labor. A moderate amount of variability is considered to be fluctuation in the FHR baseline of as little as 6 bpm to as much as 25 bpm (
Fig. 3-2).
Moderate variability is one of the most important and predictive aspects of the FHR recording. Even if decelerations are occurring, the presence of moderate variability is highly correlated with the
absence of significant metabolic acidosis (
Parer, King, Flanders, Fox, & Kilpatrick, 2006). Therefore, attention to and accurate assessment of variability are essential components in the practice of EFM.
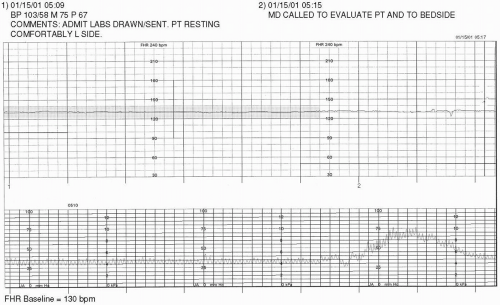
Minimal Variability
It may be cause for concern if the FHR baseline appears to have a minimal (≤5 bpm) or absent (no visible fluctuation) (
NICHD, 1997) amount of variability, because this finding may signify the presence of fetal hypoxia/acidosis. It is important to put the finding of decreased variability within the context of the entire clinical picture, however, to accurately determine its meaning.
As discussed in
Chapter 1, any condition or event that diminishes blood flow to the placenta deprives the fetus of adequate oxygenation and, if the resulting hypoxemia is sufficient to cause tissue hypoxia and metabolic acidosis, can create a loss of FHR baseline variability. Hypoxic causes of minimal or absent variability are related to diminished blood flow across the placenta or through the umbilical cord. Initially,
moderate variability may remain present, indicating that the fetus is effectively compensating for the diminished influx of oxygenated blood. If the cause of decreased perfusion is not corrected, however, variability eventually decreases. This is a warning sign, indicating that the fetus is losing its ability to tolerate or compensate for the stressors placed on it and is becoming hypoxic (
Fig. 3-3).
The overall correlation between acidemia and minimal or undetectable FHR baseline variability in the presence of decelerations is only 23%. However, deepening of decelerations over time in association with minimal or undetectable FHR baseline variability may serve as an indicator for intervention (
Parer et al., 2006).
Besides hypoxia/acidosis, there are other, more common reasons for the fetus to exhibit minimal baseline variability. These include fetal sleep, the effects of medications, an immature CNS, fetal dysrhythmias, and cardiac or CNS anomalies. Although fetal sleep is a common cause of minimal variability, it is necessary to remember that this is a transient state that should alternate with periods of moderate variability approximately every 20 to 40 minutes, and represents normal fetal physiologic function (
Schifrin, 1990).
Medications that depress the maternal CNS are likely to produce similar effects on the fetal CNS. Although it is to be expected that variability will decrease after the administration of such medications, this effect on the fetus is temporary. Once the medication is metabolized and excreted, variability will return. It is, therefore, prudent to administer such medications only after fetal well-being has been established. Also, it is important to review the patient’s medication history with her, because she may have knowingly or unknowingly exposed the fetus to a sedative or narcotic agent. Loss of variability secondary to medication effect does not require intervention.
The fetus who is less than 32 weeks’ gestation may exhibit less variability, because the ANS may not yet be fully developed (see
Chapter 1). It is important to note that, regardless of gestational age, once a fetus has exhibited a certain amount of variability, it has set a standard to which it should be held from that point forward.
Minimal or absent variability is often noted in association with patterns of fetal dysrhythmia. It is also found in the FHR tracings of fetuses with anomalies that affect cardiac, CNS, or ANS functioning. If minimal or absent variability is persistent from the commencement of monitoring and its cause is not known, further investigation is needed (
Fig. 3-4). If cardiac or CNS anomalies have not previously been ruled out by sonographic examination, it is advisable to have such testing performed.
Steps should be taken to remediate condition(s) suspected of causing minimal or absent variability. These include increasing fetal oxygenation by optimizing blood flow to and through the uterus, placenta, and umbilical cord. This is accomplished by promoting maternal cardiac and hemodynamic functioning (assess maternal vital signs and history; initiate therapies such as position changes and administration of medications, hydration, and oxygen as needed), uteroplacental perfusion (through maternal positioning and eliminating stress of uterine contractions), and blood flow through the umbilical cord (alleviate pressure through maternal positioning). Research utilizing fetal arterial oxygen saturation monitoring (a method of measuring fetal oxygenation directly) scientifically supported that an IV fluid bolus of 1,000 mL, the maternal lateral position, and oxygen administration of 10 L/min with a nonrebreather face mask for 15 minutes improves fetal oxygenation (
Simpson & James, 2005). Not all instances of hypoxia can be alleviated with such interventions, but it is necessary to perform them in an attempt to oxygenate the fetus as much as possible. If minimal or absent variability is noted at the outset of the monitoring session and there are no other components of the FHR that can be considered reassuring (such as accelerations, which are discussed later in this chapter), then hypoxia should be ruled out. It is possible that a prior hypoxic insult has occurred (
Phelan & Ahn, 1994;
Schifrin, Hamilton-Rubinstein & Shields, 1994) (
Table 3-1).
Marked Variability
The presence of more than 25 beats of fluctuation in the FHR baseline is known as
marked variability (
NICHD, 1997) (
Fig. 3-5). This pattern is only usually seen intrapartum. Although marked
variability is sometimes caused by fetal activity or stimulation, it can also be a sign that the fetus is hemodynamically compromised or mildly hypoxemic (
Parer, 1997). Once again, to put any finding in perspective, it is necessary to consider the entire clinical picture. Query the patient on her perception of fetal activity and attempt to objectively affirm and identify sources of the same. Ensure optimal blood flow to and through the uterus, placenta, and umbilical cord by promoting maternal cardiac and hemodynamic functioning (assess maternal vital signs and history; initiate therapies such as position changes and administration of medications, hydration, and oxygen, as needed). Promote uteroplacental perfusion through maternal positioning and eliminating stress of uterine contractions, and blood flow through the umbilical cord (alleviate pressure through maternal position changes) (
Table 3-2).
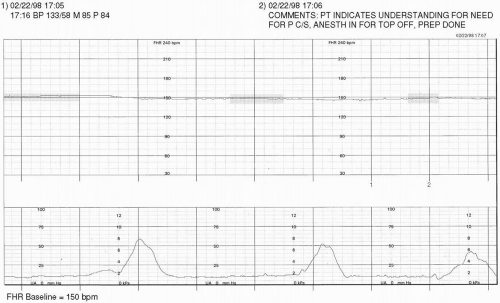
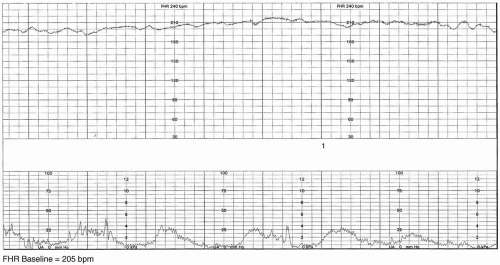
Tachycardia
If the baseline FHR rises and is maintained above 160 bpm for 10 minutes or longer, this is considered to be a fetal tachycardia (
NICHD, 1997). A fetal tachycardia may be maternal or fetal in origin. Common conditions that increase maternal heart rate (subsequently raising the FHR) include fever, dehydration, and medication effect. Remediation of the cause of the maternal tachycardia will usually assist the FHR in returning to normal range if the tachycardia is solely of maternal etiology.
Tachycardia may also result from hypoxia/acidosis, infection, and tachydysrhythmias. The onset of tachycardia or a rising baseline rate should be considered serious, because it is one of the first signs that the fetus is becoming hypoxic/acidotic. As described previously (see
Chapter 1), when there is decreased maternal-fetal perfusion, baroreceptors and chemoreceptors in the fetus trigger an increase in the FHR. In many instances, care providers do have influence over maternal-fetal exchange. This includes avoiding problems such as uterine hyperstimulation (
Fig. 3-6) and maternal hypotension. In either of these cases, correcting the cause (eg, discontinuing oxytocin, removal/reversal of uterotonic agents, changing the maternal position) may improve fetal oxygenation and assist the FHR in recovery to normal range. In the event of infection or tachydysrhythmia, the usual means of intrauterine resuscitation should be employed (ie, position changes, increased maternal hydration and oxygenation, and decreasing stressors on the fetus such as contractions) in addition to any other medical or pharmaceutical remedies ordered (
Table 3-3).