Ninety-nine percent of women of reproductive age (15 to 44 years old) in the United States have used at least one contraceptive method and 62% are currently using contraception.
Among women affected by unintended pregnancy, 60% report contraceptive use in the month prior to the pregnancy, suggesting incorrect or inconsistent use of their chosen method(s).
Increasing the use of long-term, highly effective methods, such as intrauterine devices and implantable contraceptives, may reduce the number of unintended pregnancies.
Contraceptive use is associated with improved health outcomes for women and children.
Contraceptive use prevents obstetric complications by facilitating birth spacing and preventing unintended pregnancies at the extremes of reproductive age.
Noncontraceptive benefits of hormonal contraception include improvement in menstrual and perimenstrual symptoms, bleeding patterns, and acne and decreased risk of developing ovarian and endometrial cancer.
Physicians can optimize consistent long-term use of contraception among their patients through counseling that takes into account medical history, ethical and religious concerns, the patient’s short- and long-term childbearing plans, and prior contraceptive use history.
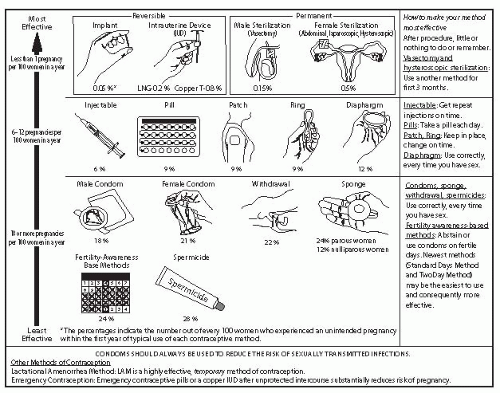
Table 32-1 lists contraceptive methods available in the Unites States, along with their perfect-use and typical-use failure rates.
Contraceptive methods can be considered in terms of “tiers of effectiveness” based on pregnancy rates with typical use.
TABLE 32-1 Efficacy of Various Contraceptive Methods
Method
Typical Use
Perfect Use
No method
85
85
Spermicides
29
18
Withdrawal
27
4
Periodic abstinence
Calendar
25
9
Standard days method
12
5
Ovulation method
25
3
Symptothermal
25
2
Postovulation
25
1
Diaphragm with spermicide
16
6
Condom
Female
21
5
Male
15
2
Pill (combined)
8
0.3
Mini-pill (progestin-only)
13
1.1
Patch (Ortho Evra)
8
0.3
Vaginal ring (NuvaRing)
8
0.3
Depo Provera
3
0.3
Implant (Implanon)
0.05
0.05
IUD
Copper T (ParaGard)
0.8
0.6
Levonorgestrel IUS (Mirena)
0.2
0.2
Female sterilization
0.5
0.5
Male sterilization
0.15
0.10
IUD, intrauterine device; IUS, intrauterine system.
An example of a visual aid that can be used for patient counseling is shown in Figure 32-1.
In this chapter, we will discuss methods in approximate descending order of effectiveness.
Another useful resource is the Centers for Disease Control and Prevention’s (CDC’s) U.S. Medical Eligibility Criteria for Contraceptive Use (US MEC), which can be consulted to determine safe contraceptive methods for women with medical comorbidities (Table 32-2).
This resource, available online and as a downloadable “app,” provides guidance for safe use of contraceptives; it does not address comparative risks of pregnancy in women with medical conditions.
Bilateral tubal ligation (BTL) is a surgical procedure in which the fallopian tubes are permanently occluded, preventing sperm from fertilizing the ovum. The procedure
can be performed postpartum (within 48 hours after vaginal delivery), at the time of cesarean delivery, or as an interval procedure (>6 weeks postpartum) via laparoscopic or transcervical hysteroscopic approach.
The Parkland and Pomeroy salpingectomies are the most common methods used for postpartum sterilization. These involve ligating and excising portions of the tubes via an infraumbilical incision.
Laparoscopic tubal ligation is performed via banding, clipping, or cauterizing the tubes.
The Collaborative Review of Sterilization (CREST) study, a landmark analysis of tubal sterilization, compared the long-term effectiveness of numerous methods of sterilization and found a rate of 18.5 pregnancies per 1,000 procedures overall (Table 32-3).
Advantages of transabdominal sterilization include the fact that these procedures offer highly effective, permanent contraception to women who desire no future childbearing. Sterilization may decrease the risk of ovarian cancer, possibly by blocking carcinogens from ascending through the fallopian tubes.
Disadvantages include the need for anesthesia for sterilization via an abdominal approach, risk of surgical complications, and sterilization failure resulting in either intrauterine or ectopic pregnancy. Sterilization failure rates are higher for women younger than the age of 30 years because these women are more fertile at the time of sterilization.
The reported 10-year cumulative probability of ectopic pregnancy for all sterilization methods in the CREST study was 7/1,000, with greater risk of ectopic
pregnancy in younger women. However, although the relative risk of ectopic pregnancy (chance that a pregnancy, once it occurs, may be ectopic) may be higher after sterilization, the absolute risk of ectopic pregnancy is lower than in noncontracepting women due to the high efficacy of sterilization. The risk of regret of sterilization is significantly higher in women sterilized prior to age 30 years.
TABLE 32-2 Contraindications to Estrogen-Containing Hormonal Contraception
Moderate or severe uncontrolled HTN
History of CVA or MI
Multiple risk factors for CAD: age, smoking, HTN, DM
History of or current DVT/PE
Migraines with aura or focal neurologic symptoms
Active hepatoma or liver cirrhosis or unexplained elevation of liver enzymes
Known or suspected breast cancer
Smoking >15 cigarettes per day and age >35 yr
Breast-feeding <6 wk postpartum (theoretic risk of growth restriction)
Diabetic neuropathy, retinopathy, neuropathy, or other vascular disease
Valvular heart disease, complicated (SBE, pulmonary HTN, or atrial fibrillation)
Known thrombogenic mutation
Migraines without aura and age >35 yr
Symptomatic gallbladder disease
Undiagnosed vaginal bleeding
Non-breast-feeding <3 wk postpartum
Category 4 (i.e., unacceptable risk) contraindications are listed.
HTN, hypertension; CVA, cerebrovascular accident; MI, myocardial infarction; CAD, coronary artery disease; DM, diabetes mellitus; DVT, deep vein thrombosis; PE, pulmonary embolism; SBE, subacute bacterial endocarditis.
From Centers for Disease Control and Prevention. U.S. medical eligibility criteria for contraceptive use, 2010. MMWR Recomm Rep 2010;59(RR-4):1-86.
TABLE 32-3 Failure Rates for Female Sterilization Methods
Method
% Pregnant in 10 years
Postpartum salpingectomy
0.75
Interval partial salpingectomy
2.0
Unipolar cautery
0.75
Bipolar cautery
2.48
Spring clip (Hulka clip)
3.65
Silastic bands (Falope ring)
1.77
Filshie clipa
0.9-1.2
a Not studied in CREST.
Data from Peterson HB, Xia Z, Hughes JM, et al. The risk of pregnancy after tubal sterilization: findings from the U.S. Collaborative Review of Sterilization. U.S. Collaborative Review of Sterilization Working Group. Am J Obstet Gynecol 1996;174:1161-1170; Kovacs GT, Krins AJ. Female sterilizations with Filshie clips: what is the risk failure? A retrospective survey of 30,000 applications. J Fam Plan Reprod Health Care 2002:28:34-35.
Essure is an irreversible method of transcervical hysteroscopic tubal occlusion that can be performed in the office or operating room. In this procedure, a 4-cm × 1-cm stainless steel and nickel-coated coil is inserted into each fallopian tube under hysteroscopic guidance. A local inflammatory response leads to tissue ingrowth around the coil and subsequent tubal occlusion. An alternative method of contraception must be used for 3 months afterward and until a hysterosalpingogram (HSG) confirms successful tubal occlusion.
Advantages to transcervical sterilization include the ability to perform these procedures in an office setting without risks associated with anesthesia and without the need for abdominal incisions.
This may be particularly important for women who desire permanent sterilization but are obese, have had multiple abdominal surgeries, or have serious medical comorbidities.
Disadvantages include a failure rate that may be higher than that seen after BTL and the need to comply with a postprocedure HSG to confirm success. Failure rate demonstrated from clinical trials was <1%, although postmarketing failure rates have been higher.
Most pregnancies result from noncompliance with the HSG protocol following an unsuccessful procedure or occur as interval pregnancies between the time of procedure and complete scarring.
Vasectomy is the surgical occlusion of the vas deferens, which prevents sperm from being ejaculated.
Up to 20 postprocedure ejaculations are required before the procedure becomes effective (as determined by two azoospermia results on semen analysis).
Vasectomy is highly effective and has no long-term side effects. It is also less expensive and associated with fewer complications than tubal ligation.
Vasectomy requires an outpatient surgical procedure, is permanent, offers no protection against sexually transmitted diseases (STDs), and is not immediately effective.
These may be excellent alternatives to sterilization, even in women who desire no further childbearing.
Long-acting methods become cost-effective after about a year of use and so can be considered for women with a wide range of fertility plans.
Intrauterine contraception, also known as intrauterine devices (IUD) or systems (IUS), is one of the most effective methods of reversible contraception. Choice of
terminology can be based on personal preference, but the term IUD is widely understood by providers and patients.
Two types are currently commercially available in the United States: the coppercontaining T380A and the levonorgestrel (LNG)-releasing IUS. Both are flexible plastic devices that are inserted into the uterus and cause a sterile inflammatory reaction in the uterus that interferes with sperm transport into and within the uterine cavity. The LNG-IUS also works through local progestin effects, such as the thickening of cervical mucus and atrophy of the endometrial lining.
The Copper T380 IUD (ParaGard) is effective for at least 10 years, likely 12. The copper IUD is also the most effective form of postcoital contraception (see “Postcoital Contraception” later).
There are now two LNG-releasing IUDs available in the United States: a 20-µg LNG/day device (Mirena) and a product that releases 14 µg LNG/day (Skyla) (both Bayer HealthCare Pharmaceuticals, Whippany, NJ). The 20-µg IUD is approved for 5 years in the United States and is likely effective for 7 years. A noncontraceptive benefit is the reduction of menstrual blood loss by up to 90% by suppressing growth of endometrial tissue. The 14-µg LNG IUD is effective for 3 years, after which the daily levels of LNG release decrease significantly.
Advantages: IUDs provide highly effective protection against pregnancy and are easily inserted and removed. The LNG-containing IUDs may correct menstrual bleeding abnormalities and improve anemia. IUDs may also provide protection against ascending pelvic infection and even protect against endometrial cancer. Return to fertility is rapid after removal.
Disadvantages/side effects: There are no hormonal side effects of the copper IUD. In some women, menstrual bleeding may be slightly heavier and longer in the initial months after insertion. This can generally be managed with nonsteroidal antiinflammatory drugs (NSAIDs). The LNG-IUDs may have hormonally related side effects, including irregular bleeding, which generally corrects after a few months of use. Oligomenorrhea or amenorrhea may occur with the LNG-IUD, which may not be desirable to some women. Some women may experience systemic hormonal side effects, although many will not.
Contraindications: There are few true contraindications to the use of IUDs. IUDs should not be used if pregnancy is suspected, if anatomic uterine abnormalities cause significant cavity distortion, if there is unexplained vaginal bleeding prior to appropriate medical workup, or if a pelvic malignancy is suspected. IUDs do not need to be removed, however, when cervical cancer or dysplasia is discovered and/or treated. Active pelvic infection is a contraindication; pelvic infection is further discussed in the following text. Although HIV infection does not contraindicate IUD placement, AIDS is considered to be a contraindication.
Risks: Risks of IUD insertion include expulsion (2%), perforation (1:1,000), pregnancy (2 to 8:1,000), and infection (uncommon).
Other considerations: Immediate postpregnancy (postpartum and postabortal) IUD placement is safe and may lead to a substantial decrease in unplanned pregnancy. Expulsion risk may be higher than when placement is not associated with pregnancy, but this risk can be balanced against other benefits and concerns.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree