 Figure 16–1. Leukocoria of the left eye caused by retrolental membrane (persistent hyperplastic primary vitreous or persistent fetal vasculature).
Figure 16–1. Leukocoria of the left eye caused by retrolental membrane (persistent hyperplastic primary vitreous or persistent fetal vasculature).
REFRACTIVE ERRORS
 Pathogenesis
Pathogenesis
Refractive error refers to the optical state of the eye (Figure 16–2). The shape of the cornea and, to a lesser extent, the shape of the lens and length of the eye play a role in the refractive state of the eye. Children at particular risk for refractive errors requiring correction with glasses include those who were born prematurely; have Down syndrome; have parents with refractive errors; or have certain systemic conditions such as Stickler, Marfan, or Ehlers-Danlos syndrome.
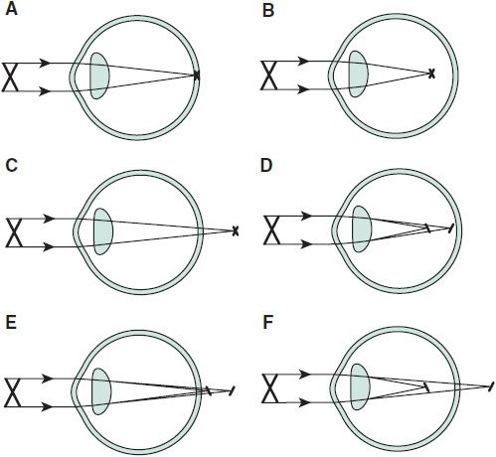
 Figure 16–2. Different refractive states of the eye. A: Emmetropia. Image plane from parallel rays of light falls on retina. B: Myopia. Image plane focuses anterior to retina. C: Hyperopia. Image plane focuses posterior to retina. D: Astigmatism, myopic type. Images in horizontal and vertical planes focus anterior to retina. E: Astigmatism, hyperopic type. Images in horizontal and vertical planes focus posterior to retina. F: Astigmatism, mixed type. Images in horizontal and vertical planes focus on either side of retina.
Figure 16–2. Different refractive states of the eye. A: Emmetropia. Image plane from parallel rays of light falls on retina. B: Myopia. Image plane focuses anterior to retina. C: Hyperopia. Image plane focuses posterior to retina. D: Astigmatism, myopic type. Images in horizontal and vertical planes focus anterior to retina. E: Astigmatism, hyperopic type. Images in horizontal and vertical planes focus posterior to retina. F: Astigmatism, mixed type. Images in horizontal and vertical planes focus on either side of retina.
 Diagnosis
Diagnosis
There are three common refractive errors: myopia, hyperopia, and astigmatism. Inequality of the refractive state between the two eyes (anisometropia) can cause amblyopia. The refractive state is determined by an eye care professional via a procedure called refraction. The determination of the refractive state in a preverbal child often proves challenging. If there is concern that there may be a significant problem with a preverbal child’s vision, they should be referred to an eye care professional specially trained for treating children.
 Treatment
Treatment
Not all refractive errors require correction, but severe errors can cause amblyopia (reduced vision with or without an organic lesion). Refractive errors in children are most commonly treated with glasses. Less often, contact lenses are required, usually for very high or asymmetrical refractive errors, or for adolescents who do not want to wear glasses. Laser refractive surgery is not indicated for most children.
MYOPIA (NEARSIGHTEDNESS)
For the myopic or nearsighted individual, objects nearby are in focus; those at a distance are blurred. This is because the plane of focus is anterior to the retina. The onset is typically at about age 8 years and may progress throughout adolescence and young adulthood. A myopic person may squint to produce a pinhole effect, which improves distance vision. Divergent lenses provide clear distance vision. Many studies have attempted to slow or stop myopic progression. Atropine eye drops have shown some effect, but produce many side effects. A newer drug, pirenzepine, has shown promise in animal studies, but human studies have not shown a significant decrease in myopic progression.
HYPEROPIA (FARSIGHTEDNESS)
Saying that the hyperopic child is sighted for far (not near) vision is somewhat misleading, because the child can focus on near objects if the hyperopia is not excessive. Large amounts of uncorrected hyperopia can cause esotropia (inward deviation, or crossing, of the eyes) and amblyopia (see later sections Amblyopia and Strabismus). Most infants have a hyperopic refraction that begins to diminish during the toddler years and does not require correction.
ASTIGMATISM
When either the cornea or the crystalline lens is not perfectly spherical, an image will not be sharply focused in one plane. Schematically, there will be two planes of focus. Both of the planes can be either in front of or behind the retina, or one of the planes can be in front of the retina and the other behind it. This refractive state is described as astigmatism. Large amounts of astigmatism not corrected at an early age can cause decreased vision from amblyopia, but proper refractive correction can prevent this.
OPHTHALMIC EXAMINATION
A history suggesting poor vision or misalignment of the eyes, visual acuity that falls outside the expected level for a specific age, eyelid malposition, abnormal pupil reactivity or shape, and presence of an asymmetric/abnormal red reflex requires referral to an ophthalmologist.
The American Academy of Pediatrics (AAP), American Association for Pediatric Ophthalmology and Strabismus (AAPOS), and the American Academy of Ophthalmology (AAO) policy statements for red reflex testing can be accessed at http://aappolicy.aappublications.org/.
Prompt detection and treatment of ocular conditions can prevent a lifetime of visual disability. The ophthalmic examination should be a part of every well-child assessment.
It is crucial to check newborn infants for vision or life-threatening conditions that present with an abnormal red reflex that may be caused by cataracts or intraocular tumors. Eyelid ptosis (droopy eyelid) that obstructs the visual axis can cause permanent visual acuity loss from deprivation amblyopia and/or induced astigmatism, and requires urgent consultation with an ophthalmologist.
From birth to 3 years of age, the ophthalmic examination should include taking a history for ocular problems, vision assessment, inspection of the eyelids and eyes, pupil examination, ocular motility assessment, and red reflex check.
The ophthalmic examination of children older than 3 years should include taking a history for ocular problems, inspection of the eyelids and eyes, pupil examination, ocular motility assessment, and red reflex check and visual acuity testing with Allen, Lea, HOTV, Tumbling E, or Snellen symbols. Direct ophthalmoscopy should be attempted. Testing of binocular status can be accomplished by various tests, including the Random Dot E stereoacuity test.
HISTORY
Evaluation begins with the chief complaint and history of the present illness. Elements of the ocular history include onset of the complaint, its duration, whether it is monocular or binocular, treatment received thus far, and associated systemic symptoms. If an infectious disease is suspected, ask about possible contact with others having similar findings. The history should include prior ocular disease, perinatal and developmental history, history of allergy, and history of familial ocular disorders.
VISUAL ACUITY
Visual acuity testing is the most important test of visual function and should be part of every general physical examination (http://one.aao.org/Flash/VisionScreening/PediatricVisionScreening.html). Acuity should be tested in each eye individually, using an adhesive eye patch to prevent peeking. Glasses that were previously prescribed should be worn during vision screening. In older children who can cooperate, use of a pinhole will improve vision in children not wearing the appropriate spectacle prescription.
Vision Screening
Vision screening in the pediatric age group is a challenge, especially in younger and developmentally delayed children. Accuracy of the screening test being administered to a particular population and expense in terms of time, equipment, and personnel are some factors that must be considered in choosing a screening test. Vision screening should be done at well child visits. Further information on vision screening can be found at the AAP website (http://www.aap.org). Risk factors that should be screened for because they interfere with normal visual development and are amblyogenic include media opacities (such as cataracts), strabismus (misalignment of the visual axes of the eyes), and refractive errors that are different in the two eyes (anisometropia) or of large magnitude in both eyes.
In the sleeping newborn, the presence of a blepharospastic response to bright light is an adequate response. At age 6 weeks, eye-to-eye contact with slow, following movements is usually present. By age 3 months, the infant should demonstrate fixing and following ocular movements for objects at a distance of 2–3 ft. At age 6 months, interest in movement across the room is the norm. Vision can be recorded for the presence or absence of fixing and following behavior, and whether vision is steady (unsteady when nystagmus is present) and maintained.
In the verbal child, the use of familiar icons will allow for a quantitative test. Allen or Lea symbols with familiar pictures can be used to test children 2–3 years of age. When it is not possible to measure visual acuity or assess alignment in the preschool-aged child, random dot stereopsis testing (for depth perception) is effective in screening for manifest strabismus and amblyopia, but this test may miss some cases of anisometropic (unequal refractive error) amblyopia and small-angle strabismus, and is not designed to detect refractive errors.
Four-year-old children are often ready to play the tumbling E game (in which the child identifies the orientation of the letter E, which is turned in one of four directions) or the HOTV letters game (in which these four letters are shown individually at a distance and matched on a board that the child is holding). Literate children are tested with Snellen letters. Typical acuity levels in developmentally appropriate children are approximately 20/60 or better in children younger than 2–3 years, 20/40–20/30 in 3-year-old children, 20/30–20/25 in 4-year-old children, and 20/20 in literate children 5–6 years old. Referral criteria for children 3–5 years of age include visual acuity of less than 20/40 or 10/20 in either eye or a two-line difference between the eyes. Children 6 years or older should be referred if their visual acuity is less than 20/30 or 20/15 in either eye or a two-line difference is noted between the eyes.
The practitioner should be aware of two situations in which vision screening is complicated by nystagmus. Children who require a face turn or torticollis (in which the head is tilted to the right or left) to quiet the nystagmus will have poor visual acuity results when tested in the absence of the compensatory head posture. When latent nystagmus is present, acuity testing is particularly challenging (see later section Nystagmus). Nystagmus appears or worsens when an eye is occluded, degrading central vision. To minimize the nystagmus, the occluder should be held about 12 in in front of the eye not being tested. Testing both eyes simultaneously without occlusion often gives a better visual acuity measurement than when either eye is tested individually.
Traditional vision screening methods using eye charts in children aged 3–5 years require the child’s cooperation as well as proficiency in testing by the examiner. Additional screening modalities including photoscreening and autorefractors have been used by various volunteer programs in schools, day care facilities, and physician offices. Photoscreening does not screen directly for amblyopia but for amblyogenic factors, which include strabismus, media opacities, eyelid ptosis, and refractive errors. Autorefractors can determine if there is a significant refractive error present in either eye or if there is a significant difference between the two eyes. Some autorefractors can also detect strabismus and eyelid ptosis. If the screening results suggest an amblyogenic factor, children are referred to an eye care professional for a complete eye examination. Problems exist with sensitivity and specificity of the instruments and poor follow-up for referrals to eye care professionals. The cost-effectiveness of various vision screening modalities remains an area of continued research.
Chou R, Dana T, Bougatsos C: Screening for visual impairment in children ages 1-5 years: update for the USPSTF. Pediatrics 2011;127(2):e442–e479 [PMID: 21282269].
Davidson S, Quinn GE: The impact of pediatric vision disorders in adulthood. Pediatrics 2011;127(2):334–339 [PMID: 21199855].
Miller JM, Lessin HR: American Academy of Pediatrics Section on Ophthalmology; Committee on Practice and Ambulatory Medicine; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Instrument-based pediatric vision screening policy statement. Pediatrics 2012;130(5):983–986 [PMID: 23109679].
EXTERNAL EXAMINATION
Inspection of the anterior segment of the globe and its adnexa requires adequate illumination and often magnification. A penlight provides good illumination and should be used in both straight-ahead and oblique illumination. A Wood lamp or a blue filter cap placed over a penlight is needed for evaluation after applying fluorescein. Immobilization of the child may be necessary. A drop of topical anesthetic may facilitate the examination.
In cases of suspected foreign body, pulling down on the lower lid provides excellent visualization of the inferior cul-de-sac (palpebral conjunctiva). Visualizing the upper cul-de-sac and superior bulbar conjunctiva is possible by having the patient look inferiorly while the upper lid is pulled away from the globe and the examiner peers into the upper recess. Illumination with a penlight is necessary. The upper lid should be everted to evaluate the superior tarsal conjunctiva (Figure 16–3).
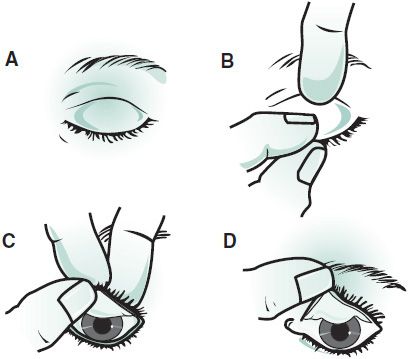
 Figure 16–3. Eversion of the upper lid. A: The patient looks downward. B: The fingers pull the lid down, and an index finger or cotton tip is placed on the upper tarsal border. C: The lid is pulled up over the finger. D: The lid is everted.
Figure 16–3. Eversion of the upper lid. A: The patient looks downward. B: The fingers pull the lid down, and an index finger or cotton tip is placed on the upper tarsal border. C: The lid is pulled up over the finger. D: The lid is everted.
When indicated for further evaluation of the cornea, a small amount of fluorescein solution should be instilled into the lower cul-de-sac. Blue light will stain defects yellow-green. Disease-specific staining patterns may be observed. For example, herpes simplex lesions of the corneal epithelium produce a dendrite or branchlike pattern. A foreign body lodged beneath the upper lid shows one or more vertical lines of stain on the cornea due to the constant movement of the foreign body over the cornea. Contact lens overwear produces a central staining pattern. A fine, scattered punctate pattern may be a sign of viral keratitis or medication toxicity. Punctate erosions of the inferior third of the cornea can be seen with staphylococcal blepharitis or exposure keratitis secondary to incomplete lid closure.
PUPILS
The pupils should be evaluated for reaction to light, regularity of shape, and equality of size as well as for the presence of afferent pupillary defect. This defect, which occurs in optic nerve disease, is evaluated by the swinging flashlight test (see later section Diseases of the Optic Nerve). Irregular pupils are associated with iritis, trauma, pupillary membranes, and structural defects such as iris coloboma (see later section on Iris Coloboma).
Pupils vary in size due to lighting conditions and age. In general, infants have miotic (constricted) pupils. Children have larger pupils than either infants or adults, whereas the elderly have miotic pupils.
Anisocoria, a size difference between the two pupils, may be physiologic if the size difference is within 1 mm and is the same in light and dark. Anisocoria occurs with Horner syndrome, third nerve palsy, Adie tonic pupil, iritis, and trauma. Medication could also cause abnormal pupil size or reactivity. For example, contact with atropine-like substances (belladonna alkaloids) will cause pupillary dilation and limit pupillary reaction. Systemic antihistamines and scopolamine patches, among other medicines, can dilate the pupils and interfere with accommodation (focusing).
ALIGNMENT & MOTILITY EVALUATION
Alignment and motility should be tested because amblyopia is associated with strabismus. Besides alignment, ocular rotations should be evaluated in the six cardinal positions of gaze (Table 16–1; Figure 16–4). A small toy is an interesting target for testing ocular rotations in infants; a penlight works well in older children.
Table 16–1. Function and innervation of each of the extraocular muscles.
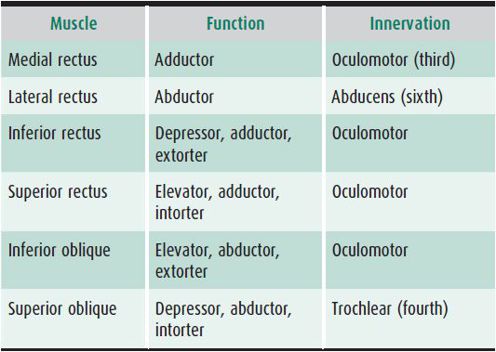
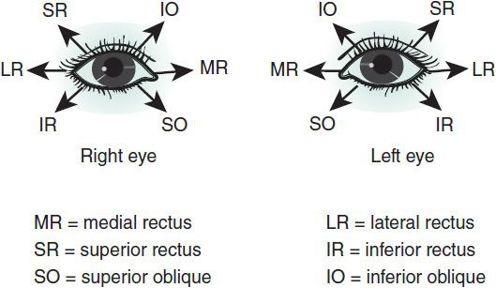
 Figure 16–4. Cardinal positions of gaze and muscles primarily tested in those fields of gaze. Arrow indicates position in which each muscle is tested.
Figure 16–4. Cardinal positions of gaze and muscles primarily tested in those fields of gaze. Arrow indicates position in which each muscle is tested.
Alignment can be assessed in several ways. In order of increasing accuracy, these methods are observation, the corneal light reflex test, and cover testing. Observation is an educated guess about whether the eyes are properly aligned. Corneal light reflex evaluation (Hirschberg test) is performed by shining a light beam at the patient’s eyes, observing the reflections off each cornea, and estimating whether these “reflexes” appear to be positioned properly. If the reflection of light is noted temporally on the cornea, esotropia is suspected (Figure 16–5). Nasal reflection of the light suggests exotropia (outward deviation). Accuracy of these tests increases with increasing angles of misalignment.

 Figure 16–5. Temporal displacement of light reflection showing esotropia (inward deviation) of the right eye. Nasal displacement of the reflection would show exotropia (outward deviation) of the left eye.
Figure 16–5. Temporal displacement of light reflection showing esotropia (inward deviation) of the right eye. Nasal displacement of the reflection would show exotropia (outward deviation) of the left eye.
Another way of evaluating alignment is with the cover test, in which the patient fixes on a target while one eye is covered. If an esotropia or an exotropia is present, the deviated eye will make a corrective movement to fixate on the target when the previously fixating eye is occluded. The other eye is tested similarly. When the occluder is removed from the eye just uncovered, a refixation movement of that eye indicates a phoria, or latent deviation, if alignment is reestablished (Figure 16–6). If the uncovered eye picks up fixation and strabismus is still present, that eye can be presumed to be dominant and the non-preferred eye possibly amblyopic. If the eye remains deviated after the occluder is removed, a tropia is noted to be present. A deviated eye that is blind or has very poor vision will not fixate on a target. Consequently, spurious results to cover testing may occur, which can happen with disinterest on the part of the patient, small-angle strabismus, and inexperience in administering cover tests.
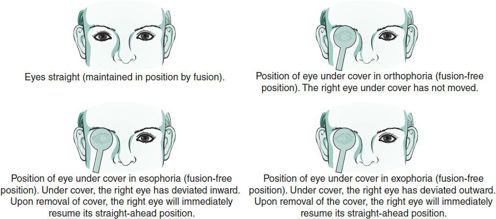
 Figure 16–6. Cover testing. The patient is instructed to look at a target at eye level 20 ft away. Note that in the presence of constant strabismus (ie, a tropia rather than a phoria), the deviation will remain when the cover is removed. (Reprinted, with permission, from Riordan-Eva P, Whitcher J: Vaughan & Asbury’s General Ophthalmology, 17th ed. McGraw-Hill; 2008.)
Figure 16–6. Cover testing. The patient is instructed to look at a target at eye level 20 ft away. Note that in the presence of constant strabismus (ie, a tropia rather than a phoria), the deviation will remain when the cover is removed. (Reprinted, with permission, from Riordan-Eva P, Whitcher J: Vaughan & Asbury’s General Ophthalmology, 17th ed. McGraw-Hill; 2008.)
Red Reflex Test
 Clinical Findings
Clinical Findings
The examiner should see a round, red light in both eyes. The red reflex of each eye can be compared simultaneously when the observer is approximately 4 ft away from the patient. The largest diameter of light is shown through the ophthalmoscope, and no correction (zero setting) is dialed in the ophthalmoscope unless it is to compensate for the examiner’s uncorrected refractive error. A red reflex chart is available through the AAP policy statement on red reflex testing on pediatric patients at http://aappolicy.aappublications.org/.
 Differential Diagnosis
Differential Diagnosis
The red reflex test (Brückner test) is useful for identifying disorders such as media opacities (eg, cataracts), large refractive errors, tumors such as retinoblastoma, and strabismus.
 Treatment
Treatment
A difference in quality of the red reflexes between the two eyes constitutes a positive Brückner test and requires referral to an ophthalmologist.
American Academy of Pediatrics; Section on Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists: Red reflex examination in neonates, infants, and children. Pediatrics 2008;122(6):1401–1404 [PMID: 19047263].
OPHTHALMOSCOPIC EXAMINATION
A handheld direct ophthalmoscope allows visualization of the ocular fundus. As the patient’s pupil becomes more constricted, viewing the fundus becomes more difficult. Although pupillary dilation can precipitate an attack of closed-angle glaucoma in the predisposed adult, children are very rarely predisposed to angle closure. Exceptions include those with a dislocated lens, past surgery, or an eye previously compromised by a retrolental membrane, such as in ROP. Therefore, if an adequate view of the fundus is precluded by a miotic pupil, use of a dilating agent (eg, one drop in each eye of 2.5% phenylephrine or 0.5% or 1% tropicamide) should provide adequate mydriasis (dilation). In infants, one drop of a combination of 1% phenylephrine with 0.2% cyclopentolate (Cyclomydril) is safer. Structures to be observed during ophthalmoscopy include the optic disc, blood vessels, the macular reflex, and retina, as well as the clarity of the vitreous media. By increasing the amount of plus lens dialed into the instrument, the point of focus moves anteriorly from the retina to the lens and finally to the cornea.
OCULAR TRAUMA
OCULAR FOREIGN BODIES
 Prevention
Prevention
Protective goggles or prescription glasses can help prevent ocular injuries and should be encouraged while participating in activities at risk for eye injuries, such as grinding metal, hammering, or sawing wood.
 Clinical Findings
Clinical Findings
Foreign bodies on the globe and palpebral conjunctiva usually cause discomfort and red eye. The history may suggest the origin of the foreign body, such as being around a metal grinder or being outside on a windy day when a sudden foreign body sensation was encountered associated with tearing, redness, and pain. Pain with blinking suggests that the foreign body may be trapped between the eyelid and the eye.
Magnification with a slit lamp may be needed for inspection. Foreign bodies that lodge on the upper palpebral conjunctiva are best viewed by everting the lid on itself and removing the foreign body with a cotton applicator. The conjunctival surface (palpebral conjunctiva) of the lower lid presents no problem with visualization. After simple removal of a foreign body that is thought not to be contaminated, no other treatment is needed if no corneal abrasion has occurred.
 Differential Diagnosis
Differential Diagnosis
Corneal abrasion, corneal ulcer, globe rupture/laceration.
 Complications
Complications
Pain, infection, and potential vision loss from scarring.
 Treatment
Treatment
When foreign bodies are noted on the bulbar conjunctiva or cornea (Figure 16–7), removal is facilitated by using a topical anesthetic. If the foreign body is not too adherent, it can be dislodged with a stream of irrigating solution (Dacriose or saline) or with a cotton applicator after instillation of a topical anesthetic. Otherwise, a foreign body spud or needle is used to undermine the foreign body. This must be done with adequate magnification and illumination. An antibiotic ointment is then instilled. Ferrous corneal bodies often have an associated rust ring, which may be removed under slit-lamp visualization in cooperative children or under anesthesia if necessary.
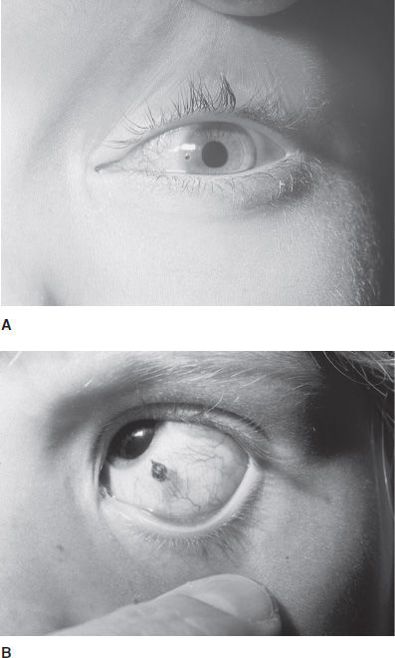
 Figure 16–7. A: Corneal foreign body at the nasal edge of the cornea. B: Subconjunctival foreign body of graphite.
Figure 16–7. A: Corneal foreign body at the nasal edge of the cornea. B: Subconjunctival foreign body of graphite.
 Prognosis
Prognosis
Usually excellent if treatment is obtained shortly after injury.
CORNEAL ABRASION
 Pathogenesis
Pathogenesis
Children often suffer corneal abrasions accidentally while playing with siblings or pets as well as participating in sports. Contact lens users frequently develop abrasions due to poorly fitting lenses, overnight wear, and use of torn or damaged lenses.
 Prevention
Prevention
Proper contact lens care and parental supervision can prevent activities that can lead to a corneal abrasion.
 Clinical Findings
Clinical Findings
Symptom of a corneal abrasion is sudden and severe eye pain, usually after an inciting event such as an accidental finger poke to the eye. Decreased vision secondary to pain and tearing are common complaints. Eyelid edema, tearing, injection of the conjunctiva, and poor cooperation with the ocular examination due to pain are common signs of a corneal abrasion. Fluorescein dye is instilled into the eye and a cobalt blue or Wood lamp is used to illuminate the affected eye. The area with the abrasion will stain bright yellow.
 Differential Diagnosis
Differential Diagnosis
Ocular or adnexal foreign bodies, corneal ulcer, corneal laceration.
 Complications
Complications
Possible vision loss from corneal infection and scarring.
 Treatment
Treatment
Ophthalmic ointment, such as erythromycin ointment, lubricates the surface of the cornea and also helps prevent infections. Patching the affected eye when a large abrasion is present may provide comfort, but it is not advised for corneal abrasions caused by contact lens wear or other potentially contaminated sources. Large corneal abrasions result in referred pain to the ipsilateral brow. If a brow ache is present, it may be treated by the use of a topical cycloplegic agent such as 1% cyclopentolate. Daily follow-up is required until healing is complete.
 Prognosis
Prognosis
Excellent if corneal infection and scarring do not occur.
INTRAOCULAR FOREIGN BODIES & PERFORATING OCULAR INJURIES
 Pathogenesis
Pathogenesis
Intraocular foreign bodies and penetrating injuries are most often caused by being in close proximity to high-velocity projectiles such as windshield glass broken during a motor vehicle accident, metal ground without use of protective safety goggles, and improperly detonated fireworks.
 Prevention
Prevention
Use protective eyewear when engaging in activities at risk for ocular injury.
 Clinical Findings
Clinical Findings
Sudden ocular pain occurs; vision loss, as well as multiple organ trauma, may be present.
Intraocular foreign bodies and corneal and scleral lacerations (ruptured globe) require emergency referral to an ophthalmologist. The diagnosis may be difficult if the obvious signs of corneal perforation (shallow anterior chamber with hyphema, traumatic cataract, and irregular pupil) are not present (Figure 16–8). Furthermore, nonradiopaque materials such as glass will not be seen on x-ray film.

 Figure 16–8. Corneal laceration with irregular pupil and vitreous loss.
Figure 16–8. Corneal laceration with irregular pupil and vitreous loss.
Computed tomographic (CT) scan may be useful in evaluating ocular trauma, including bony injury and intraocular foreign bodies. Magnetic resonance imaging (MRI) must be avoided if a magnetic foreign body is suspected.
 Differential Diagnosis
Differential Diagnosis
Corneal abrasion, superficial foreign body of the eye or eyelids.
 Complications
Complications
Vision loss, intraocular infection, loss of the eye.
 Treatment
Treatment
In cases of suspected intraocular foreign body or perforation of the globe, it may be best to keep the child at rest, gently shield the eye with a metal shield or cut-down paper cup, and keep the extent of examination to a minimum to prevent expulsion of intraocular contents. In this setting, the child should be given nothing by mouth in case eye examination under anesthesia or surgical repair is required.
 Prognosis
Prognosis
Prognosis depends on the extent of the trauma.
BLUNT ORBITAL TRAUMA
 Pathogenesis
Pathogenesis
Trauma to the orbit from a closed fist, collision with another player during team sports, and falls are common causes of blunt orbital injuries. Orbital compartment syndrome, which may result from severe orbital trauma, is caused by hemorrhaging within the orbit or severe orbital edema (or both). This is an emergency which may lead to permanent vision loss if not treated urgently.
 Prevention
Prevention
Protective eyewear during athletic activities and adequate supervision of children at home and school.
 Clinical Findings
Clinical Findings
Blunt trauma to the orbit may result in orbit fractures. The orbital floor is a common location for a fracture (called a blowout fracture). A specific fracture that occurs mainly in children after blunt orbit trauma is called the white-eyed blowout fracture. This results from a greenstick fracture of the orbit with entrapment of extraocular muscles. It is called “white-eyed” because the external orbital soft tissue injury may appear to be minimal, but the patient will have severe pain with eye movement, as well as nausea, vomiting, and restriction of eye movements.
A blowout fracture must be suspected in a patient with symptoms of double vision, pain with eye movements, and restriction of extraocular muscle movements after blunt orbital trauma. CT images of an orbital floor fracture often reveal herniation of orbital fat or the inferior rectus muscle into the maxillary sinus. Assessment of ocular motility, globe integrity, and intraocular pressure will determine the extent of the blunt orbital injury. Consultation with an ophthalmologist is necessary to determine the full spectrum of the injuries.
Orbital compartment syndrome is an emergency requiring immediate treatment. Patients present with severe edema or ecchymosis of the eyelids (which makes it very difficult to open the eyelids), proptosis, and possibly an acute traumatic optic neuropathy, resulting in decreased vision or an afferent pupillary defect. Neuroimaging may reveal a retrobulbar hemorrhage and proptosis.
 Differential Diagnosis
Differential Diagnosis
Orbit fracture with or without muscle entrapment, globe rupture, orbital compartment syndrome, and traumatic or ischemic optic neuropathy.
 Treatment
Treatment
Orbital compartment syndrome requires emergent lateral eyelid canthotomy and cantholysis to decompress the orbit. Treatment should not be delayed in order to image the orbits. Prompt treatment can prevent permanent vision loss.
Patients with clinical signs of muscle entrapment require urgent surgical repair to avoid permanent ischemic injury to the involved extraocular muscle. Large fractures may need repair to prevent enophthalmos, a sunken appearance to the orbit. This can usually be performed on a nonemergent basis.
Cold compresses or ice packs for brief periods (eg, 10 minutes at a time) are recommended in older children in the first 24 hours after injury to reduce hemorrhage and swelling.
 Prognosis
Prognosis
The prognosis depends on the severity of the blunt trauma, associated ocular injuries, and extent of the orbit fractures.
LACERATIONS
 Pathogenesis
Pathogenesis
Lacerations of the eyelids and lacrimal system often result from dog bites, car accidents, falls, and fights.
 Prevention
Prevention
Supervision of children at home and at school.
 Clinical Findings
Clinical Findings
Eyelid lacerations may be partial or full thickness in depth depending on the extent of the injury. Foreign bodies, such as glass or gravel, may be present depending on the mechanism of the injury.
 Differential Diagnosis
Differential Diagnosis
Lacerations involving the eyelid may or may not involve the nasolacrimal duct system or eyelid margin. Globe injury may be associated with eyelid lacerations as well.
 Complications
Complications
Poor surgical repair of lacerations of the eyelid margin can result in eyelid malposition, which causes chronic ocular surface irritation and possible corneal scarring.
 Treatment
Treatment
Except for superficial lacerations away from the globe, repair in children is best performed in the operating room under general anesthesia. Special consideration must be given to lacerations involving the lid margin, significant tissue loss, full-thickness lacerations, lacerations that may involve the levator muscle in the upper lid, and to those that may involve the canaliculus (Figure 16–9). These injuries are best repaired by an ophthalmologist and may require intubation of the nasolacrimal system with silicone tubes.

 Figure 16–9. Laceration involving right lower lid and canaliculus.
Figure 16–9. Laceration involving right lower lid and canaliculus.
 Prognosis
Prognosis
Prognosis depends on severity of the injury, tissue loss, and adequacy of surgical repair.
BURNS
 Pathogenesis
Pathogenesis
Chemical burns with strong acidic and alkaline agents can be blinding and constitute a true ocular emergency. Examples are burns caused by exploding batteries, spilled drain cleaner, and bleach. Eyelid burns can occur in toddlers from contact with a lighted cigarette. The cornea is often involved as well. Curling irons can cause similar burns. Burns of the conjunctiva and cornea may be thermal, radiant, or chemical. Radiant energy causes ultraviolet keratitis. Typical examples are welder’s burn and burns associated with skiing without goggles in bright sunlight.
 Prevention
Prevention
Protective eyewear when engaging in activities that pose a potential risk for exposure to hazardous chemicals, radiant energy, or when explosive conditions are possible.
 Clinical Findings
Clinical Findings
Superficial thermal burns cause pain, tearing, and injection. Corneal epithelial defects can be diagnosed using fluorescein dye, which will stain areas of the cornea bright yellow where the epithelium is absent. The fluorescein dye pattern will show a uniformly stippled appearance of the corneal epithelium in ultraviolet keratitis.
 Differential Diagnosis
Differential Diagnosis
Corneal abrasion, iritis.
 Complications
Complications
Significant corneal injury, especially if associated with an alkali burn, may lead to scarring and vision loss. Eyelid scarring can result in chronic exposure, dry eye, irritation, and entropion or ectropion.
 Treatment
Treatment
Alkalis tend to penetrate deeper than acids into ocular tissue and often causes severe injury. Damage to the conjunctival vessels gives the eye a white or blanched appearance, resulting in ocular ischemia. Immediate treatment consists of copious irrigation and removal of precipitates as soon as possible after the injury. Initial stabilization of the injury is initiated by using topical antibiotics and patching the injured eye closed. A cycloplegic agent such as cyclopentolate 1% may be added if corneal involvement is present. This reduces the pain from ciliary spasm and iritis that may accompany the injury. The patient should be referred to an ophthalmologist after immediate first aid has been given.
 Prognosis
Prognosis
Prognosis depends on the severity of the injury.
HYPHEMA
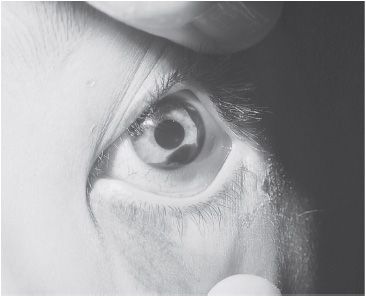
 Figure 16–10. Hyphema filling approximately 20% of the anterior chamber.
Figure 16–10. Hyphema filling approximately 20% of the anterior chamber.
 Pathogenesis
Pathogenesis
Blunt trauma to the globe may cause a hyphema, or bleeding within the anterior chamber, from a ruptured vessel located near the root of the iris or in the anterior chamber angle (Figure 16–10).
 Prevention
Prevention
Protective eyewear and appropriate supervision at home and at school.
 Clinical Findings
Clinical Findings
Blunt trauma severe enough to cause a hyphema may be associated with additional ocular injury, including iritis, lens subluxation, retinal edema or detachment, and glaucoma. In patients with sickle cell anemia or trait, even moderate elevations of intraocular pressure may quickly lead to optic atrophy and permanent vision loss. Therefore, all African Americans whose sickle cell status is unknown should be tested if hyphema is observed. These patients require extra vigilance in diagnosing and treating hyphema.
 Differential Diagnosis
Differential Diagnosis
Nontraumatic causes of hyphema include juvenile xanthogranuloma and blood dyscrasias. Rarely, hyphema is noted in the newborn after a stressful birth.
 Complications
Complications
Increased intraocular pressure, glaucoma, permanent corneal staining, and vision loss.
 Treatment
Treatment
A shield should be placed over the eye, the head elevated, and arrangements made for ophthalmologic referral.
 Prognosis
Prognosis
The prognosis is worse if intraocular pressure is elevated, the patient has sickle cell disease, or if other associated ocular injuries are present.
ABUSIVE HEAD TRAUMA & NONACCIDENTAL TRAUMA
 Pathogenesis
Pathogenesis
The mechanism of injury has been ascribed to a rapid back and forth shaking of young children that results in brain and ocular injuries. It is now believed that injuries may also be the result of blunt impact. Additional injury may result from spinal cord injuries and hypoxia.
 Clinical Findings
Clinical Findings
Victims often have multiple organ system involvement that includes, but is not limited to, traumatic brain injury, bone fractures, and retinal hemorrhages. The presentation can vary from irritability to emesis, change in mental status, or cardiopulmonary arrest.
Neuroimaging of the brain and a skeletal survey are used to diagnose shaken baby syndrome. Ophthalmic consultation and a dilated retinal examination are necessary to document retinal hemorrhages. Hemorrhages may be unilateral or bilateral and may be located in the posterior pole or periphery. Whereas retinal hemorrhages tend to resolve fairly quickly, those in the vitreous do not. If a blood clot lies over the macula, deprivation amblyopia may occur and may require intraocular surgery by a retinal specialist. Other ocular findings associated with nonaccidental trauma include lid ecchymosis, subconjunctival hemorrhage, hyphema, retinal folds, retinoschisis (traumatic separation of the retinal layers), and optic nerve edema. Acute-onset esotropia can also occur.
 Differential Diagnosis
Differential Diagnosis
The differential diagnosis of retinal hemorrhages includes those secondary to a fall, seizures, chest compressions during cardiopulmonary resuscitation, blood dyscrasias, and Terson syndrome, among others. A team effort between the primary treating physician, neurosurgery, orthopedics, ophthalmology, and social services is often needed to determine the true cause of a patient’s injuries.
 Complications
Complications
The severity of injuries dictates the long-term outcome. Severely diffuse retinal hemorrhages, associated traumatic optic neuropathy, and cortical injury adversely affect the potential for normal vision.
 Treatment
Treatment
Management of any systemic injuries is required. Observation by an ophthalmologist for resolution of retinal hemorrhages is the usual management. Vitreous hemorrhages or large preretinal hemorrhages that do not resolve within several weeks may need surgical treatment by a retinal specialist.
 Prognosis
Prognosis
Prognosis depends on the severity of ocular and brain injuries.
Levin AV: Retinal hemorrhage in abusive head trauma. Pediatrics 2010;126(5):961–970 [PMID: 20921069].
PREVENTION OF OCULAR INJURIES
Air rifles, paintballs, and fireworks are responsible for many serious eye injuries in children. Golf injuries can be very severe. Bungee cords have been associated with multiple types of severe ocular trauma, including corneal abrasion, iris tears, hyphema, vitreous hemorrhage, retinal detachment, and blindness. Use of these items and associated activities should be avoided or very closely supervised. Safety goggles should be used in laboratories and industrial arts classes, and when operating snow blowers, power lawn mowers, and power tools, or when using hammers and nails.
Sports-related eye injuries can be prevented with protective eyewear. Sports goggles and visors of polycarbonate plastic will prevent injuries in games using fast projectiles such as tennis or racquet balls, or where opponents may swing elbows or poke at the eye.
The one-eyed individual should be specifically advised to always wear polycarbonate eyeglasses and goggles for all sports. High-risk activities such as boxing and the martial arts should be avoided by one-eyed children.
DISORDERS OF THE OCULAR STRUCTURES
DISEASES OF THE EYELIDS
The eyelids can be affected by various dermatologic and infectious conditions.
Blepharitis
 Pathogenesis
Pathogenesis
Blepharitis is caused by inflammation of the eyelid margin, meibomian gland obstruction, bacterial overgrowth, and tear film imbalance.
 Prevention
Prevention
Eyelid hygiene is essential to prevent or control blepharitis. Eyelid scrubs help decrease the bacterial load on the eyelid margins and lashes. Warm compresses help loosen the secretions of the meibomian glands.
 Clinical Findings
Clinical Findings
Patients may present with dry eye symptoms, red and irritated eyelid margins, conjunctivitis, and decreased vision from corneal erosions or vascularization. When conjunctival injection accompanies blepharitis, the condition is known as blepharoconjunctivitis. Staphylococcus is the most common bacterial cause.
 Differential Diagnosis
Differential Diagnosis
Chalazion, hordeolum, and rosacea blepharitis.
 Complications
Complications
Permanent corneal and eyelid margin scarring in severe cases.
 Treatment
Treatment
Treatment includes lid scrubs with baby shampoo several times a week, warm compresses to the eyelids, and application of a topical antibiotic ointment such as erythromycin or bacitracin at bedtime.
 Prognosis
Prognosis
Generally good.
Chalazion
 Pathogenesis
Pathogenesis
Obstruction of the eyelid margin meibomian glands with resultant inflammation, fibrosis, and granuloma formation.
 Prevention
Prevention
See earlier section Blepharitis.
 Clinical Findings
Clinical Findings
Eyelid nodule of variable size and localized erythema of the corresponding palpebral conjunctiva that may be associated with a yellow lipogranuloma (Figure 16–11).
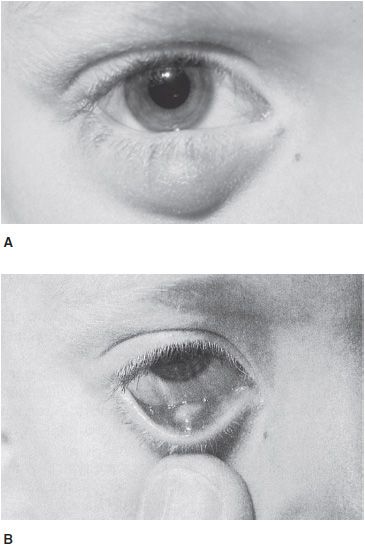
 Figure 16–11. Chalazion. A: Right lower lid, external view. B: Right lower lid conjunctival surface.
Figure 16–11. Chalazion. A: Right lower lid, external view. B: Right lower lid conjunctival surface.
 Differential Diagnosis
Differential Diagnosis
Hordeolum, blepharitis.
 Treatment
Treatment
See earlier section Blepharitis. Oral flax seed oil may also decrease the risk of recurrent chalazion. If incision and curettage are needed because the lesion is slow to resolve, the child will require a general anesthetic. Topical azithromycin (ophthalmic solution 1%) may also help decrease recurrence of chalazion, but it is still under investigation.
 Prognosis
Prognosis
Generally good.
VIRAL EYELID DISEASE
 Pathogenesis
Pathogenesis
Herpes simplex virus (HSV) may involve the conjunctiva and lids at the time of primary herpes simplex infection resulting in blepharoconjunctivitis. Vesicular lesions with an erythematous base occur. Herpes zoster causes vesicular disease in association with a skin eruption in the dermatome of the ophthalmic branch of the trigeminal nerve. Molluscum contagiosum lesions are typically umbilicated papules. If near the lid margin, the lesions may cause conjunctivitis.
 Prevention
Prevention
Avoid contact with individuals with active viral infections.
 Clinical Findings
Clinical Findings
A vesicular rash is the most common sign of herpes viral eyelid infection. Fluorescein dye should be administered topically to the effected eye followed by examination with a cobalt blue light to determine if corneal or conjunctival involvement is present. Herpes simplex or herpes zoster can be diagnosed by rapid viral culture (24–48 hours) or detection of antigen in skin lesions (3 hours).
 Differential Diagnosis
Differential Diagnosis
Impetigo.
 Complications
Complications
Conjunctivitis, keratitis (corneal infection).
 Treatment
Treatment
Primary herpes simplex blepharoconjunctivitis should be treated with systemic acyclovir (a liquid formulation is available), valacyclovir, or famciclovir. When either the conjunctiva or the cornea is involved, treatment should include topical 1% trifluridine or 3% vidarabine.
Treatment of ophthalmic herpes zoster with nucleoside analogues within 5 days after onset may reduce the morbidity. When vesicles are present on the tip of the nose with herpes zoster (Hutchinson sign), ocular involvement, including iritis, is more likely.
Molluscum contagiosum lesions may be treated with cautery or excision.
 Prognosis
Prognosis
Generally good unless corneal involvement is present.
MISCELLANEOUS EYELID INFECTIONS
Pediculosis
Pediculosis of the lids (phthiriasis palpebrarum) is caused by Phthirus pubis. Nits and adult lice can be seen on the eyelashes when viewed with appropriate magnification. Mechanical removal and application to the lid margins of Phospholine iodide or 1% mercuric oxide ointment can be effective. Other bodily areas of involvement must also be treated if involved. Family members and contacts may also be infected (see Chapter 15).
Papillomavirus
Papillomavirus may infect the lid and conjunctiva. Warts may be recurrent, multiple, and difficult to treat. Treatment modalities include cryotherapy, cautery, carbon dioxide laser, and surgery.
Staphylococcal Infection
Localized staphylococcal infections of the glands of Zeis within the lid cause a sty (hordeolum) (Figure 16–12). When the infection coalesces and points internally or externally, it may discharge itself or require incision. The lesion is tender and red. Warm compresses help to shorten the acute process. Some practitioners prescribe a topical antibiotic ointment. Any coexisting blepharitis should be treated.
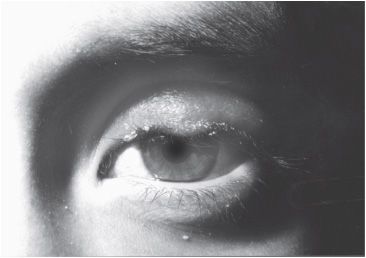
 Figure 16–12. Hordeolum and blepharitis, left upper lid.
Figure 16–12. Hordeolum and blepharitis, left upper lid.
EYELID PTOSIS
 Pathogenesis
Pathogenesis
Ptosis—a droopy upper lid (Figure 16–13)—may be congenital or acquired but is usually congenital in children owing to a defective levator muscle. Other causes of ptosis are myasthenia gravis, lid injuries, third nerve palsy, and Horner syndrome (see next section). Ptosis may be associated with astigmatism and amblyopia.

 Figure 16–13. Congenital ptosis of severe degree, left upper lid.
Figure 16–13. Congenital ptosis of severe degree, left upper lid.
 Prevention
Prevention
Injury prevention.
 Clinical Findings
Clinical Findings
An association sometimes seen with congenital ptosis is the Marcus Gunn jaw-winking phenomenon. Intermittent reduction of the ptosis occurs during mastication or sucking, due to a synkinesis or simultaneous firing of the external or internal pterygoid muscle (innervated by the trigeminal nerve) and the levator muscle (innervated by the oculomotor nerve).
 Differential Diagnosis
Differential Diagnosis
Congenital ptosis, traumatic ptosis, neurogenic ptosis (oculomotor nerve palsy), Horner syndrome.
 Complications
Complications
Deprivation amblyopia and induced astigmatism.
 Treatment
Treatment
Surgical correction is indicated for moderate to severe ptosis. Mild cases less often require operative management. Cosmesis may be better if surgery is delayed until most of the facial growth has occurred, usually around age 5 years.
 Prognosis
Prognosis
The prognosis depends on the presence of amblyopia and whether it is adequately treated.
HORNER SYNDROME
 Pathogenesis
Pathogenesis
The syndrome is caused by an abnormality or lesion to the sympathetic chain. The congenital variety is most commonly the result of birth trauma. Acquired cases may occur in children who have had cardiothoracic surgery, trauma, or brainstem vascular malformation. Most worrisome is a Horner syndrome caused by neuroblastoma of the sympathetic chain in the apical lung region.
 Prevention
Prevention
Sympathetic chain injury avoidance during cardiothoracic surgery and delivery.
 Clinical Findings
Clinical Findings
Parents may notice unequal pupils or different colored eyes. Penlight examination of the eyes may reveal unequal pupils (anisocoria), iris heterochromia, and eyelid ptosis of the affected eye.
The ptosis is usually mild with a well-defined upper lid crease. This differentiates it from congenital ptosis, which typically has a poorly defined lid crease. Another key finding of congenital Horner syndrome is heterochromia of the two irides, with the lighter colored iris occurring on the same side as the lesion (Figure 16–14). Anhidrosis can occur in congenital and acquired cases. Of note, not all of the three signs must be present to make the diagnosis.

 Figure 16–14. Congenital Horner syndrome. Ptosis, miosis, and heterochromia. Lighter colored iris is on the affected left side.
Figure 16–14. Congenital Horner syndrome. Ptosis, miosis, and heterochromia. Lighter colored iris is on the affected left side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree












































