Fig. 1
Diagram of the extensor mechanism (this was taken from Hand Clinics, if Springer has one please substitute)
Wrist extensors include the extensor carpi ulnaris (ECU), the extensor carpi radialis brevis (ECRB), and the extensor carpi radialis longus (ECRL). Each of these extensors originates on the lateral humerus and is responsible for wrist extension and, in the case of the ECU, ulnar deviation. The ECRL and ECRB are innervated by the radial nerve and insert on the index and middle finger metacarpals, respectively. The ECU is innervated by the posterior interosseous nerve (PIN) and inserts on the base of the small finger metacarpal.
Digital extensors include the extensor digitorum communis (EDC), the extensor indicis proprius (EIP), and the extensor digiti minimi (EDQ). The EDC has one common origin on the lateral condyle of the humerus and several slips (index, middle, ring, and small) which insert on the extensor hood of each digit at the metacarpophalangeal (MCP) joint. The EIP originates on the lateral border of the ulna and inserts distally on the extensor hood of the index finger just ulnar to the insertion of the EDC insertion. The EDQ originates on the proximal ulna and inserts on the extensor hood of the small finger just ulnar to the insertion of the EDC. Juncturae tendinum are fibrous connections between the digital extensors at the level of the metacarpals. These interconnections help to evenly distribute forces between the fingers during digital extension. The digital extensors are innervated by the posterior interosseous nerve.
Thumb extensors include the extensor pollicis longus (EPL), the extensor pollicis brevis (EPB), and the abductor pollicis longus (APL). The EPL originates on the interosseous membrane and ulna and inserts on the distal phalanx of the thumb. It extends the thumb at the interphalangeal (IP) and metacarpal-phalangeal (MCP) joints, as well as mildly adducts the thumb. The EPB originates on the radius and interosseous membrane and inserts on the proximal phalanx of the thumb. It extends and abducts the thumb. The APL originates on the ulna and interosseous membrane and inserts on the base of the thumb metacarpal. It abducts the thumb. The thumb extensors are innervated by the posterior interosseous nerve.
Each of the extensor tendons passes beneath the extensor retinaculum at the level of the distal radius and ulna. The extensor retinaculum is a strong fibrous band that acts as the only pulley of the extensor system. The extensor retinaculum is septated into six compartments in which the extensor tendons run (Table 1).
Table 1
Extensor tendon compartments of the wrist
1. Abductor pollicis longus (APL) and extensor pollicis brevis (EPB) |
2. Extensor carpi radialis brevis (ECRB) and extensor carpi radialis longus (ECRL) |
3. Extensor pollicis longus (EPL) |
4. Extensor digitorum communis (EDC) and extensor indicis proprius (EIP) |
5. Extensor digiti minimi (EDQ) |
6. Extensor carpi ulnaris (ECU) |
The digital extensor apparatus is a very intricate and elegant system of interconnecting extensor tendons, interossei, and lumbrical muscles, which allow for the controlled flexion and extension of the digits. The digital extensor tendons insert on the extensor hood at the level of the MCP joint. Transverse fibers form the sagittal bands which stabilize and centralize the extensor tendons over the MCP joint. The volar and dorsal interossei originate on the metacarpal shafts and insert on the dorsal hoods of the extensor mechanism. They are responsible for adduction and abduction of the digits, respectively, as well as flexion of the MCP joint and extension of the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints. The lumbrical muscles insert on the extensor apparatus at the level of the proximal phalanx. They are responsible for MCP joint flexion and PIP joint extension.
Extensor Tendon Injuries
Assessment of Injury
A complete and thorough history and physical examination is an important first step in appropriately managing any upper extremity injury in children. When obtaining a history, it is important to note when the child was injured and what the mechanism of injury was. Was the injury a sharp laceration or was there a crush component? When did the injury occur? Acute injuries may be repaired primarily, whereas subacute or chronic injuries may need to be reconstructed.
Examining an injured child may be quite difficult, especially when the child is younger or badly injured. Toddlers and infants cannot follow directions very well. Given this, the keys to a successful examination are passive tests and observations. Once the history has been obtained, the examination begins with the inspection of the limb. A lot of information can be obtained by simply observing the child interacting with the family. The skin should be inspected for any lacerations or compromise. A normal digital resting cascade should be observed. Where possible, active and passive extension of each digit should be tested at each joint (DIP, PIP, and MCP).
Disruption of the insertion of the extensor mechanism about the distal phalanx is a mallet finger. Mallet fingers will present with a flexion deformity of the DIP joint and weakness of active DIP extension. Injuries to the central slip insertion on the middle phalanx may present with normal, but painful, extension at the PIP joint. Elson’s test should be considered when a central slip injury is suspected (Elson 1986). Elson’s test places the PIP joint in a 90° of flexion, and the patient is asked to extend the finger against resistance. A positive test, for central slip disruption, causes the DIP joint to go into rigid extension when the PIP is extended (owing to the pull of the lateral bands on the distal terminal tendon). Sagittal bands should be examined for subluxation. The MCP joint should be actively extended and flexed. Difficulty with active extension associated with a clunk or snapping sensation over the hood of the MCP joint should be suspicious for sagittal band disruption. Radial-sided injury of the long finger is the most commonly observed location for this injury.
Extensor tendon injuries may be classified based on their temporal relationship (acute versus chronic), integrity of the soft tissue (open versus closed), or anatomic location. Seven anatomic zones have been described and are listed in Table 2.
Table 2
Zones of extensor tendon injury
Zone I | Disruption of the distal insertion (mallet finger) |
Zone II | Disruption of the tendon over the middle phalanx |
Zone III | Disruption over the PIP joint (central slip/Boutonnière injury) |
Zone IV | Disruption over the proximal phalanx |
Zone V | Disruption over the MCP joint |
Zone VI | Disruption over the metacarpal |
Zone VII | Disruption over the wrist |
Zone VIII | Disruption over the distal forearm |
Zone IX | Disruption at the muscle tendon junction |
Imaging
Radiographs
Standard radiographs of the hand (three views (AP/Lat/Oblique)) are useful in evaluating the hand for bony injuries, as in the case of the bony mallet finger.
Ultrasound
Ultrasound (U/S) can be useful to assess discontinuity of a tendon in a child whose examination is questionable. Ultrasound is a real-time study, where the examination is performed while the child is awake. There is no need for sedation and the examination is performed in real time which allows tendon movement to be visualized.
Magnetic Resonance Imaging
The use of magnetic resonance imaging (MRI) allows for the visualization of tendon injury in several different planes (sagittal, coronal, and axial). MRI like ultrasound is useful in assessing tendon injury when the examination is questionable. It can help determine the degree of retraction of a tendon, but unlike ultrasound younger children will need sedation for completion of the study.
Treatment
The treatment for extensor tendon injuries varies depending on several factors including the mechanism of injury, age of the child, and temporal relationship of the injury to treatment. A general rule of thumb is that “open injuries” are treated with open surgery and “closed injuries” are treated closed with immobilization or splinting.
Nonoperative Treatment
Nonoperative management of extensor tendon injuries in children is reserved for closed injuries and for children who are old enough to comply with the treatment protocols. In cases where splinting may be appropriate in an older child, a younger child may not be compliant enough and operative intervention may be necessary.
Mallet Finger
Mallet finger is the disruption of the distal terminal extensor tendon where it inserts on the distal phalanx. These are typically closed injuries, most often sustained via an axial load to the tip of the finger, forcibly flexing the distal phalanx disrupting the distal terminal extensor tendon. Mallet fingers may injure the soft tissue only or involve a portion of the distal phalanx (bony mallet finger). In younger children injuries to the distal phalanx are frequently open injuries resulting from crushing mechanisms such as getting a finger closed in a door. These crush injuries may or may not involve the extensor mechanism but careful consideration should be made.
Treatment of closed soft tissue mallet fingers consists of static extension splinting of the DIP joint. The DIP extension splint is applied to the DIP joint with the PIP joint left free (Bendre et al. 2005). The splint is worn continuously 24 h a day for 6 weeks. The finger is then reexamined for an extensor lag. If no lag is present, the splint is worn for 2 more weeks only at night. If no lag persists after a total of 8 weeks of treatment, splinting is discontinued. If a lag is present after 8 weeks, then splinting may be continued for 4–6 more weeks (Fig. 2).
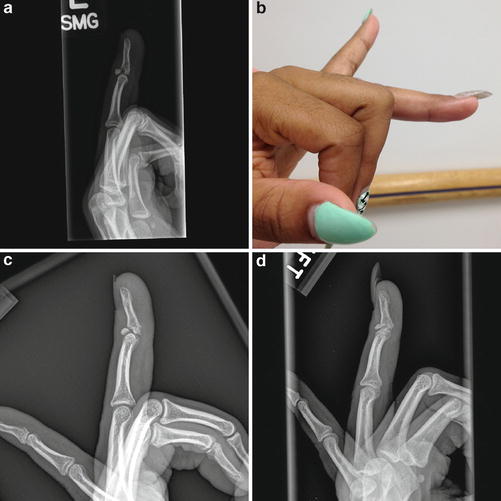
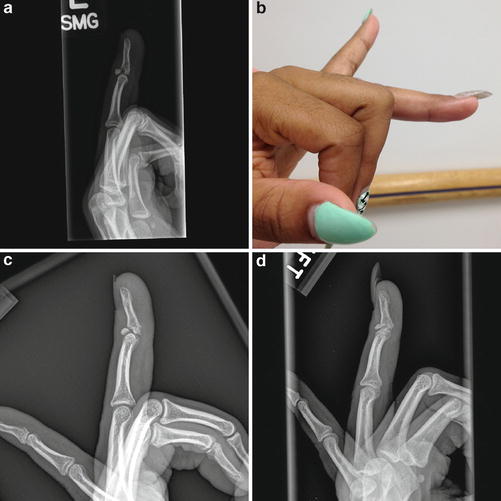
Fig. 2
(a) Injury radiograph of bony mallet, (b) clinical photo of mallet finger after 6 weeks of static extension splinting, (c) radiograph of healing of bony mallet finger 6 weeks, (d) radiograph of healing mallet finger 12 weeks
Failure to treat a mallet finger injury may result in a swan neck deformity of the finger. Incompetence of the distal insertion of the extensor tendon causes a greater force transmission to the insertion of the tendon along the central slip. This overpull causes hyperextension of the PIP joint and coupled with the flexion deformity of the DIP joint results in the swan neck deformity.
Central Slip Injury
Injuries to the PIP joint arising from blunt trauma may cause rupture of the central slip insertion on the dorsal lip of the middle phalanx. The injury may be underwhelming at first, often confused as a sprain of the PIP joint. Loss of, or painful, extension at the PIP joint should raise concern for this injury. Elson’s test should be used to test the competence of the central slip insertion. If the central slip is disrupted, the PIP joint should be immobilized in extension for 6 weeks. The DIP and MP joints should be left free, and active motion about these joints should be encouraged to prevent shortening of the oblique retinacular ligament and volar migration of the lateral bands. At 6 weeks the splint is removed and AROM of the PIP joint is initiated. The patient is followed until full range of motion of the digit is obtained.
Failure to recognize and treat the acute central slip injury may lead to the development of a chronic boutonniere deformity. This is characterized by a flexion posture of the PIP joint and hyperextension posture of the DIP joint. Similar to the case of an untreated mallet finger leading to a swan neck deformity, the imbalance of force transmission along the injured extensor mechanism causes the deformity to progress. The overpull along the terminal tendon insertion causes hyperextension of the DIP joint and lateral band volar migration causes a progressive PIP flexion deformity.
Operative Treatment
Once the decision to bring a patient to the operating room has been made, many variations in anesthesia may be considered. The choice of anesthesia depends on many factors including patient age, medical comorbidities, and anesthesia availability. More often, in younger children, general anesthesia is preferred. For older children regional anesthesia with sedation may be considered.
The patient is positioned supine on the operating room (OR) table and is pulled over to the side of the affected limb. A radiolucent hand table is placed, with the midportion at the level of the axilla. A padded tourniquet is applied to the upper limb, and the table is turned 90° to place the hand in the center of the operating room.
A variety of instruments can be used to help with the surgical treatment of tendon injuries in children. A basic hand tray should consist of small tenotomy scissors, retractors, and self-retainers. This basic set can be supplemented with tools specifically designed to aid in tendon retrieval and repair. A malleable hand, tendon retriever, and a pediatric feeding tube are tools that are useful in tendon repair for both flexor tendons and extensor tendons.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


