EBV was the first human virus to be associated with malignancy. EBV infection may result in a spectrum of proliferative disorders ranging from self-limited, usually benign disease such as infectious mononucleosis to aggressive, nonmalignant proliferations such as the virus-associated hemophagocytic syndrome to lymphoid and epithelial cell malignancies. Benign EBV-associated proliferations include oral hairy leukoplakia, primarily in adults with AIDS, and lymphoid interstitial pneumonitis, primarily in children with AIDS. Malignant EBV-associated proliferations include nasopharyngeal carcinoma, Burkitt lymphoma, Hodgkin disease, lymphoproliferative disorders, and leiomyosarcoma in immunodeficient states, including AIDS. There is no firm evidence of development of EBV quasispecies that would contribute to the pathogenesis of EBV-positive malignancies.
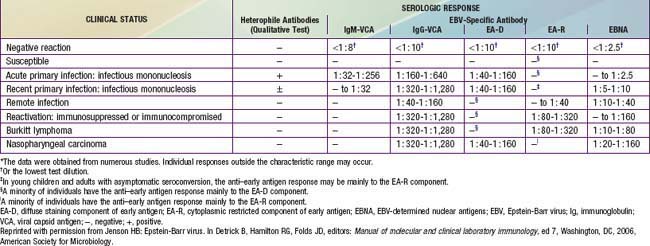
Nasopharyngeal carcinoma occurs worldwide but is 10 times more common in persons in southern China, where it is the most common malignant tumor among adult men. It is also common among whites in North Africa and Inuit in North America. Patients usually present with cervical lymphadenopathy, eustachian tube blockage, and nasal obstruction with epistaxis. All malignant cells of undifferentiated nasopharyngeal carcinoma contain a high copy number of EBV episomes. Persons with undifferentiated and partially differentiated, nonkeratinizing nasopharyngeal carcinomas have elevated EBV antibody titers that are both diagnostic and prognostic. High levels of immunoglobulin A (IgA) antibody to EA and VCA may be detected in asymptomatic individuals and can be used to follow response to tumor therapy (Table 246-1). Cells of well-differentiated, keratinizing nasopharyngeal carcinoma contain a low number of or no EBV genomes; people with this disease have EBV serologic patterns similar to those of the general population.
CT and MRI are helpful in both identifying and defining masses in the head and neck. The diagnosis is established by biopsy of the mass or of a suspicious cervical lymph node. Surgery is important for staging and diagnosis. Radiation therapy is effective for control of the primary tumor and regional nodal metastases. Chemotherapy with 5-fluorouracil, cisplatin, and methotrexate is effective but not always curative. The prognosis is good if the tumor is localized.
Endemic (African) Burkitt lymphoma, often found in the jaw, is the most common childhood cancer in equatorial East Africa and New Guinea (Chapter 490.2). The median age at onset is 5 yr. These regions are holoendemic for Plasmodium falciparum malaria and have a high rate of EBV infection early in life. The constant malarial exposure acts as a B-lymphocyte mitogen that contributes to the polyclonal B-lymphocyte proliferation with EBV infection, impairs T-lymphocyte surveillance of EBV-infected B lymphocytes, and increases the risk for development of Burkitt lymphoma. Approximately 98% of cases of endemic Burkitt lymphoma contain the EBV genome, compared with only 20% of cases of nonendemic (sporadic or American) Burkitt lymphoma. Individuals with Burkitt lymphoma have unusually and characteristically high levels of antibody to VCA and EA that correlate with the risk for developing tumor (see Table 246-1).
All cases of Burkitt lymphoma, including those that are EBV negative, are monoclonal and demonstrate chromosomal translocation of the c-myc proto-oncogene to the constant region of the immunoglobulin heavy-chain locus, t(8;14), to the κ constant light-chain locus, t(2;8), or to the λ constant light-chain locus, t(8;22). This translocation results in the deregulation and constitutive transcription of the c-myc gene with overproduction of a normal c-myc product that autosuppresses c-myc production on the untranslocated chromosome.
The incidence of Hodgkin disease peaks in childhood in developing countries and in young adulthood in developed countries. Levels of EBV antibodies are consistently elevated preceding development of Hodgkin disease; only a small minority of patients with the disease is seronegative for EBV. Infection with EBV appears to increase the risk for Hodgkin disease by a factor of 2-4. EBV is associated with more than 50% of cases of mixed cellularity Hodgkin disease and approximately 25% of cases of the nodular sclerosing subtype and is rarely associated with lymphocyte-predominant Hodgkin disease. Immunohistochemical studies have localized EBV to the Reed-Sternberg cells and their variants, the pathognomonic malignant cells of Hodgkin disease.
Only gold members can continue reading.
Log In or
Register to continue
Related