(a) The superficial muscles of the perineum; namely, the superficial transverse perineal muscle, the bulbospongiosus and the ischiocavernosus form a triangle on either side of the perineum. (b) The left bulbospongiosus muscle has been removed to demonstrate the vestibular bulb.
Anal Triangle
The anal triangle includes the anal canal, the anal sphincters and ischioanal fossae. The anal canal is approximately 3.5 cm long and is attached posteriorly to the coccyx by the anococcygeal ligament, a midline fibromuscular structure which runs between the posterior aspect of the EAS and the coccyx. The anus is surrounded laterally and posteriorly by loose adipose tissue within the ischioanal fossae. The pudendal nerves pass over the ischial spines and can be accessed digitally at this site for measurement of pudendal nerve terminal motor latency using a modified electrode. The perineum can also be anaesthetized by injection of local anaesthetic into the pudendal nerve at this site. Anteriorly, the perineal body separates the anal canal from the vagina. The anal canal is surrounded by an inner epithelial lining, a vascular subepithelium and the anal sphincter complex. The lining of the anal canal varies along its length due to its embryologic derivation. The proximal anal canal is lined with rectal mucosa (columnar epithelium) and is separated by the dentate line from the distal anoderm, which consists of modified squamous epithelium. Since the epithelium in the lower canal is well supplied with sensory nerve endings, acute distension or invasive treatment of haemorrhoids in this area causes profuse discomfort, whereas treatment can be carried out with relatively few symptoms in the upper canal lined by insensate columnar epithelium. The anal sphincter complex consists of the external anal sphincter (EAS) and internal anal sphincter (IAS) separated by the conjoint longitudinal coat (Figure 18.2). The striated EAS is subdivided into subcutaneous, superficial and deep, and is responsible for voluntary squeeze and reflex contraction pressure. It is innervated by the pudendal nerve, which is a mixed sensory and motor nerve. However, these subdivisions are not easily demonstrable during anatomical dissection or surgery, but may be of relevance during imaging. To the naked eye, the EAS appears like red meat. The IAS, which is a thickened continuation of the circular smooth muscle of the bowel, contributes about 70% of the resting pressure and is under autonomic control. In contrast to the EAS, the IAS has a pale appearance to the naked eye. As shown in Figure 18.2, the subcutaneous EAS lies at a lower level than the IAS, but during regional or general anaesthesia the paralysed EAS lies at almost the same level as the IAS. The conjoint longitudinal coat lies between the EAS and IAS and consists of a fibromuscular layer, longitudinal muscle and intersphincteric space with its connective tissue elements. Traced downwards, it separates opposite the lower border of the IAS, and the fibrous septae fan out to pass through the EAS and ultimately attach to the skin of the lower anal canal and perianal region. As a result of tonic circumferential contraction of the sphincter, the skin is arranged in radiating folds around the anus, and this is called the anal margin. These folds appear to be flat or ironed out when there is underlying sphincter damage [10].
Classification of perineal trauma depicted in a schematic representation of the anal sphincters.
Perineal Body
The perineal body is the central point of the perineum and is situated between the urogenital and the anal triangles of the perineum. Its three-dimensional form has been likened to that of the cone of the red pine, with each ‘petal’ representing an interlocking structure, such as an insertion site of fascia or a muscle of the perineum. Within the perineal body there is interlacing of muscle fibres from the bulbospongiosus, superficial transverse perineal and EAS muscles. Above this level, there is a contribution from the longitudinal rectal muscle and the medial fibres of the puborectalis muscle.
Levator Ani
The pelvic floor (pelvic diaphragm) is a musculotendineous sheet that spans the pelvic outlet and consists mainly of the symmetrically paired levator ani. The levator ani is a broad muscular sheet of variable thickness attached to the internal surface of the true pelvis and is subdivided into parts according to their attachments and pelvic viscera to which they are related, namely iliococcygeus, puborectalis and pubovisceralis. The pubovisceralis is subdivided into separate parts according to the pelvic viscera to which they relate (i.e. puboanalis, pubovaginalis, pubourethralis and puboperinealis). The levator ani is innervated largely by direct nerves from the pelvic plexus, while the muscles of the perineum are innervated by the pudendal nerve.
Classification
Perineal trauma may occur spontaneously during vaginal birth, or intentionally when a surgical incision (episiotomy) is made to facilitate delivery. It is also possible to have both an episiotomy and a spontaneous tear either as an extension of the episiotomy or as a separate tear. Anterior perineal trauma is defined as injury to the labia, anterior vagina, urethra or clitoris. Posterior perineal trauma is defined as any injury to the posterior vaginal wall, perineal muscles or anal sphincters, and may include disruption of the anal sphincter.
In order to standardize the classification of perineal trauma (Figure 18.2), Sultan proposed the following classification that has been adopted by the Royal College of Obstetricians and Gynaecologists and also recommended by the International Consultation on Incontinence [7,11]:
First degree: laceration of the vaginal epithelium or perineal skin only.
Second degree: involvement of the perineal muscles (bulbocavernosus, transverse perineal), but not the anal sphincter. If the trauma is very deep, the pubococcygeus muscle may be disrupted.
Third degree: disruption of the anal sphincter muscles, which should be further subdivided into:
3a: <50% thickness of external sphincter torn;
3b: >50% thickness of external sphincter torn;
3c: internal sphincter also torn.
Fourth degree: a third-degree tear with disruption of the anal epithelium as well.
If there is any doubt about the grade of a third-degree tear involving the external sphincter, it is advisable to classify it to the higher degree to avoid underestimation [6]. Isolated tears of the anal epithelium (buttonhole) without involvement of the anal sphincters are rare. In order to avoid confusion, they are not included in the above classification but are referred to as such.
Episiotomy
An episiotomy is a surgical incision made with scissors or a scalpel into the perineum in order to increase the diameter of the vulval outlet and facilitate delivery. There are two main types of episiotomy incisions: midline and mediolateral. A midline episiotomy is an incision from the mid-point of the posterior fourchette directed vertically towards the anus, while with a mediolateral episiotomy the incision is directed 40–60 degrees away from the midline. It is claimed that the midline incision is easier to repair and that it is associated with less blood loss, better healing, less pain and earlier resumption of sexual intercourse. However, there is no reliable evidence to support these claims. Limited evidence from one quasi-randomized trial suggested that the midline incision may increase the risk of third- and fourth-degree tears compared with the mediolateral incision. However, these data should be interpreted with caution, as there may be an increased risk of selection bias due to quasi-random treatment allocation, and also analysis was not by intention to treat [12].
There is evidence accumulating that episiotomies angled too close to the midline are at a higher risk of causing OASIS [13,14,15]. This risk reduces by 50% for every six degrees the episiotomy is angled away from the midline [14]. However, if the episiotomy angle becomes nearly horizontal (90°), the pressure on the perineum is not relieved and OASIS incidence increases nine-fold [15]. The current recommendation is to cut an episiotomy at 45–60° from the midline originating from the vaginal fourchette [16]. It is important to note that the angle of a mediolateral episiotomy will reduce significantly after the baby is born, i.e. a 40° episiotomy incision results in a suture angle of 22° from the midline [17]. If an episiotomy is performed at a 60° angle when the perineum is distended, this will result in a suture angle of 45°, which is associated with a lower incidence of anal sphincter tears, anal incontinence and perineal pain [18].
Indications for Episiotomy
Episiotomy is still performed routinely in many parts of the world in the belief that it protects the pelvic floor. However, evidence from randomized controlled trials (RCTs) suggests that routine episiotomy does not prevent severe posterior perineal tears. Carroli and Belizan have conducted the most recent systematic review of randomized clinical trials using the Cochrane Collaboration methodology to determine the possible benefits and risks of restrictive episiotomy versus routine episiotomy. This revealed that compared with routine use, restrictive use of episiotomy resulted in less severe perineal trauma, less suturing and fewer healing complications. There were no significant differences in severe vaginal/perineal trauma, dyspareunia, urinary incontinence or severe pain measures. The only disadvantage shown in restrictive use of episiotomy was an increased risk of anterior perineal trauma. The systematic review concluded that there is evidence to support the restrictive use of episiotomy compared to routine episiotomy (irrespective of the type of episiotomy performed) [12].
There is currently an absence of clear, evidence-based clinical indications for the use of episiotomy. However, it is reasonable to suggest that an episiotomy should be performed to accelerate vaginal delivery in cases of fetal distress, to facilitate manoeuvres during shoulder dystocia, to minimize severe perineal trauma during a forceps delivery, to reduce the occurrence of multiple lacerations in the presence of a thick or rigid perineum, and in situations where prolonged ‘bearing down’ may be harmful for the mother (e.g. severe hypertensive or cardiac disease).
Diagnosis of Perineal Trauma
1. Before assessment for genital trauma, the healthcare professional should [16]:
explain to the woman what they plan to do and why;
offer inhalational analgesia or ensure that epidural analgesia is effective;
ensure good lighting; and
position the woman so that she is comfortable and the genital structures can be seen clearly, and if this is not possible then the woman should be placed in lithotomy.
2. Informed consent should be obtained for a vaginal and rectal examination.
3. If the examination is restricted because of pain, adequate analgesia must be given prior to examination.
4. Following a visual examination of the genitalia, the labia should be parted and a vaginal examination should be performed to establish the full extent of the vaginal tear. When multiple or deep tears are present it is best to examine and repair in lithotomy. The apex of the vaginal laceration should always be identified.
5. A rectal examination should then be performed to exclude OASIS. Figure 18.3 shows a partial tear along the EAS which would have been missed if a rectal examination was not performed. The vagina should be exposed by parting the labia with the index and middle fingers of the other hand. Every woman should have a rectal examination prior to suturing in order to avoid missing isolated tears such as ‘buttonhole’ of the rectal mucosa [6]. Furthermore, a third- or fourth-degree tear may be present beneath apparently ‘intact’ perineal skin, highlighting the need to perform a rectal examination in order to exclude OASIS following every vaginal delivery [6]. Following diagnosis of the tear, it should be graded according to the recommended classification [6].
6. In order to diagnose OASIS, clear visualization is necessary, and the injury should be confirmed by palpation. By inserting the index finger in the anal canal and the thumb in the vagina, the anal sphincter can be palpated by performing a pill-rolling motion. If there is still uncertainty, the woman should be asked to contract her anal sphincter and if the anal sphincter is disrupted, there will be a distinct gap felt anteriorly. If the perineal skin is intact there will be an absence of puckering on the perianal skin anteriorly. This may not be evident under regional or general anaesthesia. As the EAS is in a state of tonic contraction, disruption results in retraction of the sphincter ends [6].
7. The IAS is a circular smooth muscle that appears paler (similar to raw fish) than the striated EAS (similar to raw red meat). If the IAS or anal epithelium is torn, the EAS will invariably be torn.
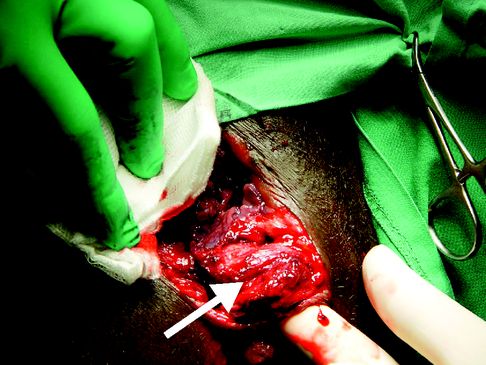
A partial tear (arrow) along the length of the external anal sphincter.
Management and Repair of Perineal Trauma
Basic principles prior to repairing perineal trauma include [6–8] the following:
The skills and knowledge of the operator are important factors in achieving a successful repair. The woman should be referred to a more experienced healthcare professional if uncertainty exists as to the nature or extent of trauma sustained [16].
Repair of the perineum should be undertaken as soon as possible to minimize the risk of bleeding and oedematous swelling of the perineum, as this makes it more difficult to recognize tissue structures and planes when the repair eventually takes place.
Perineal trauma should be repaired using aseptic techniques.
Equipment should be checked and swabs and needles counted before and after the procedure.
Good lighting is essential to visualize and identify the structures involved.
A repair undertaken on an uncooperative patient, due to pain, is likely to result in a poor repair. Ensure that the wound is adequately anaesthetized prior to commencing the repair. It is recommended that 20 ml of lidocaine 1% is injected evenly into the perineal wound. If the woman has an epidural it may be ‘topped-up’ and used to block perineal pain during suturing instead of injecting local anaesthetic [16]. Repair of obstetric anal sphincter trauma should be undertaken in theatre, under general or regional anaesthesia. In addition to providing pain relief, this provides the added advantage of relaxing the muscles, enabling the operator to retrieve the ends of the torn sphincter while performing an overlap repair [8].
First-Degree Tears and Labial Lacerations
Women should be advised that in the case of first-degree trauma, the wound should be sutured in order to improve healing, unless the skin edges are well opposed [16]. If the tear is left unsutured, the midwife or doctor must discuss the implications with the woman and obtain her informed consent. Details regarding the discussion and consent must be fully documented in the woman’s case notes.
Labial lacerations are usually very superficial but may be very painful. Some practitioners do not recommend suturing, but if the trauma is bilateral the lacerations can sometimes adhere together over the urethra and the woman may present with voiding difficulties. It is important to advise the woman to part the labia daily during bathing to prevent adhesions from occurring.
Episiotomy and Second-Degree Tears
Women should be advised that in the case of second-degree trauma, the muscle should be sutured in order to improve healing [16]. A recent Cochrane systematic review [9] of 16 studies involving 8184 women showed that continuous suture techniques compared with interrupted sutures for perineal closure (all layers or perineal skin only) was associated with less pain up to ten days postpartum. Furthermore, there was a greater reduction in pain when the continuous suturing technique was used for all layers. There was an overall reduction in analgesia use associated with the continuous subcutaneous technique versus interrupted stitches for repair of perineal skin. Subgroup analysis showed some evidence of reduction in dyspareunia experienced by participants in the groups that had continuous suturing of all layers. There was also a reduction in suture removal in the continuous suturing groups versus those with interrupted sutures, but no significant differences were seen in the need for re-suturing of wounds or long-term pain. The authors concluded that compared to interrupted methods, the continuous suturing technique for perineal closure, is associated with less short-term pain.
Apart from the technique, suture material used to repair perineal trauma needs to be taken into consideration. A Cochrane systematic review of 18 randomized controlled trials [19] involving 10 171 women was carried out to assess the effects of different suture materials on short- and long-term morbidity following perineal repair. The pooled results from nine of the included studies showed that absorbable synthetic material (polyglycolic acid and polyglactin 910) when compared with catgut suture material was associated with less pain up to three days after delivery and required less analgesia up to ten days postpartum. Compared with synthetic sutures, more women with catgut sutures required re-suturing. Furthermore, more women with standard synthetic sutures required the removal of unabsorbed suture material compared to the rapidly absorbing synthetic sutures. Currently, the use of catgut has been largely superseded in developed countries by absorbable suture material.
The following steps should be adopted [20] (Figure 18.4).
1. Suturing the vagina. The first stitch is inserted above the apex of the vaginal trauma to secure any bleeding points that might not be visible. Close the vaginal trauma with a loose, continuous, non-locking technique, making sure that each stitch is inserted not too wide otherwise the vagina may be narrowed. Continue to suture down to the hymenal remnants and insert the needle through the skin at the fourchette to emerge in the centre of the perineal wound.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


