Emergency Department
Emily F. Gregory
Efren Gutierrez
Paritosh Prasad
Linda T. Wang
Rapid Evaluation and Management of Common Pediatric Emergencies
(For more information, see specific sections in other chapters.)
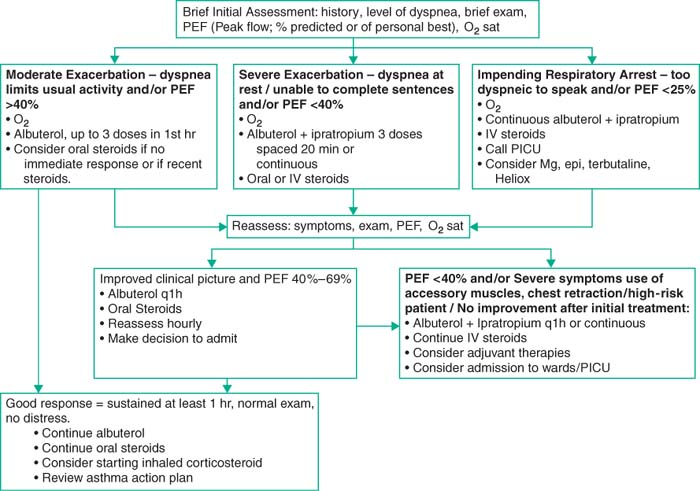
Asthma
(guidelines at http://www.nhlbi.nih.gov.easyaccess1.lib.cuhk.edu.hk/guidelines/asthma/index.htm.)
Management based on FEV1 or peak flow (FEV1 not practical for most settings)
In practice, anyone w/asthma exacerb gets 3 stacked inhaled doses of albuterol and ipratropium.
Evidence shows equiv of nebs and MDI w/ spacer (Pediatr Emerg Care 1996;12:263; J Pediatr 2004;145:172), but in practice most ERs administer via neb. Monitor to keep HR <200
Prednisone/Prednisolone IV/PO 1–2 mg/kg. Equivalence of 1 mg/kg and 2 mg/kg shown in out-patients (Chest 2002;122:624.)
May not apply to patients sick enough for admit; IV preferred if severely ill, unable to PO
Max dosing is 60 mg PO/IV
O2 to keep SpO2 >90%; further treatment based on response to initial management.
Risk factors for asthma-related death: ICU admit, intubation, 2 hospitalizations or 3 ER visits in past yr, low SES, inner city, high routine use albuterol, illicit drug use, psych dz.
Management (EPR3: Guidelines for Diagnosis and Management of Asthma, NIH 2007)
 |
Supraventricular Tachycardia
(Pediatric Advanced Life Support, 2006; Pediatr Emerg Care 2007;23:176)
(See PICU and Cardiology chapters for further management)
Suspected when HR >180 in children, >220 in infants
Incidence of 1–4 per 1000.
Distinguishing SVT from sinus tachycardia:
| ST | SVT | |
|---|---|---|
| HR | Infants <220 Children <180 | Infants >220 Children >180 |
| Beat-to-beat interval | Variable | Fixed |
| P waves | Visible, normal axis | Abnormal axis Often hidden in QRS/ST |
| Onset | Gradual | Abrupt |
| Response to vagal maneuvers | Gradual slowing, then returns | Abrupt termination |
| Response to cardioversion | None | Abrupt conversion |
| Fever | Strongly associated | 2%–3% of patients have fever |
Management (continuous EKG monitoring recommended)
Immediate assessment of hemodynamic status and obtain an EKG
Obtain large bore IV access as close to central circulation as possible
Unstable (i.e., poor perfusion, low BP, respiratory distress, ΔMS)
Synchronized cardioversion: 0.5–1 J/kg in synchronized mode (if narrow complex).
If ineffective, can ↑ to 2 J/kg. Consider sedation and analgesia whenever possible.
Can attempt vagal maneuvers or adenosine while preparing for cardioversion.
Stable (i.e., nl cap refill, BP, mental status, and no evidence of respiratory distress/CHF)
Attempt vagal maneuvers
Infants: Ice water on forehead, eyes, nose for 10–15 sec (33%–62% effective)
Children: Valsalva for 15 sec while supine (blow into occluded straw; thumb)
– OR –
Adenosine 0.1 mg/kg IV (max 6 mg initial dose) infused as fast as possible at site closest to central circ, followed by flush (72%–77% effective).
If ineffective ↑ to 0.2 mg/kg then 0.3 q1–2 min until effect or max dose (12 mg)
If administered in central line, use ½ dose.
Shock/Hypotension
(Pediatric Advanced Life Support. 2006.)
(See PICU chapter for further management)
Shock is state w/ inadeq delivery of O2 and nutrients to meet demand
Final common pathway of multiple disease processes (sepsis, anaphylaxis, dehydration, etc.)
HoTN variably defined, depends on age, best assessed by end organ fxn and profusion (mental status, UOP, capillary refill) (Pediatric Emergency Medicine 2nd Ed. McGraw-Hill 2002:60)
Preterm babies on DOL # 1, MAP should be equal to gestational age
Lower limit SBP in full-term babies: at 1–2 kg 50 mm Hg, at 3–10 kg 60 mm Hg
Lower limit SBP in infant/child ≥10 kg 70 mm Hg (+ 2× age in yr, when age ≤10)
Clinical manifestations: Hx volume loss (vomiting, diarrhea, polyuria, or trauma w/ blood loss), febrile illness (sepsis), exposure to known antigen (allergy), spinal trauma.
Exam w/ early ↑HR and often ↑RR (metabolic acidosis compensation), SBP may be preserved 2/2 significant peripheral vasoconstriction (w/ cap refill >2 sec). Later w/ obtundation and poor periph pulses.
Tachycardia is often the earliest most sensitive sign of early shock but nonspecific
Hypotension itself is often a late and ominous finding
Determine cause: Start initial management, but etiology can define specific treatments
| Specific HX and Exam | Cardiac Output | Peripheral (systemic) Vasoconstriction | Management | |
|---|---|---|---|---|
| Hypovolemic | Volume loss (diarrhea, vomiting, polyuria, blood loss) | ↓ | Increased | Volume replacement (NS bolus 20 cc/kg × 3, then RBC transfusion) |
| Septic – Early – Late | Fever, infectious source (indwelling lines, PNA, etc.) | ↑ ↓ | ↓ (warm) ↑ (cold) | Initially w/ volume, then Abx and pressors (see PICU chapter) |
| Cardiogenic | Hx of congenital heart dz, sweats w/ feeds, etc. | ↓ | ↑ | Eval for pulm edema; if none rx w/ volume; cards consult |
| Distributive | Spinal cord trauma Allergic exposure (w/ assoc rash, etc.) Toxin (drug) related | ↑ | ↓ | Initially w/ volume – Epinephrine w/ anaphylaxis – Pressors for neurogenic shock |
Also consider Obstructive Shock 2/2 Tamponade, massive PE, Tension PTX; if present treat underlying etiology.
Diagnostic studies: Consider stat CBC, glucose, K, Ca, lactate, ABG, and mixed venous sat.
Management: Obtain large bore IV access and give NS 20 cc/kg bolus, repeat up to 3×, then consider blood products. If unable to obtain IV access, obtain IO access.
Patient may need ventilatory support to ensure adequate oxygenation
Pressors: Usually w/ IV dopamine 2–20 mcg/kg/m (can use peripherally) (see PICU chapter)
Ensure pt is euvolemic before initiation of pressors
In pts who are volume and pressor unresponsive, consider IV stress dose steroids
In pts w/ evidence of anaphylaxis (urticarial rash, airway involv) use epinephrine
Central access is required for the use of most pressors.
Seizures
(Emerg Med Clin North Am 2007;25:1061)
Can be prolonged and life threatening or short and self-limited.
Followed by postictal period (lethargy, confusion, irritability); duration related to length of seizure.
Status epilepticus: continuous seizure >30 min or 2+ seizures w/o return to baseline
Partial szr arises in 1 hemisphere, is focal, and classified simple if consciousness not impaired (just motor or sensory effect) and complex if consciousness altered.
Generalized szr both hemispheres; consciousness depressed; convulsive or nonconvulsive
Febrile seizure: seizure w/ febrile illness in pt age 6 mo–5 yo
Simple if <15 min, single episode and generalized seizure, normal neuro exam
Complex if >15 min, recurs within 24 hrs or focal seizure
Etiology: Infectious (febrile, meningitis, brain abscess), neurologic (hypoxic-ischemic encephalopathy, VP shunt malfxn, neurocutaneous syndr), metabolic (electrolyte abn, hypoglycemia, hypoxia, inborn errors of metab), trauma (abuse, ICH), tox, neoplasm.
Evaluation: Assess ABCs (support as needed), hx (PMH of szr’s, antiepileptics, FHx, other meds/toxin expos, recent illness, head trauma), check temp and glucose; obtain IV
Management:
ABCs, finger stick BG, obtain IV (in extremis, then IO access); recheck ABCs
Lorazepam 0.05–0.1 mg/kg IV (max 4 mg); rpt q5 min to max total dose 10 mg in 20 min; place patient on their side to avoid aspiration
Reassess ABCs and need for airway support after each dose
Diazepam, (2–5 yr 0.5 mg/kg; 6–11 yr 0.3 mg/kg; >11 0.2 mg/kg PR; max 5–10 mg), less effective and leads to more resp depression than lorazepam
After 2 doses lorazepam; consider fosphenytoin 20 PE/kg IV; commonly need to secure airway at this time w/ endotracheal intubation; call neurology.
Stridor
Definition
High-pitched sound of turbulent airflow in upper airway indicates airway obstruction.
Inspiratory stridor usually indicates obstruction above the vocal cords.
Expiratory stridor usually indicates obstruction below the vocal cords.
Differential Diagnosis
Causes including croup, epiglottitis and bacterial tracheitis (BT may be most freq life-threatening upper airway infxn currently). (Pediatrics 2006;118:1418.)
Consider differential diagnosis anatomically based on inspiratory or expiratory stridor
Nose: Inspiratory stridor, snoring; in neonates consider choanal atresia
Pharynx: Gurgling/muffled voice
Afebrile: Macroglossia, micrognathia, tonsil/adenoid hypertrophy
Febrile: Retropharyngeal/peritonsillar abscess
Larynx: High-pitched inspiratory stridor, voice change, hoarseness
Afebrile: Laryngomalacia, laryngeal web, cyst, vocal cord paralysis, laryngotracheal stenosis, intubation, foreign body, cystic hygroma, subglottic hemangioma, laryngospasm, psychogenic stridor, vocal cord paralysis
Febrile: Croup, epiglottitis
Trachea: Insp and exp stridor: Tracheomalacia, bacterial tracheitis, external compression, TEF
Croup
(laryngotracheobronchitis)
Characterized by barking cough, +/- inspiratory stridor, +/- respiratory distress.
Peak incidence 1–2 yr of age, Sept to Dec, M > F. Parainfluenza virus accounts for >50%, next most common cause is RSV. (Pediatrics 1983;71:871.)
Mild: Dexamethasone 0.6 mg/kg PO/IM ↓ rpt visits, length of sx, and parental stress, and ↑ sleep (N Engl J Med 2004;351:1306). Also consider cool mist, hydration, and antipyretics.
Can use oral prednisolone 1–2 mg/kg PO; t1/2 of prednisolone 24 hr; t1/2 of Dex is 32 hr.
Moderate to severe:
Mist tent or humidified oxygen near child’s face (Not supported by Cochrane review)
Dexamethasone 0.6 mg/kg PO/IM (N Engl J Med 1998;339:498; meta-analysis in BMJ 1999;319:595).
Racemic epi (2.25%) 0.05 mL/kg/dose in 3 mL NS (max 0.5 mL) q15 min up to 3× PRN, watch HR (Pediatrics 1992;89:302; Cochrane review ongoing)
If epi given, need obs (effects wears off in 2 hr). Obs in ED for min 4 hr.
Decrease epi dose for known cardiac disease.
Equiv of PO vs. IM dosing shown in study of mod croup. (Pediatrics 2000;106:1344)
Epiglottitis
Usually 2/2 Hib. Incidence of Hib ↓ by >99% since intro of conj vaccine in 1998 (MMWR 2002;51:234) P/w toxic child, drooling, sitting forward, stridor.
True emergency requiring immediate intubation in controlled environment (if possible), any manipulation of child may cause full obstruction.
Give O2 as accepted by child, allow parent to accompany child to allay anxiety.
Summon senior pediatrician, anesthesiologist, and ENT or pediatric surgeon.
If unstable, intubate emergently; bag-mask w/ high pres, may need to disable pop-off valve.
If stable with high suspicion (toxic, febrile, leaning forward, audible stridor, uncertain vaccination record) escort pt to OR for laryngoscopy/intubation.
If moderate/low suspicion, obtain lat neck x-ray (thumbprint sign), will agitate them
Once airway secure, check CBC/diff, cx of blood and epiglottis, start Abx (such as ceftriaxone) covering HIB, S. pneumo, and Grp A strep
Bacterial Tracheitis
(Pediatrics 2006;118:1418; Emerg Med Clin North Am 2007;25:961)
Commonly seen fall/winter, 6 mo–8 yr
Presentation: viral prodrome followed by acute onset of toxic appearance, high fever (mean 101.8°F/38.8°C), cough, resp distress. Unlikely to drool, may be able to lie flat.
Management: To OR for endoscopy to obtain sample for GS and cultures and intubation. If intubating in ER consider smaller ETT than usual because of airway edema.
Abx to cover S. aureus, S. pneumo, M. catarrhalis, H. flu, and alpha-hemolytic strep.
CXRs usually normal or similar to croup (steeple sign), blood cx usually negative.
Diagnostic Studies
Initial eval w/ CXR lat/AP neck film; ENT (direct laryngoscopy), consider fluoro if available
Anaphylaxis
(Pediatrics 2000;106:762; Pediatr Emerg Care 2007;23:49; J Allergy Clin Immunol 2006;117:391)
Definition
Anaphylaxis is a serious systemic allergic reaction, which is rapid in onset and may cause death.
IgE mediate hypersensitivity mediated by mast cells and basophils
Symptoms of Anaphylaxis
| Skin | Diaphoresis, flushing, pruritus, urticaria, warm sensation, angioedema |
| Respiratory | Oropharynx/lip tingling or itching, throat/chest tightness, hoarseness, stridor, wheezing, dyspnea, respiratory failure |
| GI | Nausea, diarrhea, vomiting, cramps |
| CV | Arrhythmias, hypotension, shock, arrest |
| Neuro | Dizziness, visual changes, tremor, disorientation, syncope, seizures |
| Other | Impending sense of doom, metallic taste, rhinorrhea, tearing |
Criteria for Anaphylaxis
Highly likely when any 1 of the following 3 criteria fulfilled:
Acute onset (min to hrs) involving skin &/or mucosal tissue & ≥1 of following
Respiratory compromise (e.g., dyspnea, wheeze, stridor, hypoxemia)
Reduced SBP or assoc sx of end-organ hypoperfusion (e.g., syncope, hypotonia)
≥2 of the following occurring rapidly (min to several hr) after exposure to allergen
Skin and/or mucosal involvement (hives, itching, flushing, and swollen lips, tongue or uvula)
Reduced SBP or associated symptoms of end-organ hypoperfusion.
Respiratory compromise
Persistent GI symptoms
Reduced SBP after exposure to a known allergen for that pt (min to several hr)
Management
Initial management assess ABCs; place patient on CVR/O2 monitor, continuous BP monitor
If severe:
IM/SC epinephrine (1:1000 solution, 0.01 mg/kg (0.01 mL/kg) max ∼0.3 mg (0.3 mL). IM preferred
Repeat q5–15 min as needed; Inhaled epi not as effective 2/2 inhaling insuff amts.
Obtain IV/IO access: IV fluids 20 mL/kg bolus ×3 followed by use of pressors (epi).
Inhaled β2-agonists can be helpful, especially if Hx of asthma
Consider H1-H2 antihistamines to slow onset of reaction, cannot block events that occur subsequent to histamine receptor binding; better to give H1-H2 together than just H1
Diphenhydramine IV (1.25 mg/kg/dose up to 50 mg/dose)
Ranitidine IV (0.5–1 mg/kg up to 50 mg/dose)
Corticosteroids: no clinical trial (most helpful in pt w/ Hx of recent steroid use, asthma, or endogenous corticosteroid deficiency); no effectiveness against biphasic reactions.
Methylprednisolone IV 1–2 mg/kg up to 125 mg/dose.
Observation: Usual observation is 6–8 hr.
Late reactions occur in up to 20% of patients and as late as 72 hr.
Factor to include: severity of the initial reaction, adequacy of supervision, reliability of the patient/parent, and ease of access to medical care.
High risk of latent rxn: Hx of previous biphasic rxn, asthma, and possibility of continuing absorption of antigen or those who presented w/ severe refractory symptoms.
Outpatient Management
EpiPen (0.30 mg) and EpiPen Jr (0.15 mg). Give closest to 0.01 mg/kg/per dose.
May be difficult with <10 kg 2/2 to overdosing, consider EpiPen Jr.
Provide instructions. Use www.epipen.com for helpful information.
If used as outpatient, must return to the ED.
Apparent Life-threatening Event (ALTE)
Definition
(Pediatr Clin North Am 2005;52:1127)
Described as an event frightening to the observer and including any of the following:
Apnea: can be central (no resp effort) or obstructive (breath w/ paradox inverse motion of chest/abd and ↓ O2 sat by 3%.) Significant apnea >20 sec or shorter w/ ↓HR or hypotonia
CHIME (1,079 infants on home card-resp monitors) – 43% w/ apnea and bradycardia >20 sec w/o diff in freq btw “healthy” infants and those w/ Hx idiopathic ALTE requiring vigor stim and CPR. # events >30 sec similar in both groups (Pediatr Rev 2007;28:203)
Change in color: Central cyanosis (>5 g/dL deoxyhemoglobin) w/ bluish lips or tongue.
Distinguish from acrocyanosis (nml bluish color of hands and feet) and circumoral cyanosis; both of which are benign in absence of other signs of shock or sepsis.
Change in muscle tone
Coughing or gagging.
May or may not require stimulation to resolve (stim includes being picked up by caregiver).
Uncomplicated ALTEs not related to SIDS (in fact, ALTEs and SIDS have different risk factors and campaigns that have dec rates of SIDS have not had impact on ALTEs).
Incidence
(Am Fam Physician 2005;71:2301; Pediatr Clin North Am 2005;52:1127)
0.01%–0.5%; by definition <1 yo (most <10 wk); though limited data.
Etiology determined in 50% if cases. (Arch Dis Child 2004;89:1043)
Risk factors: Repeated apnea, pallor, Hx of cyanosis, feeding difficulties prematurity
| Ddx | GI (reflux, colic, gastroenteritis) 31%–33% in collected series Idiopathic 23%–28% in collected series CNS (seizure, head trauma, perinatal hypoxic ischemic encephalopathy, congenital, central hypoventilation) 11%–15% in collected series Respiratory (RSV, RAD, PNA, pertussis, foreign body) 8%–11% in collected series ENT 4% (laryngomalacia, laryngeal/subglottic stenosis, OSA) Abuse (shaken baby syndrome, Münchhausen-by-proxy) Breath-holding, periodic breathing Other infections (sepsis, botulism, meningoencephalitis) Metabolic (HypoNa/Ca/glycemia, CAH, acidosis) Congenital (vascular ring) Cardiac (CHD, cardiomyopathy, arrhythmia) Toxic (ingestion) Anemia |
| Useful history | Recent illness, relation to sleep/feeding/position, birth history, appearance (color, tone), duration, sequelae, response to stim, h/o seizures, fitful sleeping, snoring, mouth breathing, location of event (parents bed, 1st d in day care), position found (prone) |
Diagnostic Studies
In 1 study of 239 cases, 17.7% of tests +, 5.9% contributed to dx. (Pediatrics 2005;115:885)
High-yield testing: High-yield tests suggested by H&P. If nothing suggested, consider U/A and Ucx, WBC, GER screen (pH probe), neuroimag, pneumogram. (Pediatrics 2005;115:885) consider toxicology as well; not looked at in this study
Low-yield testing: Can consider lytes, ABG, full septic w/u, viral panel, EKG, EEG, lat neck films, CXR, barium swallow, “milk scan” (contrast scintigraphy), CVR monitoring o/n.
Management
Admission: Study (59 infants) w/ use of high-risk criteria (age <30 d old and multi ALTEs in 24 hr) predicted w/ 100% sens all cases needing hospitalization. (Pediatrics 2007;119:679) Also high risk if premature or <43 wks corrected. (J Pediatr 2008;154:332)
Proposes that nontoxic full term pts, w/ nml exam and >30 d old p/w 1st ALTE, safe to d/c home.
Consider admission if complex resuscitation required, abnormal PE or results
Other: Consider CPR training for parents
Home monitoring appt in preterm at-risk, high-risk recurrent apnea, bradycardia, and hypoxemia following d/c or w/ infants who are equipment dependent, have conditions affecting resp reg, or those w/ unstable airways. (Pediatrics 2005;115:885)
Prognosis
No develop diff in f/u studies at 10 yr, some ↑ breath-holding at 3 yr. ↑ risk of subsequent SIDS, only if recurrent episodes require CPR.
Fever without an Identified Source in Infants and Children
**These guidelines DO NOT replace clinical judgment. If in doubt, always err on the side of conservative management. Close follow-up continues to be the most important tool for evaluating children with fever. Caretakers of febrile children under 36 mo old should be in daily contact with a medical provider.**
Definition
(Emerg Med Clin North Am 2007;25:1087)
Most common def of fever is core temp >38°C (higher levels used for eval in pts >3 mo of age)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


