The Institute of Medicine (IOM) report
Crossing the Quality Chasm first called for elimination of handwritten data and set a goal to implement a paperless EHR before the end of the decade, citing evidence that the EHR improves health care quality, safety and efficiency.
1 The electronic format provides a record of clinical data that is legible, organized, complete, and accessible by multiple users across sites of care and episodes of care. In addition, the digital record creates a database of clinical information that can be automatically analyzed. This IOM report energized the development of health information technology (HIT) and the application of information processing technology (computer hardware and software) to enable the collection, analysis, storage, retrieval, and sharing of health care data, information, and knowledge for communication and decision-making. In 2009, The American Recovery and Reinvestment Act (ARRA) and the Health Information Technology for Economic and Clinical Health Act (HITECH Act) created funding and reimbursement incentives for the adoption of EHRs that included expectations for using certified systems (
the right technology) for standard use (
the right use of technology), commonly referred to as “meaningful use.”
2,
3 The Office of the National Coordinator for HIT (ONC) is the complete source for a current list of certified technology products and specific meaningful use criteria (Office of the National Coordinator for Health Information Technology [ONC]).
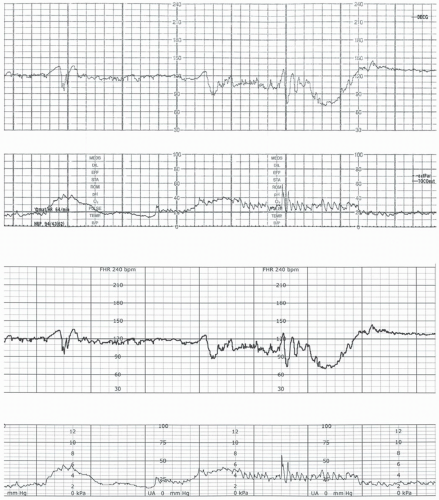
4 The ARRA goals include improving care coordination through the effective use of HIT and effective health information exchange (HIE), goals that are relevant to obstetric patients and fetal monitoring. Effective use aims to bring key data directly to the frontline providers at the point-of-care, reduce duplicative work, and provide access to clinical data immediately (such as data entry of the mother’s expected delivery date that is entered once and flows to all parts of the medical record simultaneously, or immediate access to interpret and document on a fetal tracing). Effective HIE aims to improve interoperable data standards, so information is portable, travels with the patient, and can be shared among providers (such as access to prenatal FHR assessments and diagnostics). Collectively, these strategies will deliver the right information to the right person at the right time.
The transition to an EHR poses education and practice challenges for clinicians. A multidisciplinary summit sponsored by the American Health Information Management Association addressed such training needs and listed specific actions for not only health care workers, but for employers, vendors, educators, and the government to promote workforce competencies.
5 This panel recommended that health care workers themselves self-assess knowledge gaps and seek ongoing professional development. Obstetric clinicians must recognize how the national agenda
is shaping EFM practice with clinical information systems and informatics.