Electronic Fetal Heart Rate Monitoring Equipment and Technology
To accurately interpret the data presented by the electronic fetal monitor, it is necessary to have a basic understanding of both the workings and the limitations of the equipment. The greatest effect on the data is produced by the mode of monitoring used. Information about both the fetal heart rate (FHR) and uterine activity may be gathered using sensors that are placed either internally or externally.
Acquisition of Fetal Heart Rate Data
Fetal Electrocardiogram (FECG)
Signal Processing
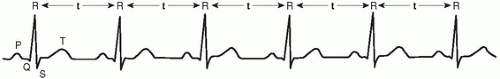
The most accurate means for assessing the FHR is through internal monitoring, currently accomplished by using the spiral electrode. The lead wires of the spiral electrode conduct the electrical signal of the fetal QRS waveform complex (FECG) to the electronic fetal monitor. From the FECG data, the electronic fetal monitor determines the FHR. The cardiotachometer is a component within the electronic fetal monitor that converts the FECG signal into the FHR. This processing is accomplished through the application of a mathematical equation:
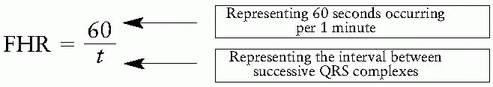
To determine the unknown factor of t to enter into this equation, the cardiotachometer measures the time elapsed between the R peaks of successive QRS complexes (Fig. 2-1).
Trending of Data
Once the factor of t is determined, it is then entered into the equation, FHR = 60/t. The product of this equation is the FHR, expressed in beats per minute (bpm). The FHR is then plotted on the FHR channel of the strip chart in bpm. Sinus arrhythmias are normal in the fetus and present as varying R-R intervals (t). Longer R-R intervals are represented by a slower FHR, whereas shorter R-R intervals are exhibited as a faster FHR. These fluctuations of the FHR from one beat to the next are recognized in the FHR tracing as baseline variability. (Note: Prior to the adoption of National Institute of Child Health and Human Development [NICHD] terminology [NICHD, 1997; American College of Obstetricians and Gynecologists (ACOG), 2005; Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN), 2006] into clinical practice, this data [obtained only via internal monitoring] was further distinguished by use of the term short-term variability. Observation of the continuous recording of this data over a period of time allowed for even further determination of variations in the FHR baseline, previously known as long-term variability.)
Ultrasound
The FHR may also be determined from the signal acquired through use of external sensors. When properly placed on the maternal abdomen, the ultrasound transducer detects the movements of the
fetal heart that occur with each beat. The ultrasound transducer contains crystals that transmit and receive high-frequency sound waves using the piezoelectric effect. The piezoelectric effect is the conversion of electrical energy into mechanical sound wave energy and vice versa. This is accomplished in the ultrasound transducer by the application of voltage to the crystals, which causes them to vibrate at a predetermined frequency. When this sound wave meets the fetal heart, its frequency becomes either compressed or stretched by the beating motion of the fetal heart and is reflected back to the crystals. The reflected sound wave is converted back into electrical energy at a frequency altered from the original transmitted frequency. The difference between the frequency of the sound wave that is transmitted and that which is reflected back is referred to as the Doppler shift. The Doppler shift frequency can be used to produce the audible sound that is recognized as the fetal heart beat and also provides the raw data from which the FHR can be determined by using the equation, FHR = 60/t.
fetal heart that occur with each beat. The ultrasound transducer contains crystals that transmit and receive high-frequency sound waves using the piezoelectric effect. The piezoelectric effect is the conversion of electrical energy into mechanical sound wave energy and vice versa. This is accomplished in the ultrasound transducer by the application of voltage to the crystals, which causes them to vibrate at a predetermined frequency. When this sound wave meets the fetal heart, its frequency becomes either compressed or stretched by the beating motion of the fetal heart and is reflected back to the crystals. The reflected sound wave is converted back into electrical energy at a frequency altered from the original transmitted frequency. The difference between the frequency of the sound wave that is transmitted and that which is reflected back is referred to as the Doppler shift. The Doppler shift frequency can be used to produce the audible sound that is recognized as the fetal heart beat and also provides the raw data from which the FHR can be determined by using the equation, FHR = 60/t.
Continual transmission and reception of sound waves to and from the ultrasound transducer is known as “continuous wave” ultrasound. This is accomplished by having certain crystals dedicated to emitting sound waves, whereas others only receive the reflected signal. Continuous wave ultrasound was used in early versions of the ultrasound transducer until it was replaced by pulse Doppler technology. Pulse Doppler ultrasound allows all of the crystals in the transducer to both send and receive sound waves. Each of the crystals inside the transducer is timed to transmit sound waves and then “standby” for a predetermined period (the amount of time it takes for the signal to be transmitted and reverberated). The crystals are then reactivated as receivers for the ultrasound signal as it is returned for processing. Pulse Doppler ultrasound makes it possible to monitor more than one fetus simultaneously. Because of the timing built into each crystal, the signal emitted by the ultrasound transducer for the purpose of evaluating one fetus will not be received by the ultrasound transducer that is tracking the second fetus.
Signal Processing
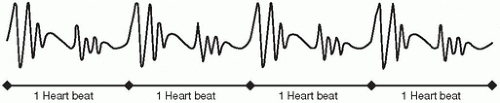
The external mode of monitoring requires different processes for identifying the factor of t for use in the equation, FHR = 60/t, than that which is used with internal monitoring. Determining the factor of t is very straightforward with internal monitoring—it is the time elapsed between the clearly identifiable, successive R peaks of the QRS complex. The raw data gathered by the ultrasound transducer do not contain such distinct reference points from which the factor of t may be figured. These data are created by electronically comparing the reflected ultrasound signal to the transmitted signal. The original signal is “subtracted” from the reflected signal, and the resulting waveform is representative of the motion of the fetal heart (Fig. 2-2). To facilitate determination
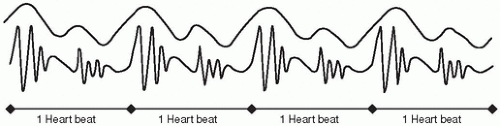
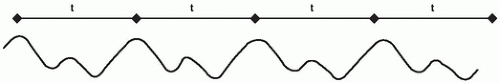
of the factor t, the waveform is filtered to reduce the amount of high-frequency component. These filtered waveforms are irregularly shaped and lack an obvious common distinguishing element from which the timing of the occurrence of one waveform could be compared to that of the next (Fig. 2-3). To assist in converting these raw data into useful information, the monitor employs a method referred to as autocorrelation. Autocorrelation is a process of successively comparing waveforms to identify their similarities. Once such features are recognized, a template of the waveforms is created and is used as a comparison to incoming waveform data (Fig. 2-4). As correlations in the data are determined, the factor of t can be calculated from the peaks of the correlation function.
of the factor t, the waveform is filtered to reduce the amount of high-frequency component. These filtered waveforms are irregularly shaped and lack an obvious common distinguishing element from which the timing of the occurrence of one waveform could be compared to that of the next (Fig. 2-3). To assist in converting these raw data into useful information, the monitor employs a method referred to as autocorrelation. Autocorrelation is a process of successively comparing waveforms to identify their similarities. Once such features are recognized, a template of the waveforms is created and is used as a comparison to incoming waveform data (Fig. 2-4). As correlations in the data are determined, the factor of t can be calculated from the peaks of the correlation function.
Trending of Data
Another difference of external versus internal monitoring is that information concerning the individual intervals between each successive fetal heart beat is not represented in the FHR tracing. Instead, once the factor of t is determined, it is applied in the equation FHR = 60/t and then averaged over several successive beats. It is only after this multiple beat average has been calculated that the FHR is determined and plotted on the strip chart. This averaging process is repeated continuously as data become available. Fluctuations in the FHR will be represented by variations in these averaged figures as the trend of the FHR is traced over a period of time. These variations are recognized by the clinician as baseline variability. (Note: Prior to the adoption of NICHD terminology [NICHD, 1997; ACOG, 2005; AWHONN, 2006] into clinical practice, fluctuations in the FHR obtained via external monitoring were further distinguished by use of the term long-term variability. Today, in accordance with current recommendations, the distinction between long- and short-term variability is no longer made. The visibly apparent fluctuations in the recorded trend of the FHR baseline [whether obtained internally or externally] are now simply referred to collectively as baseline variability.)
Limitations of Technology
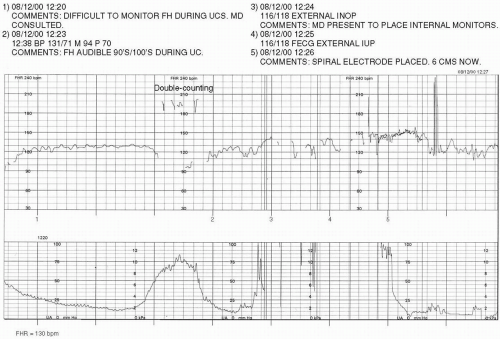
Half-Counting and Double-Counting. The ultrasound transducer is able to recognize the FHR that is occurring within the range of approximately 50 to 180 bpm. As the FHR nears the outer limits of this range, it may be difficult to obtain a clear signal by external means. Occasionally, when the FHR nears the lower limits of the capacities of the ultrasound transducer, the electronic fetal monitor may begin to erroneously consider the motion data resulting from one heart beat to instead be that of two separate beats. This is exhibited by the intermittent trending of the FHR on the strip chart at twice the actual rate. Such an event is referred to as double-counting
(Fig. 2-5). If the FHR nears the upper limits of the capability of external monitoring, half-counting may occur. The monitor may only recognize every other section of motion data as a heart beat, thereby intermittently presenting the FHR at half the actual rate on the strip chart (Fig. 2-6). During the occurrence of both double-counting and half-counting, the audible signal will remain accurate and can be used as an indicator of the actual FHR. Internal monitoring may be selected as a remedy to either event because neither double-counting nor half-counting occurs during the use of this mode of monitoring.
(Fig. 2-5). If the FHR nears the upper limits of the capability of external monitoring, half-counting may occur. The monitor may only recognize every other section of motion data as a heart beat, thereby intermittently presenting the FHR at half the actual rate on the strip chart (Fig. 2-6). During the occurrence of both double-counting and half-counting, the audible signal will remain accurate and can be used as an indicator of the actual FHR. Internal monitoring may be selected as a remedy to either event because neither double-counting nor half-counting occurs during the use of this mode of monitoring.
Maternal Signal. The maternal pulse should be assessed and compared against the electronic fetal monitor’s audible signal each time electronic fetal monitoring (EFM) is initiated or the mode of monitoring is changed (Murray, 2004; Doyle & Angelotti, 2004). The maternal heart rate may be transmitted by either mode of monitoring. The spiral electrode conducts electrocardiography (ECG) information to the electronic fetal monitor. In most cases, there are two sets of ECG data available—fetal and maternal. The electronic fetal monitor recognizes the stronger of these two signals. As the spiral electrode is applied directly to the fetus, the FECG is expected to provide the stronger signal. If the spiral electrode is inadvertently applied to maternal tissue or to a fetus who is not alive, the maternal signal will appear stronger and, therefore, be the one that is transmitted (Fig. 2-7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree