Chapter 23 Disorders in the puerperium
POSTPARTUM HAEMORRHAGE
Primary postpartum haemorrhage (PPH)
Aetiology
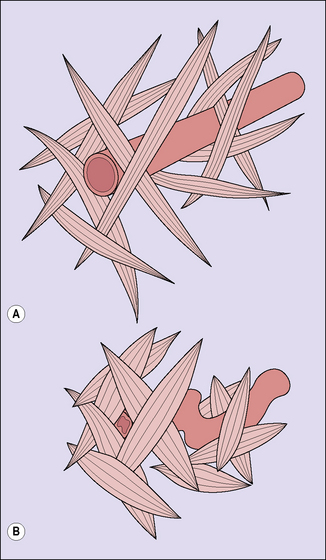
In normal labour, following the birth of the baby a blood loss of 200–600 mL occurs before myometrial retraction, supplemented by strong uterine contractions. This causes shortening and kinking of the uterine blood vessels and a retraction of the placental bed. These changes prevent further blood loss (Fig. 23.1). Some discussion arises as to whether this traditional quantity of blood loss is an underestimate, when blood loss is measured accurately. Provided the blood loss is less than 800 mL, the woman should have no problems.
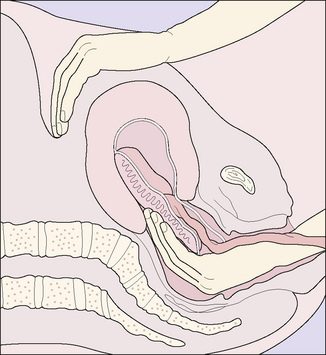
In 20% of cases the cause of bleeding is a laceration of the genital tract, usually of the vagina or cervix, but rarely following uterine rupture (see p. 180). In a few instances PPH follows a blood coagulation defect, such as may occur following abruptio placentae.
Management
Third-stage bleeding (placenta in the uterus)
True postpartum haemorrhage (placenta expelled)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree