Chapter 18 Diseases of the placenta and membranes
ABNORMAL PLACENTATION
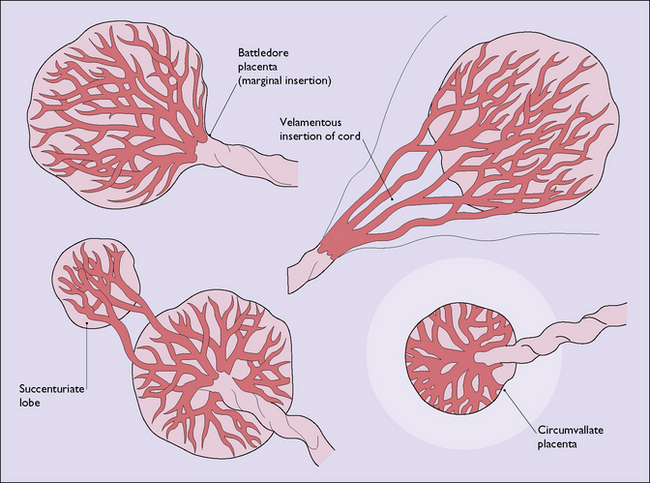
The shape of the definitive placenta is determined at the time the placenta forms, the variations found (Fig. 18.1) mostly having no clinical significance.
GESTATIONAL TROPHOBLASTIC DISEASE
Gestational trophoblastic disease is uncommon affecting 1/750 pregnancies of women of non-Asian ethnicity but 1/380 of those from Asia. It is potentially lethal, but with treatment a 98% cure rate is attainable. The disease occurs in two forms (Box 18.1).
Hydatidiform mole
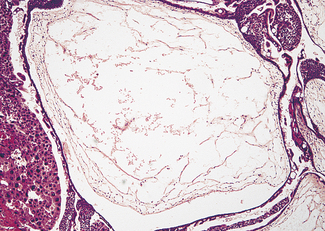
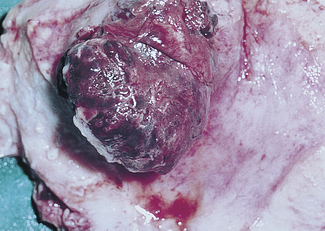
The tumour may have completely or partially replaced the placenta (Fig. 18.2). In the complete form, hydropic swelling and vesicle formation is associated with trophoblastic proliferation and a paucity or absence of blood vessels within the villi (Fig. 18.3). No fetus can be found. Five per cent of complete moles undergo malignant change.

Fig. 18.2 Benign trophoblastic tumour (hydatidiform mole): gross specimen. Note the grape-like masses.
Malignant trophoblastic disease
In choriocarcinoma (Fig. 18.4) the tumour is characterized by sheets of trophoblastic cells, both syncytio- and cytotrophoblasts, with few or no villi formed.