A human embryo is susceptible to the effects of ionizing radiation because of rapidly proliferating cells present therein. Doctors Douglas Murphy and Leopold Goldstein first described these effects in 1928 to 1929. They reported on the offspring of mothers who had received radiation while pregnant. Over 50% had abnormalities including a high prevalence of microcephaly.3 Survivors of the atomic bomb in Japan also provided information about radiation exposure in pregnancy. Prenatal exposure to such high doses of radiation produced an increased risk for microcephaly, mental deficiency, and growth deficiency.4 It is estimated that doses of 50 rads (500 mGy) or greater would produce these effects. During the first two weeks after conception, the main risk is spontaneous miscarriage, usually at doses of 10 rad (100 mGy) or higher. Between 4 and 17 weeks, the main concern is for CNS abnormalities, mental retardation, and microcephaly increases but again, at doses more than 10 rads. None of these adverse outcomes appear to be present with radiation levels less than 5 rads which fortunately is higher than the radiation dose for any one single imaging procedure.5
CANCER RISKS FROM PRENATAL RADIATION EXPOSURE
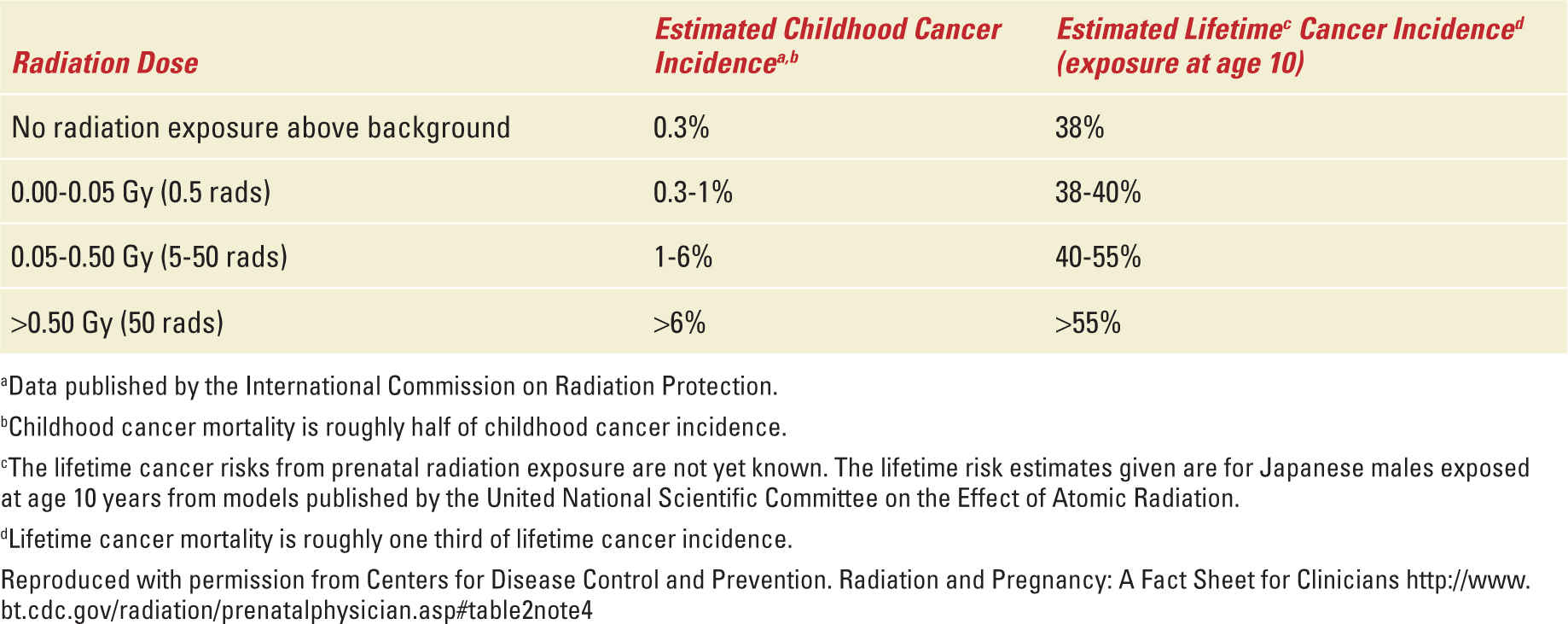
In 2009, a study was published demonstrating the link between radiation exposure from CT scans and an increased risk for cancer.6 The carcinogenic risk for childhood cancers after fetal exposure to radiation appears to be increased as well, but this is much debated.7 The exact risk is unclear and whether the effect for a particular dose varies with gestational age is unknown and is currently thought to be constant throughout gestation. There is some suggestion that the human embryo may be more sensitive to the leukemogenic effects of radiation exposure and fetuses exposed to radiation may be more likely than an adult exposed to that same level. Most diagnostic procedures fall in the 0 to 5 rad range; therefore, the risk for childhood cancer would be 0.3% to 1% for any child exposed to a radiologic test in utero (Table 36-2).
Estimated Risk for Cancer from Prenatal Radiation Exposure |
CONTRAST AGENTS
A concern also exists for the contrast agents used in imaging and their effects on the fetus. Gadolinium (mainly used in MRI) and iodinated agents (mainly used in CT scan) are the most commonly used contrast media in imaging. Gadolinium has been shown to cross the placenta in animal studies.8 Animal studies have shown teratogenic effects in high and repeated doses.9 No adverse effects have been seen in human fetuses but studies are limited. Gadolinium is considered pregnancy category C and can be used if the benefit of obtaining the information outweighs the risk. Animal studies have also failed to show a risk of teratogenesis for iodinated contrast media. The iodine found in CT contrast media does have the potential to induce hypothyroidism in the fetus, but fortunately there have been no reports of such effects from iodinated intravenous contrast.10
MINIMIZING RISKS
Although minimizing the risk to the fetus from undo radiation exposure is one goal for any given procedure, making an accurate diagnosis and optimizing therapy to the mother is also of utmost importance. Knowing the correct imaging modalities available for a suspected diagnosis, its application, safety, and alternatives can help when deciding how to approach the workup and counseling of patients about the risks of imaging for a particular disorder. There are many common clinical situations and illnesses encountered in pregnancy that may require imaging. In the abdomen conditions, such as appendicitis, cholecystitis/pancreatitis, urinary calculi, pelvic thrombosis, and masses (some suspicious for malignancy or infection) are often encountered. Pulmonary emboli and cardiac disease can occur in the chest. Central nervous system complications include subarachnoid hemorrhage (SAH); venous thrombosis and strokes may be encountered. Maternal trauma may also require imaging. In general, the guiding principle should be to perform any exam [CT, MRI, intravenous pyelograms (IVP), fluoroscopy] needed to make a diagnosis with care to minimize the risks to mother and fetus. On occasion, it may be necessary to use the modality that carries a higher radiation risk over one with less risks but which is not as diagnostic. Therefore, it is important to know which imaging approach has the highest yield for specific clinical scenarios.
Abdomen
When pregnant women present with acute abdominal pain, conditions such as appendicitis, cholecystitis, pancreatitis, and ovarian torsion are the most frequent to consider. The most common indication for abdominal surgery (nonobstetrical) during pregnancy is appendicitis. Appendicitis occurs in 1 in 1700 pregnancies.11 The most common diagnostic modality used in the evaluation of a pregnant patient suspected of having appendicitis is ultrasonography. Although the benefit of this modality is that no ionizing radiation is involved, the sensitivity may be limited with reports ranging from 65% to 100% during pregnancy.12 If clear visualization of the appendix cannot be achieved, the diagnosis of appendicitis cannot be excluded and further diagnostic imaging may be indicated. Second-line imaging techniques for evaluation include noncontrast MRI and CT. The incorporation of MRI into the workup of abdominal pain suspicious for appendicitis has been associated with a decreased negative laparotomy rate without a significant increase in the perforation rate. Sensitivities, specificities, positive predictive values, and negative predictive values have been reported to be 90% to 100%, 93% to 98%, 61% to 82%, and 99% to 100%.13–15 A patient with a negative MRI is unlikely to need an emergent appendectomy. CT is highly sensitive for the detection of appendicitis (92%). It is also valuable in the detection of alternate pathology as a cause of lower abdominal pain. The main concern is the risk of radiation exposure. However, the average dose using most protocols is low (probably between 20 and 43 mGy or 2-4.3 rads) and certainly within what is considered an acceptable range for a pregnancy.
Cholelithiasis/Pancreatitis
Gallstones are thought to occur in about 3% to 12% of all pregnancies.16 Ultrasound is the best initial modality to evaluate the liver and biliary systems. Although ultrasound is sensitive for diagnosing cholelithiasis, gallstones of the common bile duct (CBD) are not as readily imaged and the sensitivity for detecting stones of the CBD may be only as high as 38%.17 Magnetic resonance cholangiopancreatography (MRCP) seems to be an effective modality for diagnosing choledocholithiasis and is probably the most appropriate second line imaging test for suspected biliary disease. Gadolinium is not necessary for MRCP.15 MR imaging also is useful for evaluating the pancreas, as it is sensitive for detecting pancreatic edema, ductal obstruction, and peripancreatic inflammation. ERCP, endoscopic retrograde cholangiopancreatography, is also an effective modality for imaging as well as treating choledocholithiasis. However, it is invasive, requires sedation, and exposes the patient and the fetus to ionizing radiation. Endoscopic ultrasound (EUS) may be an alternative to ERCP for the diagnosis of CBD stones; however, its use in pregnancy has not been well defined. EUS entails no radiation exposure and appears to be safe. If a CBD stone is discovered, ERCP with sphincterotomy can be performed in the same setting.
Urinary Calculi
Nephrolithiasis resulting in obstruction occurs in about 1 in 3300 pregnancies.18 Ultrasound is the preferred method to image suspected renal stones because of lack of ionizing radiation. The sensitivity of ultrasound for obstructive renal stones in pregnancy ranges between 34.0% and 95.2%.19,20 Physiologic changes limit the accuracy of diagnosis especially the normal physiologic dilation of the collecting system. Doppler ultrasound for the calculation of the intrarenal resistive index (RI) may be helpful in the diagnosis. Normal pregnancy does not typically affect the intrarenal RI; therefore, an elevated value will reflect an obstructive process. An RI ≥0.70 or a difference in the RI between normal and abnormal kidneys of ≥0.04 has been associated with unilateral obstruction in pregnant women.21 The absence of ureteral jets may also indicate obstruction by a stone; however, 15% of asymptomatic pregnant women can have absent ureteral jets.22 IVP is not recommended as a first line test for the evaluation of nephrolithiasis during pregnancy. Presence of the fetus often obscures adequate visualization and the radiation dose delivered is not significantly lower than the dose from CT using the standard “stone protocol.”23 CT also has the benefit of detecting other pathology as an etiology for abdominal pain if urolithiasis is excluded as a cause. Fast MR urography confers no ionizing radiation and may also represent an alternative to CT if the ultrasound is unremarkable and there are persistent symptoms despite conservative therapy. Distinct differences in the appearance of pathologic hydronephrosis and physiologic hydronephrosis have been described in pregnant patients making this a viable alternative.24 When compared the positive predictive value of CT, MR urography, and ultrasound are 96%, 80%, and 77%, respectively.25 A plain abdominal x-ray film may demonstrate calcium oxalate stones with minimal radiation exposure (100 mrad).
Pelvic Thrombosis
Ultrasound has been shown to reliably diagnose venous thrombosis of the lower limbs. The sensitivity and specificity of ultrasound for detecting proximal deep venous thrombosis (DVT) is reported to be 95% and 98%, respectively.26 However, thrombi in the pelvis are not as readily identifiable with ultrasonography. The alternative method of choice, which is especially helpful in the cases of suspected pelvic thrombi, is magnetic resonance venography (MRV). MRV can be carried out without intravenous contrast and is superior in the assessment of thrombosis in the vena cava and pelvic veins.27 It can also be used in cases where clinical findings support the suspicion of a clot in the deep veins of the leg that were not seen on initial compression ultrasonography. Contrast venography is considered the gold standard for diagnosing DVTs. Although the most accurate, the exposure to radiation has resulted in its replacement by ultrasound and MR venography.
Pelvic/Adnexal Masses
Ultrasound is the initial imaging modality of choice for most pelvic/adnexal masses. A large number of studies attest to the sensitivity of ultrasound for characterizing masses especially when arising from the ovary or adnexa.28 MRI can be used in cases where the ultrasound is nondiagnostic and may better characterize the origin of the mass.29
Pulmonary Emboli
Venous thromboembolism is the leading cause of maternal death in the developed world.30 The diagnosis if pulmonary embolism (PE) during pregnancy can be difficult. Many of the associated symptoms such as shortness of breath, tachycardia, and leg edema may be found in normal pregnancies. In pregnancy, there are no prospective clinical prediction models available. Although avoiding fetal radiation is of concern, a fatal misdiagnosis weighs more heavily in the decision algorithm. The American Thoracic Society recently published guidelines to aid clinicians in the diagnosis of PE in pregnancy. First, the panel recommended that D-dimer NOT be used to exclude PE. There have been case reports of false negatives in pregnancy and the data do not currently justify its use in the pregnancy setting. If a pregnant patient with suspected PE also has signs of DVT then bilateral lower extremity Doppler (CUS) should be performed. If positive, then anticoagulation can be initiated without further workup. If negative, additional testing is necessary. In pregnant patients without symptoms of DVT, the utility of CUS to diagnose DVT to avoid further workup with radiation-emitting modalities is unclear. The number needed to image will likely be higher because of lower prevalence of DVT in pregnant patients with PE when compared to the nonpregnant population. The initial study should be one that images the pulmonary vasculature. The panel also recommends a chest x-ray (CXR) in all pregnant women with suspected PE. The results are used to triage between lung scintigraphy (V\Q scan) and CT pulmonary angiography (CTPA). If patients have a normal CXR, then lung scintigraphy should follow as the next test rather than CTPA. If the V\Q scan is nondiagnostic, then additional testing with CTPA is recommended. If the CXR is abnormal, then CTPA is the next step in the evaluation31 (Figure 36-1).
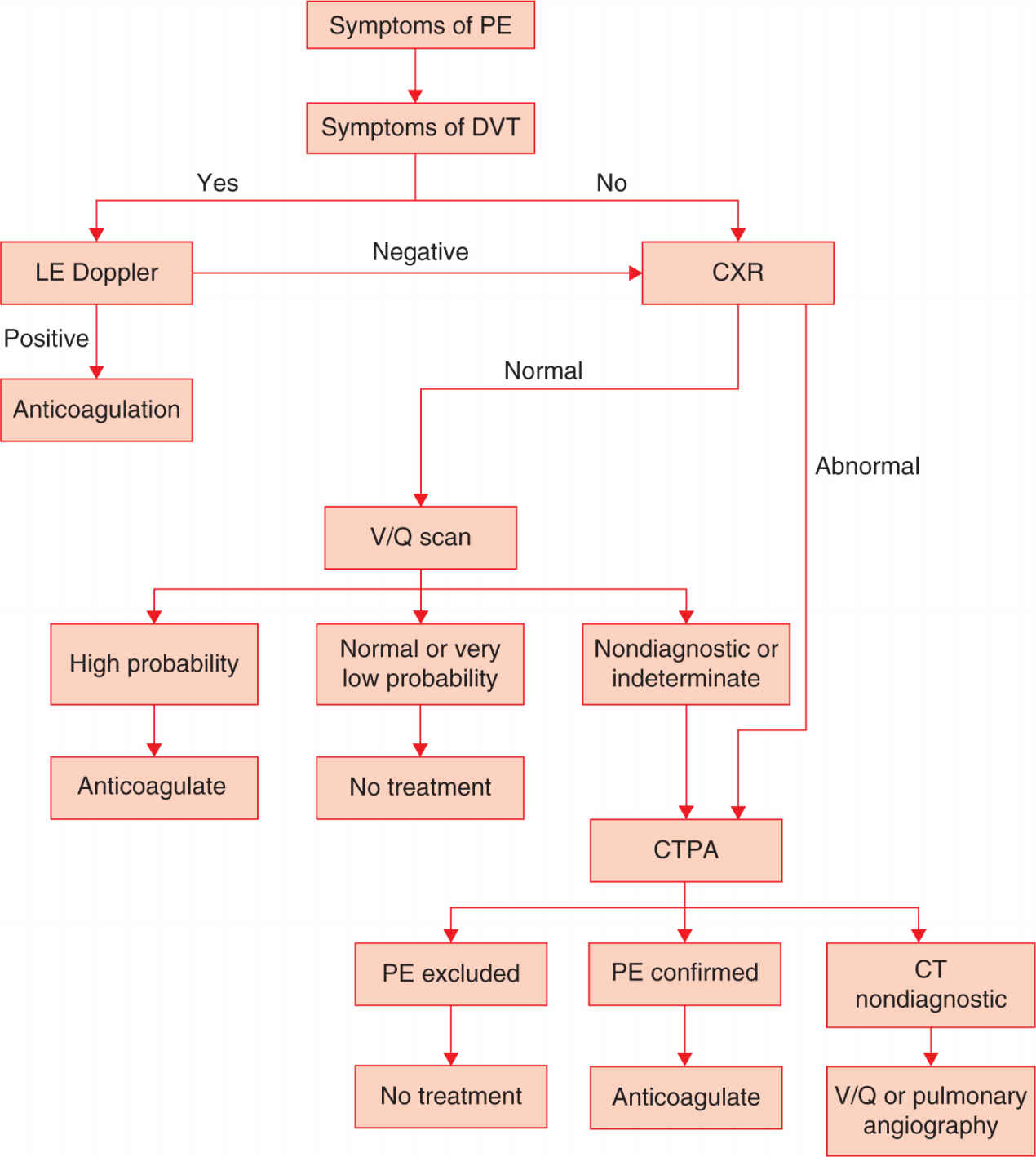
FIGURE 36-1. Evaluation for pulmonary embolism.
Cardiac Disease
Cardiovascular disease is a major cause of maternal morbidity and mortality. Hypertensive disorders combined with the ever-increasing population of women with congenital heart abnormalities who now give birth has resulted in cardiovascular disease now ranked as the leading cause of pregnancy associated maternal morbidity.32 Most pregnant women with cardiac disease undergo echocardiography, which will adequately assess the structure and function of the heart. If stress testing is needed, Dobutamine has also been safely used in pregnancy. Table 36-3 lists some of the indications for echocardiography in pregnancy.
Indications for Echocardiography |



