3 Developmental–Behavioral Pediatrics
Developmental Assessment
Developmental Screening
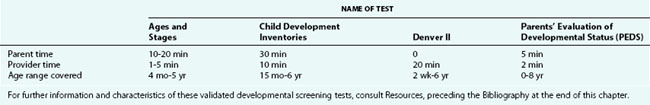
The physician’s ability to identify children with developmental delays and disorders is improved by the appropriate use of validated screening tools (Table 3-1). The tools have been designed to be used with unselected groups of children, ideally as part of routine developmental surveillance at a few selected health maintenance visits, such as the 9-, 18-, 24-, and 36-month visits. The use of these screening tests is not appropriate in populations at risk; such patients require comprehensive assessment. The sensitivity and specificity of these instruments range from 0.70 to 0.90. The clinician’s judgment is required in interpretation of test results, particularly of measures that rely on parental report. Children who are developing normally may fail a screening test because of shyness, unfamiliarity with the examiner or the materials, or other factors unrelated to developmental competence. In most cases, a positive screen should be followed by a comprehensive assessment of development and should not be ignored. Screening tests can be used to confirm parental concerns but are not appropriate for diagnosing the nature of the problem. If parental concerns persist despite negative findings, a full evaluation is advisable because of the limited sensitivity of the tests and the importance of attending to parental concerns. To ensure that the performance is representative of the child’s ability, screening tests should be performed when the child is physically well, is familiar with the setting and with the examiner, and under minimal stress. Examples of familiar settings include the child’s home for infants, toddlers, and younger children; the child’s preschool becomes another familiar setting for children 3 years of age and older.
Gross Motor Development
Early Reflex Patterns (“Primitive Reflexes”)
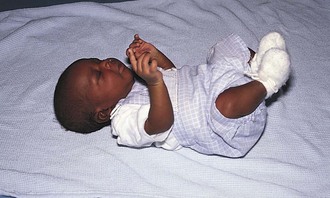
Perhaps the best known of these reflex patterns is the Moro response, or startle reflex. This reflex can occur spontaneously after a loud noise, but typically it is elicited during the course of physical examination by an abrupt extension of the infant’s neck. The response consists of symmetrical abduction and extension of the arms with extension of the trunk (Fig. 3-1) followed by adduction of the upper extremities, as in an embrace, and frequently is accompanied by crying (Fig. 3-2). The Moro reflex gradually disappears by 4 months of age, associated with the development of cortical functioning. In children up to 4 months of age, the Moro response can be used to evaluate the integrity of the central nervous system and to detect peripheral problems, such as congenital musculoskeletal abnormalities or neural plexus injuries; an asymmetrical response may indicate unilateral weakness.
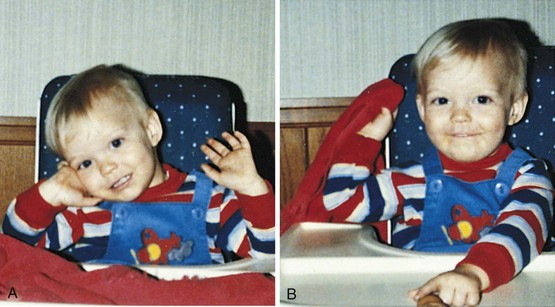
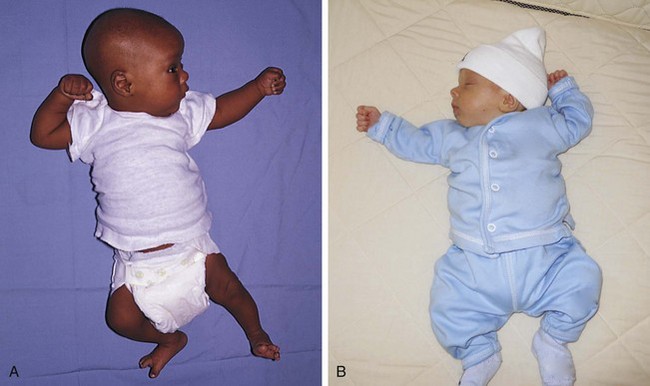
Another early reflex pattern is called the asymmetrical tonic neck reflex (ATNR) (Fig. 3-3, A and B). A newborn’s limb motions are strongly influenced by head position. If the head is directed to one side, either by passive turning or by inducing the baby to follow an object to that side, tone in the extensor muscles increases on that side and in the flexor muscles on the opposite side. This response may not be seen immediately after birth, when the newborn has high flexor tone throughout the body, but it usually appears by 2 to 4 weeks of age. The ATNR allows the baby to sight along the arm to the hand and is considered one of the first steps in the coordination of vision and reaching. This reflex disappears by 4 to 6 months of age, to allow for the development of voluntary reaching.
With the emergence of voluntary control from higher cortical centers, muscular flexion and extension become balanced. Primitive reflexes are replaced by reactions that allow children to maintain a stable posture, even if they are rapidly moved or jolted. A timetable listing the expected emergence and disappearance of primitive reflexes and the protective equilibrium responses is presented in Table 3-2.
Table 3-2 Primitive Reflexes and Protective Equilibrium Responses
| Reflex | Appearance* | Disappearance* |
|---|---|---|
| Moro | Birth | 4 mo |
| Hand grasp | Birth | 3 mo |
| Crossed adductor | Birth | 7 mo |
| Toe grasp | Birth | 8-15 mo |
| ATNR | 2 wk | 6 mo |
| Head righting | 4-6 mo | Persists voluntarily |
| Protective equilibrium | 4-6 mo | Persists voluntarily |
| Parachute | 8-9 mo | Persists voluntarily |
ATNR, asymmetrical tonic neck reflex.
* Different sources may vary on the precise timing of the appearance and disappearance of these primitive and equilibrium responses.
Antigravity Muscular Control
Head Control
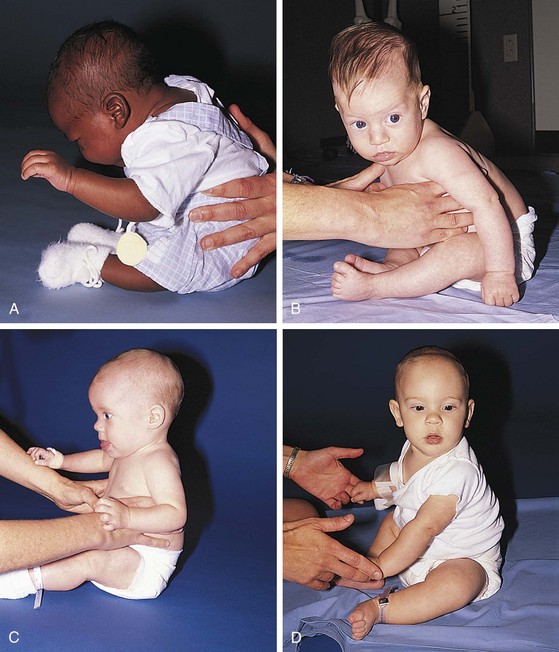
The infant’s earliest control task is to maintain a stable posture against the influence of gravity. Neck flexors allow head control against gravity when a child is pulled from the supine to the sitting position. Neonates show minimal control of the neck flexors, holding their heads upright only briefly when supported in a sitting position. When an infant is pulled to a sitting position, the head lags behind the arms and shoulders (Fig. 3-4, A). By 4 months of age the child is able to support his head, and his head moves along with his shoulders when he is pulled to a sitting position (Fig. 3-4, B). At 5 to 6 months of age the infant anticipates the direction of movement of the pull-to-sit maneuver and flexes the neck before the shoulders begin to lift (Fig. 3-4, C).
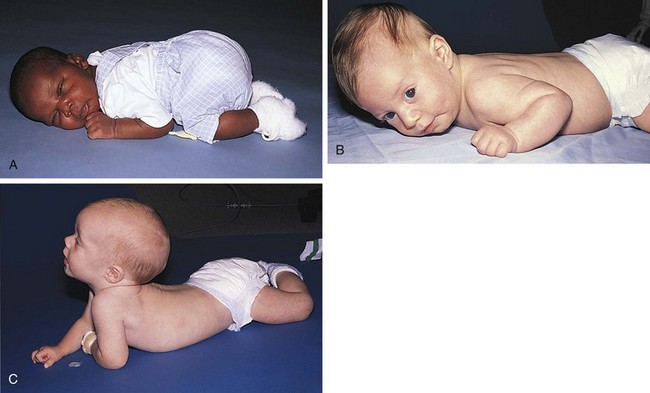
Trunk Control and Sitting
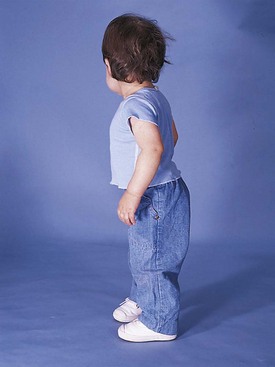
In the prone position a newborn remains in a tightly flexed position and can simply turn the face from side to side along the bed sheets. Progressive control of the shoulders and upper trunk in the first few months of life, plus a decrease in flexor tone, enables the young infant to hold the chest off the bed with the weight supported on the forearms by about 4 months (Fig. 3-5). Evolution of trunk control down the thoracic spine can also be observed with the infant in a sitting position (Fig. 3-6). As control reaches the lumbar area, the lumbar lordotic curve can be seen when the child is standing (Fig. 3-7).
Automatic Reactions: Equilibrium and Protective Reactions
Equilibrium and protective reactions are automatic, reflexive patterns that also emerge in a cephalocaudal sequence. Head righting refers to the infant’s ability to keep the head vertical despite a tilt of the body. A 4-month-old infant typically demonstrates this ability in vertical suspension when gently swayed from side to side. As control moves downward, protective equilibrium responses can be elicited in a sitting infant by abruptly but gently pushing the infant’s center of gravity past the midline in one of the horizontal planes. This is the lateral protective reaction, which involves increased trunk flexor tone toward the force and an outreached hand and limb away from the force; it usually emerges by 6 months of age, and is required for the development of stable, independent sitting (Fig. 3-8). At 10 months the child develops the forward protective or parachute reaction, an outstretching of both arms and legs when the body is abruptly moved head first in a downward direction (Fig. 3-9). The forward protective (parachute) reaction is a programmed reflex that protects the head if the child falls from standing or walking and is generally seen just before these motor skills develop.
Development of Locomotion
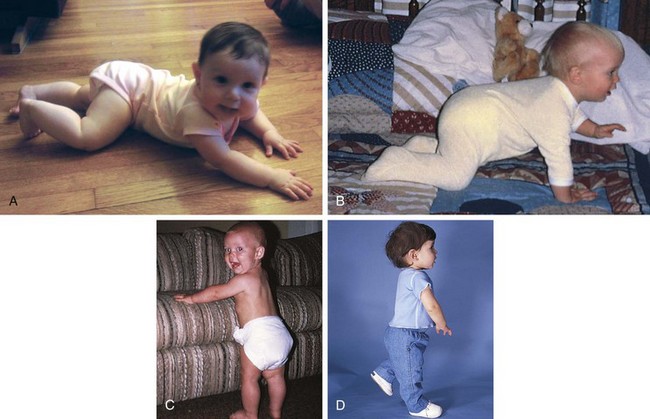
Gross motor milestones can also be described in terms of locomotion (Table 3-3). Prone-to-supine (front to back) rolling may be accomplished by 3 to 4 months of age, after the child gains sufficient control of shoulder and upper trunk musculature to prop up on the arms. Supine-to-prone (back to front) rolling requires control of the lumbar spine and hip region, as well as the upper trunk; this is usually present by 5 to 6 months of age. Since the introduction of Back to Sleep (recommended supine sleeping to prevent sudden infant death syndrome), prone-to-supine rolling may appear later, at 5 to 6 months, because the child has had little experience in the prone position; it may actually occur later than supine-to-prone rolling, demonstrating the impact of experience on gross motor skills. Creeping (also called commando or army crawling), accomplished at 5 to 6 months of age (Fig. 3-10, A), involves coordinated pulling with upper arms and passive dragging of the legs, akin to a soldier trying to keep the body low to the ground. By 6 to 9 months of age, as voluntary control moves to the hips and legs, the child is capable of getting up on the hands and knees, assuming a quadruped position, and crawling (Fig. 3-10, B). The next developmental milestone is supported standing. By 9 to 10 months of age, many children like to demonstrate this new skill by holding on to a parent or by walking independently while holding on to furniture. This is called cruising (Fig. 3-10, C). Increased control to the feet and disappearance of the plantar grasp reflex allow the child to walk independently. Walking three steps alone occurs at a median age of about 12 months, with a range of 9 to 17 months of age (Fig. 3-10, D).
Table 3-3 Early Gross Motor Milestones in the Normal Child
| Task | Age Range* |
|---|---|
| Sits alone momentarily | 4-8 mo |
| Rolls back to stomach | 4-10 mo |
| Sits steadily | 5-9 mo |
| Gets to sitting | 6-11 mo |
| Pulls to standing | 6-12 mo |
| Stands alone | 9-16 mo |
| Walks three steps alone | 9-17 mo |
* Wide ranges in the attainment of these gross motor milestones in healthy children are the rule rather than the exception.
From Bayley N: Bayley Scales of Infant Development, ed 2, San Antonio, Tex, 1993, Psychological Corporation/Harcourt Brace.
Gross Motor Assessment During Health Maintenance Visits
Evaluation of gross motor skills can begin when the pediatrician enters the office for a well-child visit. The typical 2-month-old infant is cradled in the parent’s arms; the 4-month-old has enough strength to support her back when held inside her arms by her father’s hands but not enough strength to sit on her own (Fig. 3-11); the 6-month-old child is sitting with minimal support on the parent’s lap or on the examination table next to the parent; the 12-month-old is cruising or toddling through the room. Although there is a wide age range in the onset and duration of each stage, the 6-month-old infant who lacks head control on the pull-to-sit maneuver, who cannot clear the table surface with the chest by supporting weight on the arms when prone, who shows no head righting, or who has persistent primitive reflexes such as a complete Moro response or ATNR is at sufficient variance from peers to warrant evaluation for a possible neuromuscular disorder. In addition, when gross motor delays are found in association with verbal and social delays, asymmetrical use of one limb or one side of the body, or loss of previously attained milestones, diagnostic evaluation is indicated.
At the discovery of delayed or atypical development, the pediatrician’s first task is to develop a differential diagnosis and a plan to establish the specific diagnosis. Potential causes of delayed gross motor development are listed in Table 3-4. Another equally important task is to recommend a treatment program. Early intervention programs and/or physical therapy should be actively considered for children with motor difficulties during infancy through preschool. Adaptive physical education programs are available for older children with mild problems that do not seriously impair function.
Table 3-4 Potential Causes of Delayed Gross Motor Development
| Global Developmental Delay | Motor Dysfunction | Motor Intact but Otherwise Restricted |
|---|---|---|
| Genetic syndromes and chromosomal abnormalities Brain morphologic abnormalities Endocrine deficiencies—hypothyroidism, prolonged hypoglycemia Congenital infections Neurodegenerative diseases Idiopathic intellectual disability | Central nervous system damage—kernicterus, birth injury, neonatal stroke, trauma, prolonged seizures, metabolic insult, infection | Congenital malformations—bony or soft tissue defects Diminished energy supply—chronic illness, severe malnutrition Environmental deprivation—casted, non–weight bearing Familial and genetic endowment—slower myelination Sensory deficits—blindness Temperamental effects—low activity level, slow to try new tasks Trauma—child abuse |
| Spinal cord dysfunction—Werdnig-Hoffmann disease, myelomeningocele, polio | ||
| Peripheral nerve dysfunction—brachial plexus injury, heritable neuropathies | ||
| Motor end-plate dysfunction—myasthenia gravis | ||
| Muscular disorders—muscular dystrophies | ||
| Other—benign congenital hypotonia |
Fine Motor Development
Involuntary Grasp
At birth the neonate’s fingers and thumb are typically tightly fisted. A newborn grasps reliably and reflexively at any object placed in the palm (Fig. 3-12) and cannot release the grasp. Because of this reflex, the newborn’s range of upper extremity motion is functionally limited. Normal development leads to acquisition of a voluntary grasp.
Voluntary Grasp
The reflexive palmar grasp gradually disappears at about 1 month of age. From that point, the infant gains control of fine motor skills in an orderly progression. In the second or third month of life, the infant initially brings both hands together for midline hand play (Fig. 3-13). Shortly after that, the baby begins to swipe at objects held in or near the midline (Fig. 3-14). It is through swiping that the infant increases the exploratory range and fine-tunes the small muscles of the wrist, hand, and fingers.
Next, the child develops the ability to bend the fingers against the palm (palmar grasp), squeeze objects, and obtain them independently for closer inspection. Differentiation of the parts of the hand develops in association with differentiation of the two hands. Between 5 and 7 months of age, the infant can use hands independently to transfer objects across the midline. Further differentiation of the plane of movement of the thumb allows it to adduct as the fingers squeeze against the palm in a radial palmar or whole-hand grasp. With time, the thumb moves from adduction to opposition. The site of pressure of the thumb against the fingers moves away from the palm and toward the fingertips, in what is called an inferior pincer or radial digital grasp, seen around 9 months of age (Fig. 3-15). By 10 months of age, differentiated use of the fingers allows the child to explore the details of an object.
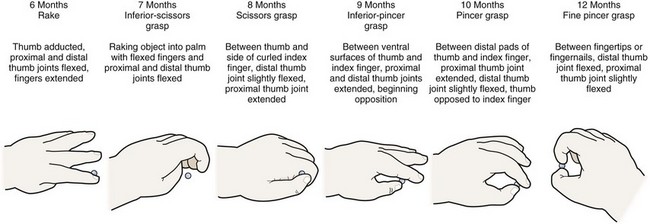
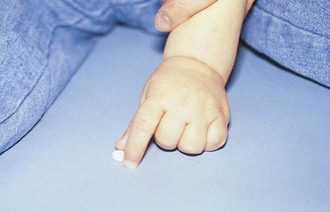
Figure 3-15 Development of prehension.
(Modified from Erhardt RP: Developmental hand dysfunction: theory, assessment, treatment, ed 2, San Antonio, Tex, The Psychological Corporation, 1994.
Between 9 and 12 months of age, the fine pincer grasp develops, allowing opposition of the tip of the thumb and the index finger (see Fig. 3-15). This milestone enables the precise prehension of tiny objects (Fig. 3-16). The infant uses this skill in tasks such as self-feeding and exploration of small objects. By 1 year, the infant can position the hand in space to achieve vertical or horizontal orientation before grasping or releasing an object.
Development of Complex Fine Motor Skills
Early in the second year of life the young child uses the grasp to master tools and to manipulate objects in new ways. Dropping and throwing, stacking, and putting objects in and out of receptacles become favorite pastimes. Mastery of the cup and spoon supplement or replace finger feeding as a more efficient and less messy means of eating (Fig. 3-17).

Figure 3-17 Independent feeding. A 15-month-old child employs fine motor skills to use a spoon independently.
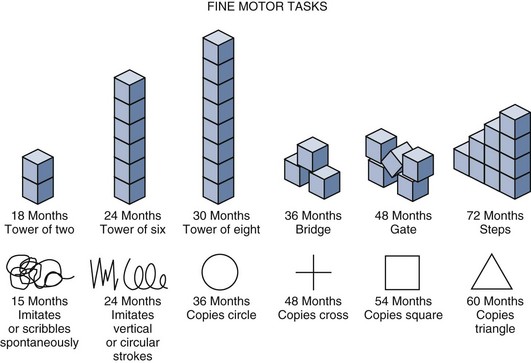
Advancements in fine motor planning and control can be demonstrated through the child’s ability to stack small cubes. After children master stacking, they show consistent patterns of improvement in reproducing structures that they have watched the examiner assemble (Fig. 3-18). The child’s ability to copy a variety of drawings also improves during this period.
Fine Motor Evaluation and Testing
Fine motor activities can be engaging and nonthreatening to the preschool and school-age child; these activities allow the physician to make valuable observations and to establish rapport. The physician can routinely request that the child use the waiting time or the period of history-taking to draw a self-portrait. These drawings provide a wealth of information not only on the child’s capacities for fine motor control but also on cognitive development and social and emotional functioning. A quick method for analyzing the age level of a drawing is to count the number of features in the drawing. The child receives one point for each of the following features: two eyes, two ears, a nose, a mouth, hair, two arms, two legs, two hands, two feet, a neck, and a trunk. Each point converts to the value of  year added to a base age of 3 (Fig. 3-19). Screening tests and standardized measures, such as the Beery-Buktenica Developmental Test of Visual–Motor Integration, fifth edition, can also be used to assess fine motor skills.
year added to a base age of 3 (Fig. 3-19). Screening tests and standardized measures, such as the Beery-Buktenica Developmental Test of Visual–Motor Integration, fifth edition, can also be used to assess fine motor skills.
Children with brain damage are at particular risk for problems with perceptual–fine motor integration, even in the absence of visual problems and with minimal involvement of the upper extremities (Fig. 3-20).
Cognitive Development
Early Sensory Processing
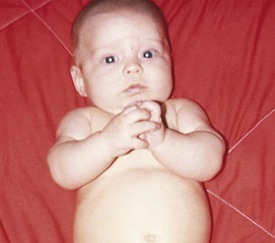
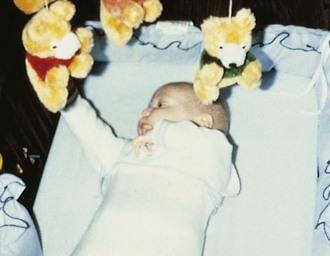
The visual acuity of the full-term infant is estimated to fall between 20/200 and 20/400 and improves rapidly over the first year of life. Even at birth, it is possible to get the full-term newborn to fix on faces 9 to 12 inches from the face and to track objects horizontally at least 30 degrees (Fig. 3-21). Some neonates, if assessed when calm and fully alert, can track objects 180 degrees across the visual field. Newborns also respond to sound, typically quieting in response to a human voice, rattles, or music. In the first days of life, many infants turn to the source of sound and search for it with their eyes. These maneuvers, found on the Brazelton Neonatal Behavioral Assessment Scale, are useful in demonstrating neurobehavioral characteristics of newborns.

Figure 3-21 Early social skills. A newborn within an hour of birth fixates on the face of the mother.
Development of Sensorimotor Intelligence
Early progress in the development of object permanence is indicated by the infant’s continued though brief gaze at the site where a familiar toy or face has disappeared. At this point, children also repeat actions that they have discovered will produce interesting results. Between 4 and 8 months of age, infants become interested in changes in the position and appearance of toys. They can track an object visually through a vertical fall (Fig. 3-22) and search for a partially hidden toy. They also begin to vary the means of creating interesting effects. In these early months the baby’s play consists of exploring toys to gain information about their physical characteristics. Activities such as mouthing, shaking, and banging can provide sensory input about an object beyond its visual features. However, when mouthing of toys persists as the predominant mode of exploration after 12 to 18 months of age, assessment of cognitive function is warranted.
At approximately 9 to 12 months of age, infants can locate objects that have been completely hidden (Fig. 3-23). Not surprisingly, peek-a-boo becomes a favorite pastime at this point. Later, the infant can crawl away from the mother and recall where to return to find her.
By 18 months of age, children can deduce the location of an object even if they have not seen it hidden from view. They can maintain mental images of desired objects and develop plans for obtaining them. The child’s understanding of causality also advances; cause-and-effect relationships no longer need to be direct to be appreciated (Fig. 3-24). These developments herald the beginning of a new stage in cognitive development, that of symbolic thinking. They also indicate that distraction may not succeed in drawing a child away from a desired object; a direct request is required.
Development of Logical Thinking
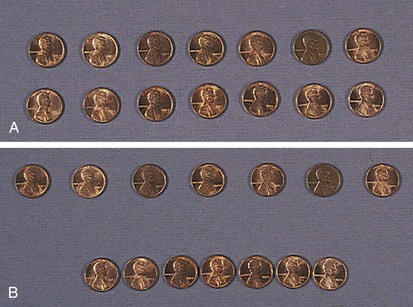
The logic of the preschooler is in large part influenced by the appearance of objects. Because an airplane appears to become smaller as it takes off, the preschooler may assume that all the people on the plane become smaller as well. Piaget demonstrated that preschoolers seem to think that number and quantity vary with appearance (Fig. 3-25). Under certain circumstances a 4-year-old child may show understanding that a quantity remains invariant unless something is added or subtracted. That same child, however, may insist that two rows of pennies are different in number simply because of a compelling visual difference between them.
The immature logic of the preschooler is gradually replaced by conventional logic and wisdom. School-age children follow logic akin to adult reasoning, at least when the stimuli are concrete. Faced with the same question about the pennies, they readily acknowledge that the two rows have the same number regardless of their visual appearance (see Fig. 3-25). They also know that the airplane just looks smaller because it has moved farther from the viewer, and they giggle at the suggestion that the people on the plane have shrunk. Their logical limitations become obvious when they must reason about the hypothetical or the abstract.
Assessing Cognitive Development
For the parents, a delay in a child’s attainment of a well-known milestone may create tremendous fear about ultimate learning potential. In many cases, such parental concerns are put to rest at that time when the physician determines that the child’s learning to date is age-appropriate. If a child does show delays in cognitive development, the physician should generate a differential diagnosis (Table 3-5) from knowledge of the child’s level of functioning in multiple domains, history, and physical examination.
Table 3-5 Potentially Remediable Disorders Associated with Developmental Delay
| Findings Sometimes Present on History or Examination | Possible Disorder |
|---|---|
| Decreased vision or hearing | Specific sensory deficits |
| Staring spells, motor automatism | Seizure disorders |
| Lethargy, ataxia | Overmedication with anticonvulsants |
| Myxedema, delayed return on DTRs, thick skin and tongue, sparse hair, constipation, increased sleep, coarse voice, short stature, goiter | Hypothyroidism |
| Irritability, cold sweats, tremor, loss of consciousness | Hypoglycemia |
| Unexplained bruises in various stages, failure to thrive | Child abuse and neglect |
| Short stature, weight below third percentile | Malnutrition or systemic illness producing failure to thrive |
| Poor purposeful attending in multiple settings | ADHD |
| No specific findings | Environmental deprivation |
| Anemia | Iron deficiency or lead exposure |
| Absent venous pulsations or papilledema on funduscopic examination, morning vomiting, headaches, brisk DTRs in lower extremities | Increased intracranial pressure |
| Vomiting, irritability and seizures, failure to thrive | Some inborn errors of metabolism (e.g., methylmalonic acidemia) |
| Hepatomegaly, jaundice, hypotonia, susceptibility to infection, cataracts | Galactosemia |
| Fair hair, blue eyes, “mousy” odor to urine | Phenylketonuria |
| Ongoing evidence of active or progressive disease | Chronic infection, inflammatory disease, malignancies |
ADHD, attention-deficit/hyperactivity disorder; DTR, deep tendon reflex.
If children with sensory or motor impairments are tested with instruments normalized on able-bodied children, they often obtain low scores. Different assessment techniques have been devised to circumvent specific disabilities while obtaining information about a child’s cognitive abilities; these are typically administered by psychologists, child development specialists, or special educators (Table 3-6).
Table 3-6 Tests Used in the Assessment of Cognitive Development
| Type of Scale | Test(s) Used | Age Range |
|---|---|---|
| Standard intelligence scales | Stanford-Binet Intelligence Scales-IV | 2-adult |
| Wechsler Intelligence Scale for Children-IV | 6-16 yr | |
| Nonverbal intelligence scale | Leiter International Performance Scale-R | 2-18 yr |
| Infant development tests | Bayley Scales of Infant Development-III | 0- yr yr |
| Gesell Developmental Schedules | 0-5 yr | |
| Developmental scale for the visually impaired | Reynell-Zinkin Developmental Scales for Young Children with Visual Impairments | 0-5 yr |
| Adaptive behavior | Vineland Adaptive Behavior Scales-II | 0-18 yr |
| Adaptive Behavior Assessment System-II | 0-21 yr |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






 months the child walks well, and by 36 months he or she can balance on one foot for 1 second. Most children can hop by age 4. They can throw a ball overhand by
months the child walks well, and by 36 months he or she can balance on one foot for 1 second. Most children can hop by age 4. They can throw a ball overhand by  months, but catching develops later, at almost 5 years.
months, but catching develops later, at almost 5 years.

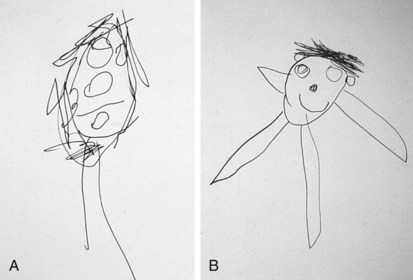
 year for each of the five features, added to a base age of 3 years. This drawing has an age equivalent of
year for each of the five features, added to a base age of 3 years. This drawing has an age equivalent of  years. B, A drawing by the same child at age 5 years. Note the inclusion of ears and arms, as well as improvements in proportion. This drawing has an age equivalent of
years. B, A drawing by the same child at age 5 years. Note the inclusion of ears and arms, as well as improvements in proportion. This drawing has an age equivalent of  years.
years.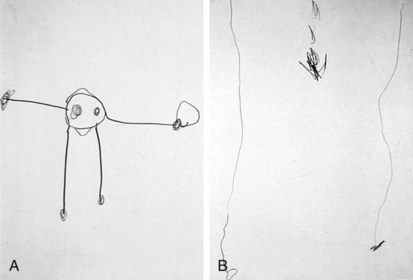
 years. B, Drawing by a 4-year-old child with spastic diplegia. Difficulties in organization appear related to visuomotor integration skills rather than to problems with fine motor skills.
years. B, Drawing by a 4-year-old child with spastic diplegia. Difficulties in organization appear related to visuomotor integration skills rather than to problems with fine motor skills.