Dermatologic Diseases
Kara Sternhell-Blackwell
Monique Gupta Kumar
Susan J. Bayliss
Skin disorders are one of the most common problems in pediatrics.
Never underestimate parental concerns about their child’s skin. Unlike many disease processes, the skin is visible and noticeable to parents and others.
Examination of the skin requires observation and palpation of the entire skin surface under good light. Do not forget to look at the eyes and mouth for mucous membrane involvement.
Examination should include onset, duration, and inspection of a primary lesion. It is also important to note secondary changes, morphology, and distribution of the lesions.
NEONATAL DERMATOSES
Cutis Marmorata
Transient, blanchable, reticulated mottling occurs on the skin exposed to a cool environment.
No treatment is necessary; the condition generally resolves by 1 year of age.
If it persists, consider hypothyroidism, heart disease, or other associated abnormalities.
Erythema Toxicum Neonatorum
Scattered erythematous papules and pustules may occur anywhere on the body (Fig. 15-1).
This self-limited condition generally appears in the 1st week of life and resolves within 1 month.
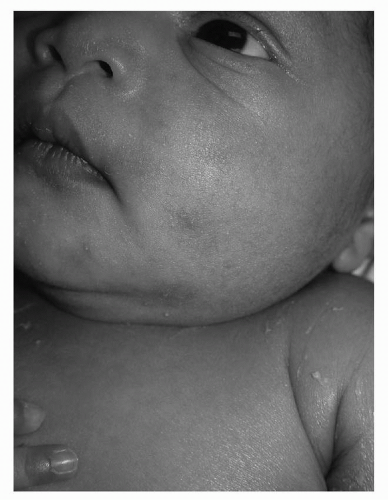
Transient Neonatal Pustular Melanosis
Pustular lesions rupture easily and leave hyperpigmented macules on the neck, chin, forehead, lower back, and shins (Fig.15-2).
Almost always present at birth, this condition is more common in dark-skinned infants.
It is self-limited. Pustules resolve within days, but hyperpigmentation may take months to resolve.
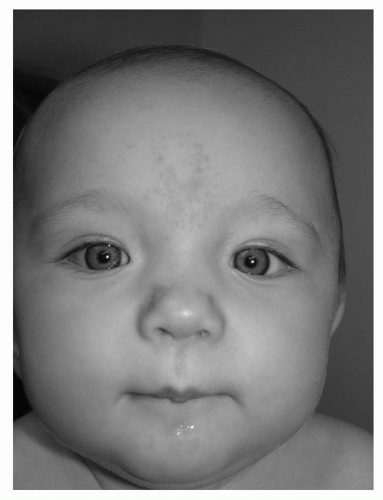
Acne Neonatorum
Comedones, pustules, and papules on the face resemble acne vulgaris (Fig.15-3).
It generally develops at 2-3 weeks of age and resolves within 6 months.
No treatment is usually necessary; wash face with baby soap. In severe cases, referral to a pediatric dermatologist may be warranted.
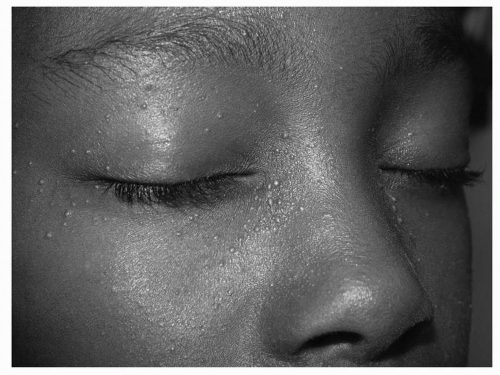
Milia
These 1-2 mm pearly white papules are found most commonly on the face (Fig. 15-4) but may occur anywhere. On the palate, they are known as “Epstein pearls.”
They may be present at birth.
They usually resolve without treatment by 2-6 months of age.
Miliaria
This “heat rash” is due to sweat retention when the sweat glands are plugged. It is worsened by heat and humidity.
Miliaria crystallina are 1-2 mm vesicles without erythema in intertriginous areas, neck, and chest.
Miliaria rubra are erythematous papules in the same distribution that result from obstruction deeper in the epidermis.
This condition resolves without treatment in a dry environment.
Harlequin Color Change
This transient erythematous flush occurs on the dependent half of the body when the infant is placed on his or her side.
This self-limited condition generally resolves within minutes but may recur.
Subcutaneous Fat Necrosis
Erythematous subcutaneous nodules and plaques that may be fluctuant.
They appear at 1-6 weeks of life and generally resolve without treatment in 2-6 months. Fluctuant nodules require drainage.
They may be associated with significant hypercalcemia as well as localized calcification. Infants should be monitored for hypercalcemia for at least 6 months after appearance of extensive lesions.
BIRTH MARKS
Mongolian Spots (Dermal Melanosis)
These blue-gray poorly circumscribed macules often occur in lumbosacral area or lower extremities (Fig. 15-5).
More common in pigmented skin, they are present from birth.
Lumbosacral lesions tend to fade during childhood; however, lesions in other locations usually persist.
Café-au-Lait Macules
These light brown macules (Fig. 15-6) can occur anywhere on the body.
They may occur in isolation or in association with a syndrome.
The presence of six or more macules >0.5 cm in diameter in prepubertal children or >1.5 cm in postpubertal, as well as inguinal or axillary freckling, is suggestive of neurofibromatosis 1.
Large, irregular truncal patches may be associated with McCune-Albright syndrome.
Congenital Melanocytic Nevi
These brown pigmented macules or plaques may have dark brown or black papules or other irregular pigmentation within the lesions (Fig. 15-7). They may cover large areas of skin.
Lesions are present at birth; small congenital melanocytic nevi may become more noticeable within the 1st year of life.
The small increased risk of melanoma development within lesions makes close follow-up important.
Decisions about excision versus observation vary with the size and site of the lesion.
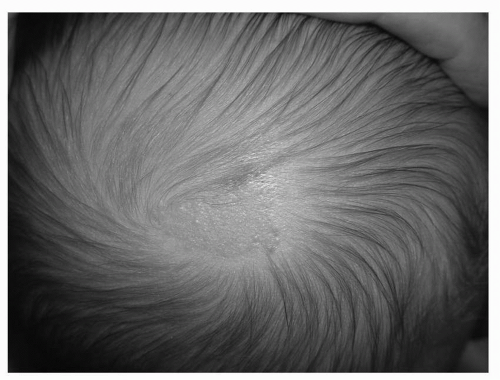
Nevus sebaceous
This hairless, yellow-colored plaque tends to have an irregular surface.
Located on the scalp (Fig. 15-8), it becomes less prominent after the newborn period but later grows and becomes more papular or verrucous around puberty, when hormone levels increase.
Treatment is surgical excision or observation.
Surgery is often deferred until puberty when the lesion begins to grow.
The plaque should be followed by clinical observation until excision because there is a low, but increased, risk of benign tumors within the lesion.
Aplasia Cutis Congenita
This is an absence of skin with scar formation in a localized area, most commonly on the scalp (Fig. 15-9).
Defects are present from birth.
Larger or multiple lesions may be associated with other congenital anomalies or a genetic syndrome.
Small defects often heal on their own, leaving scar tissue. Larger defects may require skin grafting or other surgical intervention.
Port Wine stain
This pink, red, or purple blanchable macule is caused by capillary malformations (Fig. 15-10). This is due to a somatic mutation in GNAQ.
Lesions in cranial nerve V1 (+/- V2) distribution on the face should be evaluated for associated glaucoma and/or Sturge-Weber syndrome. These lesions persist and generally become darker and thicker with age.
Therapy is pulsed-dye laser treatment.
Salmon Patch/Nevus simplex (“stork Bite”)
These are pink macular patches (Fig. 15-11), generally on the eyelids, glabella, or nape of neck.
Lesions on the eyelids usually improve at 1 year and fade by 3 years.
Lesions on the nape of the neck tend to persist.
Hemangiomas
Appearance
Superficial: bright red vascular plaques or nodules
Deep: bluish purple nodules, sometimes with overlying telangiectatic markings (Fig. 15-12)