Chapter 593 Demyelinating Disorders of the CNS
Demyelinating disorders of the central nervous system (CNS) cause acute or relapsing-remitting encephalopathy and other multifocal signs of brain, brainstem, and spinal cord dysfunction. They affect white matter, which is formed by myelin contained within oligodendrocytes, providing electrical insulation for neurons and neuronal connections. In contrast to genetically determined leukodystrophies (sometimes called dysmyelinating disorders) that also produce disrupted white matter, demyelinating disorders generally target normally formed white matter through immune-mediated mechanisms. Major demyelinating disorders in childhood include multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM). The rare macrophage activating syndromes and isolated angiitis of the CNS can sometimes be confused with ADEM (Table 593-1).
Table 593-1 SUMMARY OF CONSENSUS DEFINITIONS FOR PEDIATRIC CENTRAL NERVOUS SYSTEM INFLAMMATORY DEMYELINATION
| MONOPHASIC CNS INFLAMMATORY DEMYELINATION | |
| ADEM | Clinical event must include encephalopathy (behavioral change and/or altered consciousness) |
| New symptoms or signs within 3 months are considered part of same ADEM event | |
| CIS | Clinical event that can be monofocal (e.g., isolated optic neuritis) or polyfocal, but cannot include encephalopathy |
| NMO | Must have optic neuritis and transverse myelitis as major criteria. Must have spinal MRI lesion extending over 3 or more segments or be NMO-IgG positive |
| RELAPSING CNS INFLAMMATORY DEMYELINATION | |
| Recurrent ADEM | New event of ADEM (must have encephalopathy) with recurrence of initial ADEM symptoms and signs 3 or more months after initial event and not related to withdrawal of steroids |
| Multiphasic ADEM | ADEM followed by new clinical event also meeting criteria for ADEM, but involving new CNS lesions (clinically and radiologically) |
| Relapsing NMO | Relapse of NMO as described above. Additional clinical and radiologic features extrinsic to optic nerve and spinal cord are well described and acceptable for diagnosis |
| Pediatric MS | Two or more events separated in time (4 or more weeks) and space. First episode cannot be ADEM. If 1st episode is ADEM, 2 or more non-ADEM events are required for diagnosis of MS. New MRI lesions 3 months or longer after the initial clinical event can be used to satisfy criteria for dissemination in time |
All events must include compatible MRI features of CNS inflammatory demyelination and exclude alternative causes.
ADEM, acute disseminated encephalomyelitis; CIS, clinically isolated syndrome; CNS, central nervous system; MS, multiple sclerosis; NMO, neuromyelitis optica.
(Data from Krupp LB, Banwell B, Tenembaum S: Consensus definitions proposed for pediatric multiple sclerosis and related disorders, Neurology 68[16 Suppl 2]:S7–S12, 2007.)
593.1 Multiple Sclerosis
Clinical Manifestations
Presenting symptoms in pediatric MS include hemiparesis or paraparesis, unilateral or bilateral optic neuritis, focal sensory loss, ataxia, diplopia, dysarthria, or bowel/bladder dysfunction (Table 593-2). Polyregional symptoms are reported in 30% of patients. Encephalopathy is less common and suggests consideration of acute disseminated encephalomyelitis (ADEM).
Table 593-2 SYMPTOMS AND SIGNS OF MULTIPLE SCLEROSIS BY SITE
| SYMPTOMS | SIGNS | |
|---|---|---|
| Cerebrum | Cognitive impairment | Deficits in attention, reasoning, and executive function (early); dementia (late) |
| Hemisensory and motor | Upper motor neuron signs | |
| Affective (mainly depression) | ||
| Epilepsy (rare) | ||
| Focal cortical deficits (rare) | ||
| Optic nerve | Unilateral painful loss of vision | Scotoma, reduced visual acuity, color vision, and relative afferent papillary defect |
| Cerebellum and cerebellar pathways | Tremor | Postural and action tremor, dysarthria |
| Clumsiness and poor balance | Limb incoordination and gait ataxia | |
| Brainstem | Diplopia, oscillopsia | Nystagmus, internuclear and other complex ophthalmoplegias |
| Vertigo | ||
| Impaired swallowing | Dysarthria | |
| Impaired speech and emotional lability | Pseudobulbar palsy | |
| Paroxysmal symptoms | ||
| Spinal cord | Weakness | Upper motor neuron signs |
| Stiffness and painful spasms | Spasticity | |
| Bladder dysfunction | ||
| Erectile impotence | ||
| Constipation | ||
| Other | Pain | |
| Fatigue | ||
| Temperature sensitivity and exercise intolerance |
Modified from Compston A, Coles A: Multiple sclerosis, Lancet 372:1502–1517, 2008, p 1503.
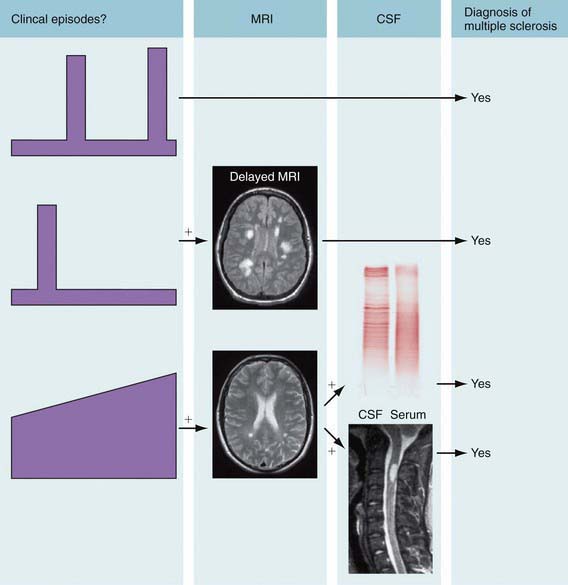
Laboratory Findings
Cranial MRI exhibits discrete T2 lesions in cerebral white matter, particularly periventricular regions as well as brainstem, cerebellum, and juxtacortical and deep gray matter. Alternatively, tumefactive T2 lesions are also seen. Spine MRI typically shows partial-width cord lesions restricted to 1-2 spine segments. CSF may be normal or exhibit mild pleocytosis, particularly in younger children. Abnormal MS profiles (increased IgG index, and/or CSF oligoclonal bands) increase likelihood of MS but may be negative in 10-60% of pediatric MS patients, particularly prepubertal children (Fig. 593-1). Abnormal evoked potential studies can localize disruptions in visual, auditory, or somatosensory pathways.