Gary D. V. Hankins, MD
George R. Saade, MD
MASSIVE AND SUBMASSIVE PULMONARY EMBOLISM
INTRODUCTION
Pregnancy is a hypercoagulable state secondary to blood stasis in the lower extremities, increased liver production of clotting factors, decreased fibrinolysis, and endothelial injury mostly at the time of delivery.1 The risk of deep venous thrombosis (DVT) and pulmonary embolism (PE) is five to six times higher than the nonpregnant population. Thromboembolic disease constitutes the most common cause of maternal mortality in developed nations.1 The risk of developing a thromboembolic complication is highest during the postpartum period. Particularly, the risk for PE is most pronounced in the postpartum.
CLINICAL PRESENTATION
The clinical presentation of DVT and PE during pregnancy is essentially the same as outside pregnancy. Importantly, many physiological symptoms of pregnancy resemble the clinical presentation of these conditions including physiologic dyspnea of pregnancy and bilateral leg swelling. The astute clinician should individualize each case presentation and decide based on the preclinical probability if further workup is needed. The vast majority of DVT cases during pregnancy (up to 80%) affect the left lower extremity secondary to decreased venous return as the result of compression of the right iliac artery over the left iliac vein as the latter crosses to drain into the inferior vena cava (similar pathophysiology as that seen in the May Thurner Syndrome).2
DVT is characterized by unilateral swelling of the affected extremity and pain. Pain may be elicited by flexion of the foot (Homan’s sign) and palpation of the calf muscles (Pratt sign). PE is characterized by a sudden onset of chest pain and shortness of breath. In addition, patients may present with tachypnea with resultant respiratory alkalosis, tachycardia, and rarely with hypotension and hemodynamic instability due to acute right ventricular failure. The latter leads to acute right ventricular dilation with leftward displacement of the interventricular septum resulting in obliteration of the left ventricular cavity and consequently impaired cardiac output and hemodynamic shock. The acute dilation of the right ventricle compresses the ventricular wall with coronary compression increasing also the risk of an acute right ventricular infarct. The latter two mechanisms explain the hemodynamic compromise seen in cases of massive PE. Hypoxemia may also be present but normal oxygenation does not rule out the possibility of a PE.
DIAGNOSIS
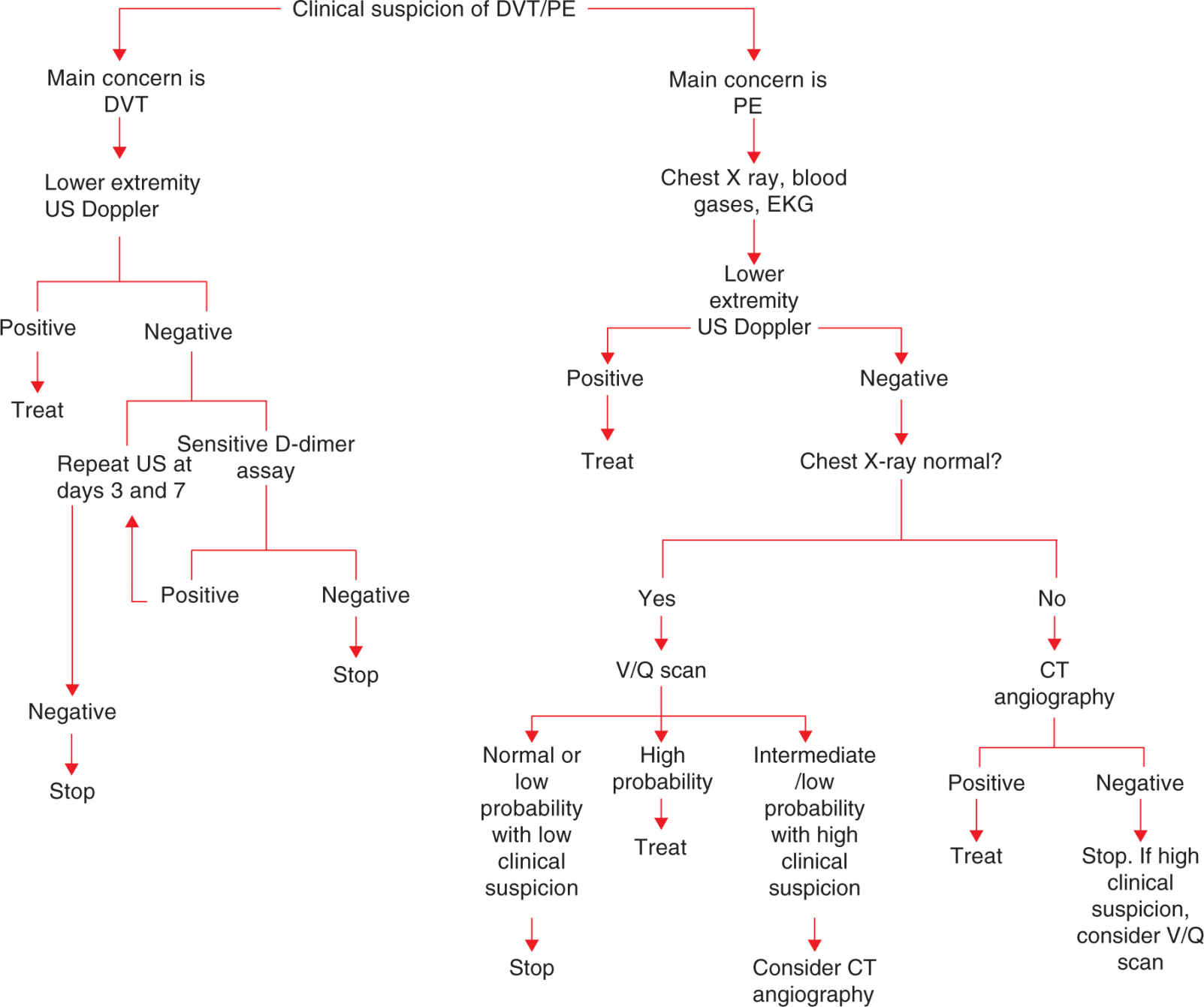
Clinical suspicion of DVT or PE must be confirmed with imaging studies. When suspicion exists for a DVT in the lower extremities, ultrasound Doppler is the initial test of choice. If the initial ultrasound is negative, serial further imaging at days 3 and 7 is recommended. Alternatively, the use of a sensitive D-dimer assay may be considered. If the assay is negative, no further workup is required. If the assay is positive, repeat imaging at days 3 and 7 is recommended.3 Elevated levels of D-dimer are physiologic during pregnancy and should not by themselves trigger extensive diagnostic workups.4 However, a negative D-dimer during pregnancy has a high negative predictive value to rule out DVT in the presence of a negative ultrasound study.
Importantly, during pregnancy, there is a higher prevalence of venous clots limited to the pelvic vessels (eg, iliac veins) that may not be visualized by ultrasound imaging of the venous system of the lower extremities. The latter is sometimes suspected by the presence of sluggish blood flow in the femoral veins. If the clinical suspicion is high, usually with swelling of the entire leg associated with flank and back pain, the diagnosis of an isolated pelvic clot may be accomplished with magnetic resonance venography.2
Diagnosis of PE during pregnancy is slightly different as compared with nonpregnant individuals. The initial workup should always include arterial blood gases, electrocardiograph, and a chest x ray. D-dimer assays (normally elevated during pregnancy) are not recommended to rule out PE. Regardless of the pretest probability, clinical suspicion of PE should be evaluated with imaging studies. In order to avoid radiation exposure, it is reasonable to initially perform lower extremity ultrasound Doppler studies. If a clot is found with clinical symptoms of PE, the diagnosis is confirmed and no further imaging will be required. If the ultrasound of the lower extremities is normal, chest imaging is required. The latter may be accomplished with either a ventilation/perfusion scan (V/Q scan) or a computed tomography angiography (CT angiography). The result of the initial chest x-ray is important in deciding which study to select. In the presence of a baseline abnormal chest x-ray, CT angiography should be used, as most V/Q scans will be nondiagnostic in this setting. If the chest x-ray is normal, a V/Q scan should be ordered if available as it will result in more diagnostic tests compared with CT angiography.5 The V/Q scan has the advantage of limiting maternal exposure to ionizing radiation (recent concern has developed in terms of increased risk of both breast and lung cancer among young women exposed to CT angiography). Fetal radiation exposure with a V/Q scan is minimal (50 mrads). Similarly, fetal exposure with CT angiography is equal or less compared with a V/Q scan.6
In order to limit radiation exposure, a perfusion scan (without the inhaled Xe-133) is acceptable. One study reported a 100% diagnostic yield using perfusion only scintigraphy.7 If the V/Q scan is normal or high probability, the diagnosis is either ruled out or in, respectively. In cases of a low or intermediate probability result, if the clinical suspicion is high, further imaging with a CT angiography may be indicated.
CT angiography is highly specific; the sensitivity is close to 80% to 85%. If the CT angiography result is negative in the presence of a high clinical suspicion, further imaging with a V/Q scan may be indicated (lower extremity ultrasound should have been done previously as discussed above).
An advantage of CT is that it may provide information of alternative diagnosis such as pleural effusions, lung parenchymal consolidations, and allows direct visualization of the right ventricular size (acute dilation may identify some of the patients with a higher probability of poor outcomes). Timing of contrast injection during pregnancy may limit the utility of CT angiography. Recent evidence has showed that up to 35% of CT angiographies during pregnancy may be nondiagnostic due to inadequate timing of contrast injection with subsequent poor vascular imaging.8 The latter may be secondary to the increased inferior vena cava pressure that occurs during pregnancy which coupled with the increased negative pressure in the chest during inspiration leading to shorter contrast material arrival time and subsequent artifacts. The increased cardiac output during pregnancy is also expected to contribute to the faster arrival of contrast media to the pulmonary vessels. Alternatively, the increased blood volume likely results in dilution of the contrast media.9 Despite theoretical concerns with the use of iodinated contrast media in CT, a case series of 344 newborns exposed to iodinated contrast media in utero reported no cases of thyroid dysfunction.10 Figure 30-1 summarizes the diagnostic work up in cases of suspected DVT and PE.
FIGURE 30-1. Diagnosis of deep venous thrombosis (DVT) and pulmonary embolism (PE) during pregnancy.
TREATMENT
When clinical suspicion is high, anticoagulation should be started immediately before imaging studying is performed, as the risk of sudden death may be high. Therapeutic anticoagulation during pregnancy is most commonly started with either unfractionated heparin (UFH) or low molecular heparin (LMWH). Current guidelines recommend LMWH as the first option for both prophylaxis and treatment during pregnancy.11 UFH has a half-life of 60 to 90 minutes and after intravenous administration the effect lasts for 4 to 6 hours. Intravenous dosing consists of an initial bolus of 80 units/kg followed by a continuous infusion of 18 units/kg/h.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree