One of the most difficult challenges in obstetrics is to ensure appropriate timing of delivery of the fetus. During labor, unnecessary operative interventions may cause maternal harm whereas delayed interventions may cause fetal or neonatal death or permanent central nervous system (CNS) injury. Labor exposes the fetus to varying degrees of stress from interruptions in blood supply due to uterine contractions, umbilical cord compression, head compression, placental abruption, or rupture of fetal vessels. Electronic fetal monitoring (EFM) was introduced in the 1960s, as a means of intrapartum fetal surveillance, in hopes of early detection and timely delivery of fetuses with inadequate reserve to tolerate the stress of labor. Since most fetal asphyxia cases occur in low-risk pregnancies, it was natural for the use of EFM to become widespread–being utilized in 85% of pregnancies. Unfortunately, years later there is still controversy about its fetal benefits despite the associated increased rates of cesarean and operative vaginal deliveries. One of the shortcomings of EFM has been the high interobserver and intraobserver variabilities in the interpretation and management of the various fetal heart rate (FHR) patterns. This can foster the impression that FHR tracing interpretation is somewhat subjective, which is problematic when trying to make decisions about labor management based on signs of fetal deterioration. The use of computerized or color-coded FHR classification systems could be helpful, but they have not been studied enough and are not widely available.
Due to the aforementioned challenges, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, American Congress of Obstetricians and Gynecologists (ACOG), and Society for Maternal-Fetal Medicine held a workshop in April 2008 to provide an update on FHR definitions, interpretation, and research guidelines. The workshop recommended standard definitions for FHR patterns and proposed a new 3-tier classification system for interpretation and management of FHR patterns. Based on the ability to predict fetal acid-base status at the time, the FHR patterns were classified as category I (normal), II (indeterminate), or III (abnormal). The workshop specifically recognized that FHR tracing categories “can and will change” since labor is a dynamic process. One of the recommended areas for research was observational studies focused on change of FHR patterns “over time.” Unfortunately, very little research has been published focusing on the longitudinal (over time) FHR assessment during labor. Instead, studies have focused on the static cross-sectional evaluations of FHR tracings of limited duration just prior to delivery.
The ACOG recommends that in low-risk patients, the FHR tracing should be evaluated by nurses or physicians, every 30 minutes in the first stage of labor and every 15 minutes during the second stage of labor. However, no instructions or recommendations are provided regarding over time (longitudinal) FHR assessment including more than just the last 15 or 30 minutes. In a recent poll (unpublished data, A.M.V.) taken among labor and delivery nurses, it was found that most nurses will evaluate the last 15-30 minutes, as per ACOG guideline, and they rarely go back to evaluate the FHR tracing in its entirety. Not surprisingly, there often is a predictable change in the FHR pattern as the fetus deteriorates over time from category I to category II or III, which will be missed unless the entire FHR tracing from admission is evaluated instead of the last few minutes. Category II tracings, which are the most frequent seen in >80% of laboring women, are quite variable in their significance and can include FHR patterns from the most benign to the most threatening. In such cases, a static evaluation of only the last 15-30 minutes may miss earlier transitional FHR changes of a deteriorating fetus. This editorial argues in favor of using the longitudinal assessment of FHR changes during labor to emphasize the point that in many cases, especially in the evolution of category II FHR patterns, evaluation of fetal status over time should include not only the last 15-30 minutes of the FHR tracing, but the entire labor. Given the electronic storage of the FHR tracings during labor in most labor and delivery units, this task will take only few minutes.
Previous reviews have shown that undetectable or minimal FHR variability in the presence of late or variable decelerations is the most consistent predictor of newborn acidemia and that fetal acidemia with decreasing FHR variability and decelerations develops over time. Although there is a positive association between the depth of decelerations or bradycardia and fetal acidemia, the 2008 workshop did not consider the severity of FHR decelerations in the FHR classification; instead, it heavily relied on FHR baseline variability (moderate for category I, minimal for category II, and absent for category III). In our practical experience, we have found that one of the most frequent reasons for misinterpreting the severity of a FHR pattern is the human inability to distinguish between absent (amplitude range undetectable) vs minimal (amplitude range >undetectable and ≤5 beats per minute [bpm]) variability in a 10-minute window. As a matter of fact, it is not unusual to perceive epochs with both absent and minimal baseline FHR variability within the same 10-minute window. For this reason, we agree with Clark et al who proposed to classify and manage category II FHR tracings based on: (a) moderate (6-25 bpm) vs minimal or absent (≤5 bpm) FHR variability; (b) significance (late, severe variable or prolonged) and frequency of decelerations (≥50% of the contractions); and (c) estimated time to delivery by evaluating the progress of labor. The algorithm of Clark et al based on the aforementioned main criteria is definitely a step forward. However, by the time a fetus shows the most concerning features of (a) and (b) noted above, the optimum window of intervention for prevention of fetal injury may have passed. In cases of fetal hypoxia, it is very common to observe progressively more frequent episodes of tachycardia after decelerations that are initially transient and later become more consistent. This is because in response to repetitive hypoxic stress from uterine contractions, the fetus initially compensates by increasing its heart rate since its ability to increase stroke volume is not very efficient. However, the development of fetal tachycardia, as a longitudinal FHR change, in the course of fetal deterioration was not emphasized by either the 2008 workshop or the Clark et al report.
In our view, any pattern of decelerations that cause compensatory tachycardia should be included in the list of clinically significant decelerations. We believe that the significance of fetal tachycardia as an indicator of the fetal condition is missed by many clinicians when evaluating the progression of FHR changes. The association of fetal tachycardia with fetal compromise and injury is not a new concept, with the link suggested over a century ago. Ginsburg and Gerstley, in 1965 assessed outcomes in 102 fetuses with tachycardia (≥180 bpm) 31 of which also had episodes of FHR decelerations, called “bradycardias.” They noted that fetuses with tachycardia plus decelerations were much more likely to result in depressed infants, especially if this occurred >2 hours prior to delivery. In our view, frequent episodes of fetal tachycardia, or continuous fetal tachycardia, in response to FHR decelerations are commonly the first signs of fetal struggle when a longitudinal assessment is performed of infants compromised at delivery. More recent research has strongly suggested the combination of decelerations with fetal tachycardia is the strongest predictor of metabolic fetal acidemia. Fetal tachycardia is reported to be a better predictor of fetal acidemia (cord artery pH <7.10) than just late decelerations with adjusted odds ratios of 3.68 vs 2.28, respectively. There may be a tendency to underestimate the importance of tachycardia when there is a known cause such as maternal fever, but the presence of tachycardia with decelerations in a febrile mother should remain concerning for substantial fetal compromise.
The progression of FHR patterns during labor could be sudden from category I to category III in the presence of acute insults such as placental abruption, uterine rupture, bleeding vasa previa, or cord prolapse. However, more frequently, the progression of category I patterns to category II or III is gradual, developing over the course of many hours. Clinicians should consider these progressive longitudinal changes as a deteriorating fetal vital sign. There are few obstetric tragedies greater than a pregnancy that enters labor with an apparently healthy fetus and delivers a compromised infant, especially when many of these cases could be preventable. Obstetric services should audit all cases with FHR accelerations and moderate variability (category I FHR pattern) on admission, which end up with a birth of a depressed neonate in the absence of a sudden unexpected sentinel event. Such audits often provide important information that can be used to improve the quality and safety of obstetrical care. Review of the longitudinal FHR changes from admission and during the labor of these depressed infants should be presented to staff in the context of a safe learning environment, to identify prevention strategies.
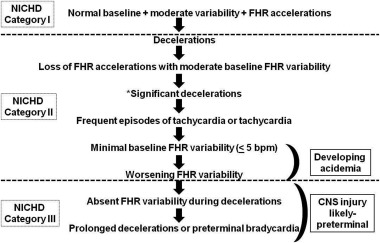
In our experience, as well in the experience of others, when longitudinal assessments are performed, compromised fetuses will often exhibit a progression in FHR patterns that is quite predictable, characterized by the sequential development of FHR decelerations, loss of accelerations, significant decelerations, rise of FHR baseline with frequent episodes of tachycardia or continuous tachycardia, minimal baseline variability, worsening variability, absent variability during decelerations, and prolonged or preterminal bradycardia ( Figure ). This sequence of FHR pattern deterioration should be used to help appropriately time the delivery prior to the development of category III or some of the ominous types of category II FHR patterns. It should be noted that the above sequence of FHR pattern changes will not be seen in fetuses initially found to have category II or III FHR patterns on presentation, since they may already have gone through these changes prior to admission.