Fig. 11.1
ASC-US (liquid-based preparation, LBP). (a) Mature squamous cells with nuclear enlargement, hyperchromasia, but even chromatin distribution. (b) ASC-US versus LSIL. Squamous cells with binucleation and nuclear enlargement: these are the only cells found on this Pap smear. (c) Squamous cells with multinucleation andFig. 11.1 (continued) nuclear enlargement. (d) ASC-US versus LSIL. Squamous cells with multinucleation, hyperchromasia, nuclear enlargement, and possible perinuclear halo. (e) Atypical parakeratosis. Cluster of squamous cells with irregular hyperchromatic nuclei and dense orangeophilic cytoplasm. (f) Single squamous cell with irregular hyperchromatic nucleus and possible perinuclear halo. (g) ASC-US versus LSIL. Single squamous cell with hyperchromatic nucleus and perinuclear halo. (h) Atypical repair. Single and cluster of cells with features suggestive of repair, but also enlarged nuclei, increased N/C ratio, irregular chromatin distribution, and conspicuous nucleoli
1.
Nuclei are about 2½–3 times the area of the nucleus of a normal intermediate squamous cell.
2.
Slight increase in nuclear to cytoplasmic ratio (N/C).
3.
Nuclear membrane is smooth to slightly irregular.
4.
Nuclear hyperchromasia is absent to light.
5.
Chromatin is finely granular and evenly distributed.
6.
Nucleoli/chromocenters are inconspicuous or absent.
7.
Cells present singly and in sheets.
8.
Atypical parakeratosis may present as small orangeophilic cells with moderate cellular pleomorphism, slight increase in nuclear size, and vesicular or pyknotic chromatin.
9.
Suggestive HPV cytopathic effect and/or binucleation may be present, but fall short of LSIL.
ASC-US includes the following patterns:
1.
Mature intermediate squamous cells with changes that resemble koilocytes, but lack all of the features of typical koilocytes (e.g., definite hyperchromasia, sharp perinuclear halos, or binucleation).
2.
Atypical parakeratosis with dense orangeophilic cytoplasm, minimal nuclear irregularity, and mild nuclear atypia.
3.
Atypical repair cells with features of repair and presence of marked nuclear size variation, prominent nucleoli, and irregular chromatin distribution.
4.
Atypia of atrophy with nuclear enlargement, hyperchromasia, or irregular nuclear contours.
5.
ASC-US may refer to cells with atypical nuclear features due to air-drying artifact in conventional smears or distorted cells at the rim of liquid-based cytology specimens.
Differential Diagnosis
Reactive Changes
The nucleus in cells with reactive changes may increase up to two times the area of the nucleus of a normal intermediate squamous cell with hypochromasia, fine chromatin, and smooth nuclear contour. The N/C ratio is low, and the cytoplasm is degenerative. Nucleoli may be seen (Fig. 11.2).
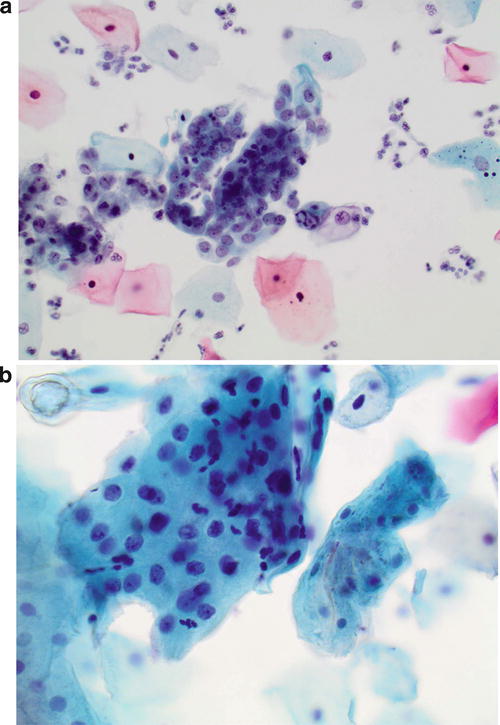
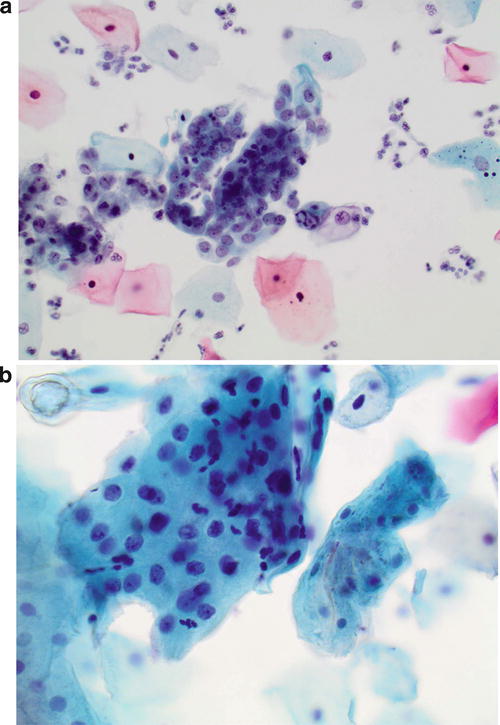
Fig. 11.2
Reactive endocervical cells (liquid-based preparation, LBP). (a) Endocervical cells with enlarged nuclei, fine chromatin, regular nuclear contour, and prominent nucleoli arrange in a glandular pattern. (b) Reactive squamous cells in the presence of inflammation. Clusters of squamous cells with enlarged nuclei, regular nuclear contour, and prominent nucleoli
LSIL
The nucleus in LSIL cells is usually more than three times the area of the nucleus of a normal intermediate squamous cell with irregular nuclear shape and contour, hyperchromasia, binucleation/multinucleation, and coarse chromatin. Nucleoli are usually inconspicuous. Typical koilocytes have sharply defined perinuclear halos.
Follow-Up Results
In a s creened US population, approximately 50 % of ASC-US cases are positive for high-risk human papillomavirus (hr-HPV). Approximately 10–20 % of women with ASC-US were proven to have CIN2–3 on biopsy. Approximately 30–50 % of women with ASC-US were proven to have CIN1 on biopsy [9].
Management
The 2012 updated consensus management guidelines recommend that high-risk HPV testing is the preferred method for women ages 25 years or older, although repeat cytology at 1 year is acceptable. Colposcopy is not an option for women with ASC-US in the 2012 updated g uideline. For women ages 21–24 years with ASC-US, repeat cytology at 1 year is the preferred method, although high-risk HPV testing is acceptable.
ASC-H
Definition
ASC-H represents squamous cells with findings that are suggestive of high-grade SIL (HSIL) and accounts for less than 10 % of ASC cases.
Morphology (Fig. 11.3)
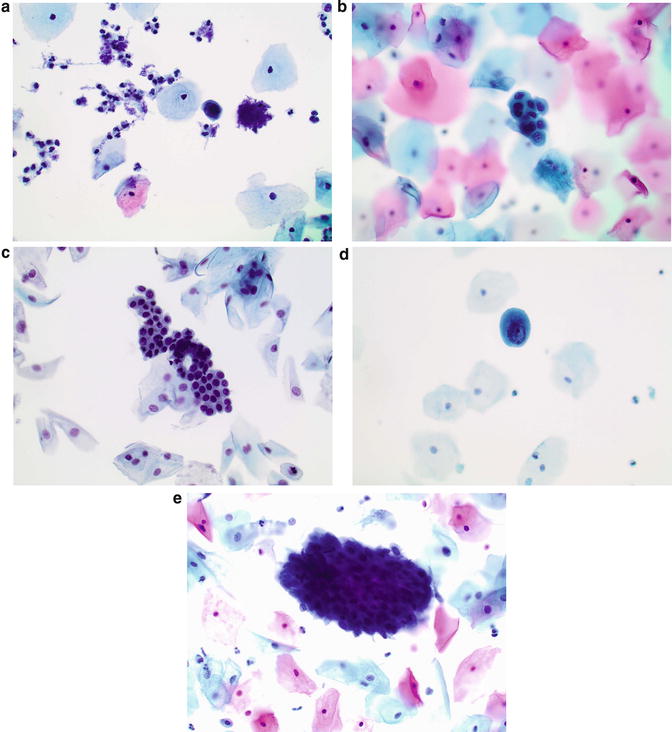
Fig. 11.3
ASC-H (liquid-based preparation, LBP ). (a) Single small cell with scant cytoplasm, high N/C ratio, and a dark hyperchromatic nucleus which shows round nuclear contour and irregular chromatin distribution. (b) A loose cluster of cells with metaplastic cytoplasmic change, high N/C ratio, hyperchromatic nuclei, variation in size of nuclei, and minimal irregular nuclear contour. (c) A relatively large cluster of cells with thin rim of cytoplasm, high N/C ratio, and round hyperchromatic nuclei. (d) Single small cell with metaplastic cytoplasmic change, high N/C ratio, and a dark hyperchromatic irregular nucleus and irregular chromatin distribution. (e) A hyperchromatic group of cells with dark nuclei and nuclei overlapping, which are difficult to be ascertain
Small cell pattern (atypical immature squamous metaplasia) : immature (small) squamous cells with high N/C ratio but mild-moderate nuclear atypia
1.
Small fragments or individual cells
2.
Nuclei size is 1½–2½ times larger than normal intermediate cell nuclei
3.
Smooth to slightly irregular nuclear membrane
4.
Increased N/C ratio, similar to that of HSIL
5.
Finely granular and evenly distributed chromatin
6.
Inconspicuous or absent nucleoli
Hyperchromatic crowded group (HCG) pattern :
1.
Groups of crowded cells with sharp linear edges
2.
Polygonal cells containing nucle i with loss of polarity or difficultly visualized nuclei and dense cytoplasm
Differential Diagnosis
1.
Squamous metaplasia : mostly in sheets and cobblestone-like clusters or individual cells with homogenous dense cytoplasm, uniform round to oval nuclei, smooth nuclear membranes, and fine chromatin (Fig. 11.4).
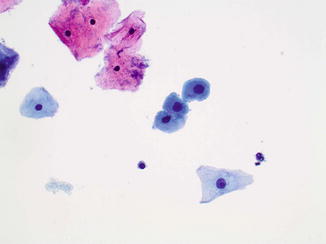
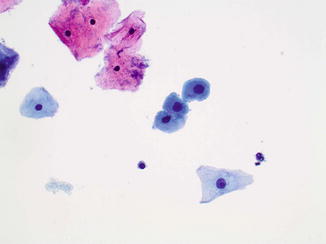
Fig. 11.4
Squamous metaplasia (liquid-based preparation, LBP ). Individual cells with homogenous dense cytoplasm, uniform round to oval nuclei, smooth nuclear membranes, and fine chromatin
2.
Atrophy : sheets/single parabasal cells with abundant cytoplasm, uniform round to oval nuclei, smooth nuclear membranes, and fine chromatin. Cell borders are usually distinct.
3.
Repair : flat sheets with maintained polarity (streaming) containing cells with minimal nuclear enlargement (1½–2 times enlargement), smooth nuclear membrane, mild hyperchromasia, finely granular and evenly distributed chromatin, prominent single or multiple nucleoli, dense cytoplasm with polychromasia, or vacuolization in a background of inflammation (Fig. 11.5).
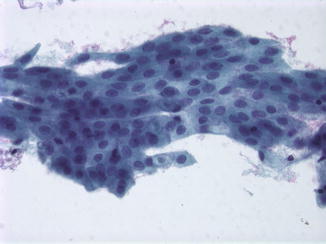
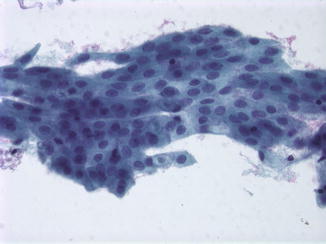
Fig. 11.5
Repair (liquid-based preparation, LBP). Flat sheets with maintained polarity containing cells with minimal nuclear enlargement, smooth nuclear membrane, mild hyperchromasia, finely granular and evenly distributed chromatin, prominent nucleoli, and dense cytoplasm
4.
Radiation : markedly enlarged cells with no significant increase of N/C ratio, bizarre cell shapes, variable nuclear size, binucleation/multinucleation, smudging chromatin, prominent single/multiple nucleoli, and cytoplasmic vacuolization.
5.
Histiocytes : streaming single cells with round, ovoid, and bean-shaped nuclei, foamy cytoplasm, a low N/C ratio, and fine cytoplasmic vacuoles.
6.
HSIL : cells with conspicuous nuclear atypia, a greater N/C ratio (nuclear size > 2× the size of normal intermediate cells), more pronounced irregular nuclear contours, and marked coarse chromatin.
7.
Endometrial cells : small cells with bean-shaped nuclei and smudgy chromatin in 3D clusters (Fig. 11.6).
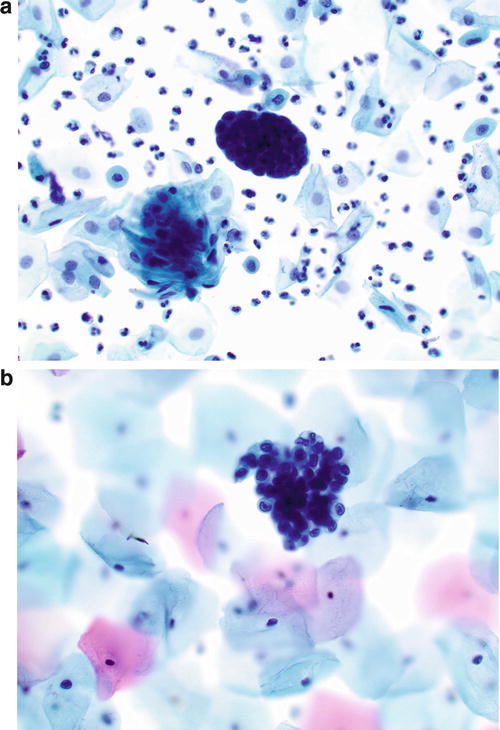
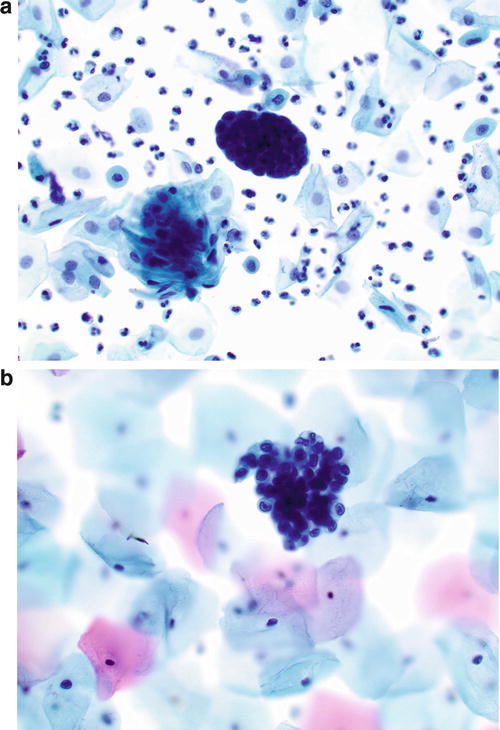
Fig. 11.6
Endometrial cells (liquid-based preparation, LBP). (a) A tight cluster of small cells in 3D structure. (b) Small cells with bean-shaped nuclei
Follow-Up Results
Approximately 30–50 % of ASC-H cases prove to have CIN2 or CIN3 on follow-up biopsy, and the incidence is higher in younger patients [10].
Management
The 2012 updated consensus management guidelines recommend women with ASC-H cytology to undergo colposcopy regardless of HPV results. Reflex HPV testing is not recommended. Recent studies and CAP survey results indicate that HPV-positive rate is about 50–60 % in women with ASC-H Pap test.
Follow-up of patients with HPV-negative ASC-H results yielded very low rates of detectible CIN2/3 (1.6 %) and no diagnoses of cervical cancer. Triage of study patients with HPV-negative ASC-H results to routine HPV and cytology co-testing at 1 year was a safe follow-up option [11].
LSIL
Definition
LSIL represents squamous cells with mild dysplasia or koilocytosis caused by both low-risk and high-risk HPV infections. The majority of LSIL represent a transient HPV infection which usually regresses within 1–2 years. Less than 2 % of LSIL will progress to invasive cervical carcinoma if untreated.
Koilocytosis represents HPV-associated cytopathic effect in mature intermediate or superficial cells.
Morphology (Fig. 11.7)
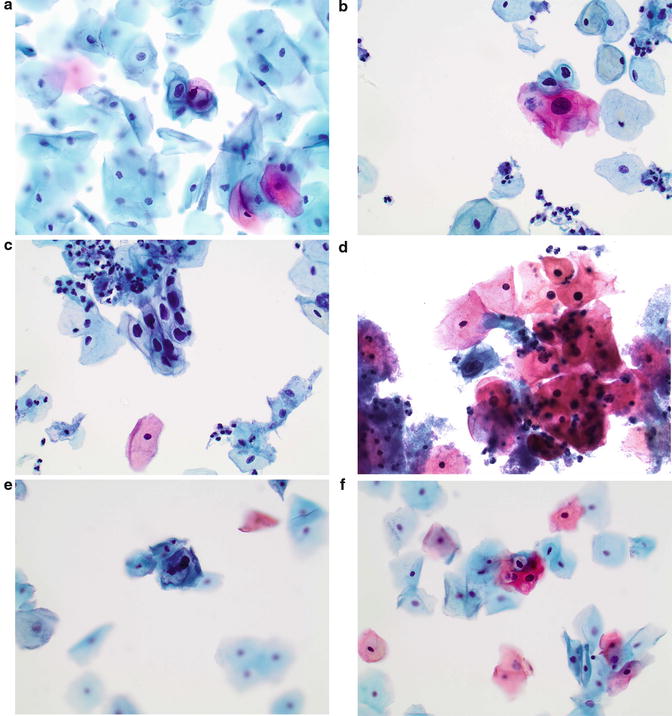
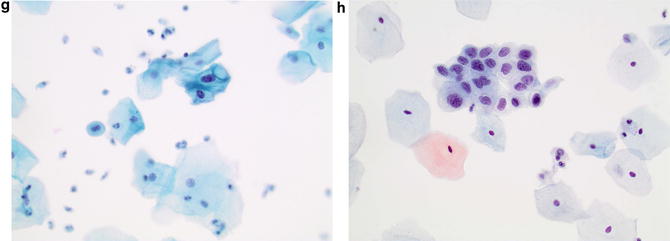
Fig. 11.7
LSIL (liquid-based preparation, LBP). (a) Squamous cells with slightly increased N/C ratio, slightly coarse chromatin, irregular and hyperchromatic nuclei, well-defined perinuclear cavitation, and a dense peripheral rim of cytoplasm. (b) Single squamous cells with slightly enlarged, irregular, and hyperchromatic nuclei, well-defined perinuclear cavitation, and a dense peripheral rim of cytoplasm. (c) A cluster of squamous cells with enlarged, highly irregular, and hyperchromatic nuclei, relatively abundant dense cytoplasm, slightly increased N/C ratio, and well-defined perinuclear cavitation. (d) Single squamous cells with binucleation, well-defined perinuclear cavitation, and relatively abundant dense cytoplasm. (e) Single squamous cells with multinucleation and well-defined folded perinuclear cavitation. (f) Squamous cells with small, but highly hyperchromatic, nuclei and well-defined perinuclear cavitation. (g) LSIL versus ASC-US. Cells with slightly enlarged, slightly hyperchromatic nuclei and binucleation. (h) SIL, grade cannot be determined. Atypical squamous cells with irregular hyperchromatic nuclei, moderate amount of cytoplasm, and slightly increase N/C ratio. Based on the nuclear features, these cells are interpreted as SIL, but not gradable due to moderate amount of cytoplasm and absence of perinuclear halo
1.
Singly or sheets of mature/superficial squamous cells with distinct cytoplasmic borders.
2.
Slightly increased N/C ratio.
3.
Nuclear size >3 times the size of a normal intermediate nucleus.
4.
Variable nuclear size and shape.
5.
Smooth to slightly irregular nuclear membranes.
6.
Variable hyperchromasia.
7.
Binucleation or multinucleation may be seen.
8.
Slightly coarse but evenly distributed chromatin.
9.
Koilocytosis: squamous cells with well-defined perinuclear cavitation and a dense peripheral rim of cytoplasm together with nuclear abnormalities.
10.
Other LSIL cells include macrocytes, kite cells with cytoplasmic tails, polka dot cells with cytoplasmic globules, and balloon cells with clear cytoplasm.
Differential Diagnosis
1.
Reactive squamous cells with nonspecific halos. Nonspecific perinuclear halos usually show small clearings without nuclear atypia and can be caused by trichomoniasis infection, other inflammatory changes, or artifact during slide preparation (Figs. 11.8 and 11.9).
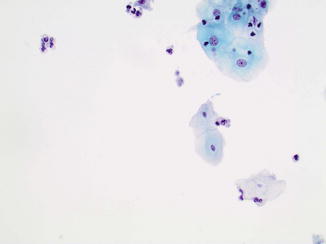
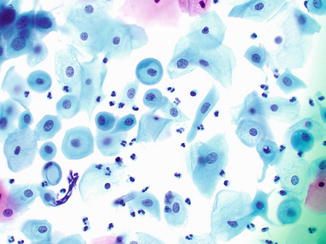
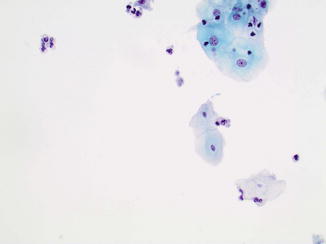
Fig. 11.8
Reactive squamous cells in the presence of trichomonas vaginalis. Clusters of squamous cells with enlarged nuclei, regular nuclear contour, and prominent nucleoli on the upper right corner. Trichomonas vaginalis can be seen in the center of the image (liquid-based preparation, LBP)
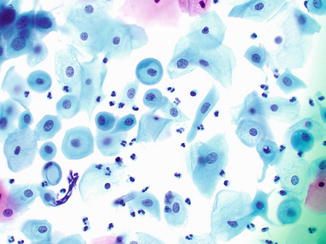
Fig. 11.9
Nonspecific clear perinuclear halos can be seen in glycogenated intermediate cells during pregnancy or other conditions. These cells lack typical nuclear features of LSIL (liquid-based preparation, LBP)
2.
Reactive endocervical cells can show enlarged nuclei and hyperchromasia which may mimic LSIL cells. However, reactive endocervical cells usually show regular nuclear contour and prominent nucleoli (Fig. 11.10).
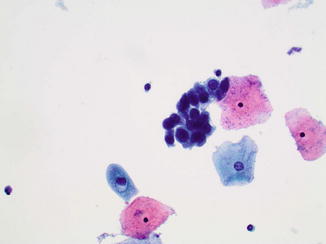
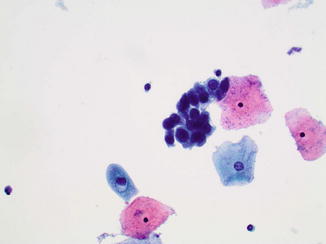
Fig. 11.10
Reactive endocervical cells with enlarged nuclei and hyperchromasia, but regular nuclear contour. A nonspecific clear perinuclear halo is also seen in a reactive squamous cell (liquid-based preparation, LBP)
3.
Parakeratosis or atypical parakeratosis (ASC-US). The cells with parakeratosis are much smaller than koilocytes and do not display atypia. The cells with atypical parakeratosis show nuclear atypia but not enough for a diagnosis of LSIL cells (Fig. 11.1).
4.
Postpartum changes. Navicular cells found in pregnant women can show empty vacuoles which may mimic perinuclear halos. However, nuclei are round to oval and uniform with fine and evenly distributed chromatin.
Follow-Up Results
Approximately 15–25 % of LSIL cases prove to have histologic CIN2 or CIN3 during follow-up biopsies [12].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


