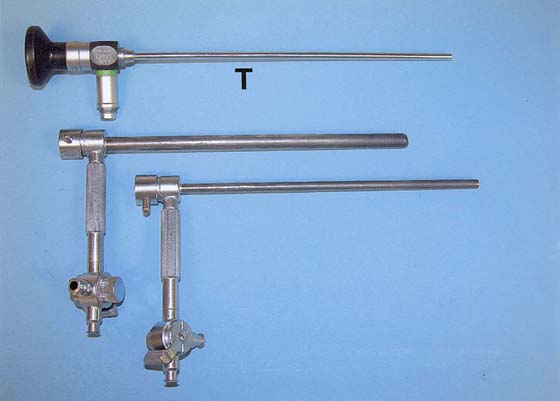
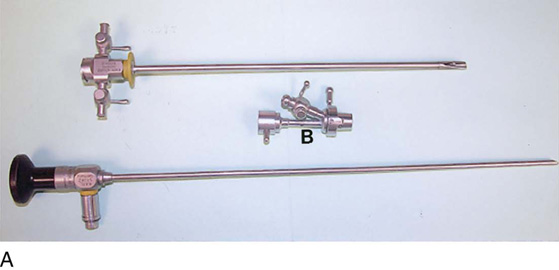
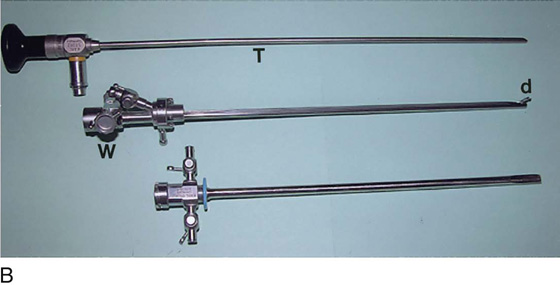
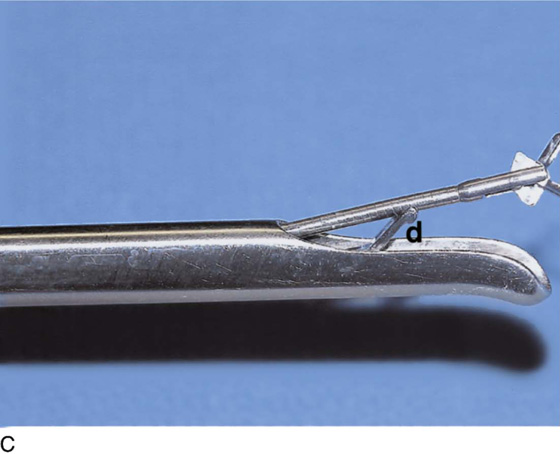
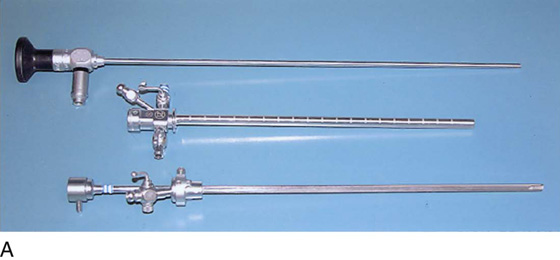
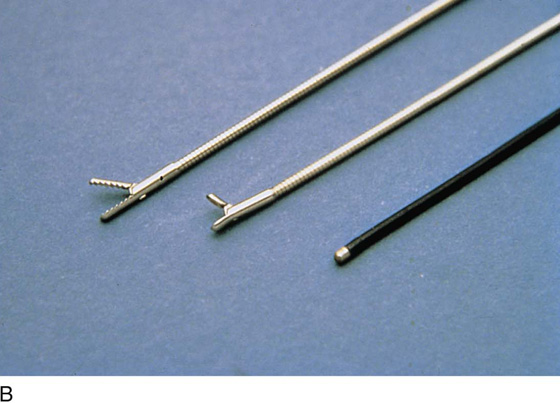
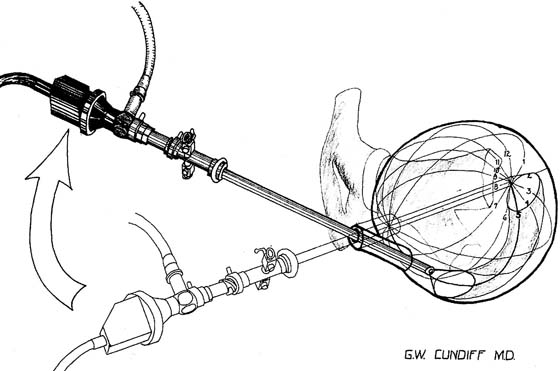
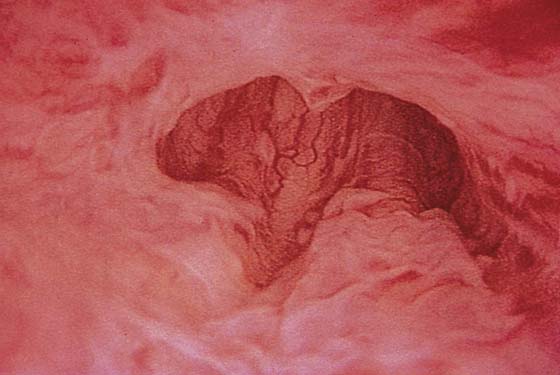
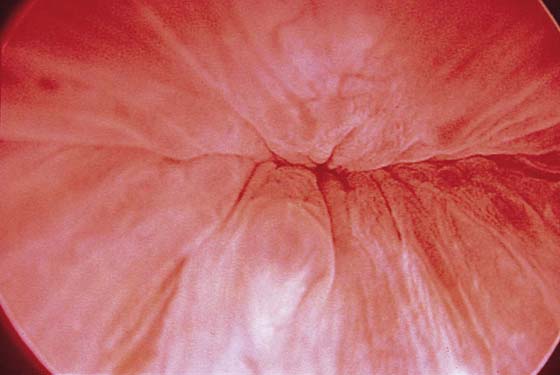
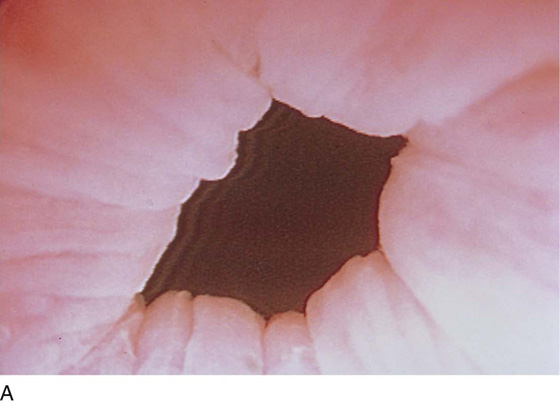
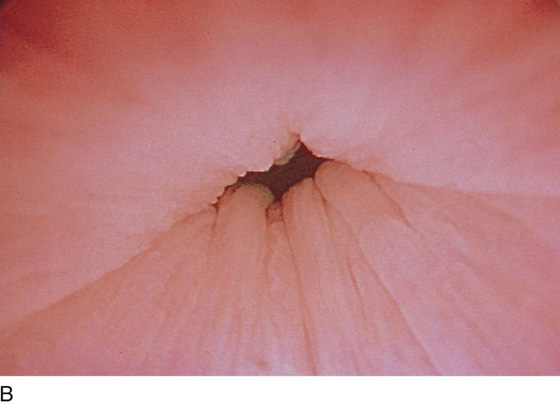
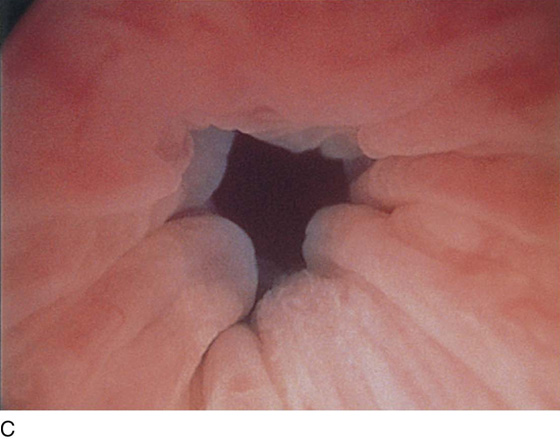
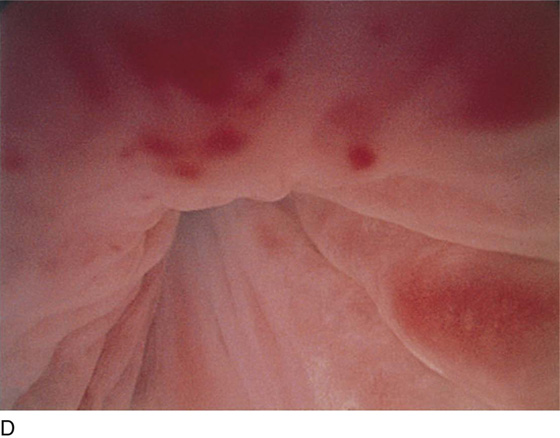
CHAPTER 123 The rigid urethroscope is a modification of the cystoscope, designed exclusively for evaluation of the urethra (Fig. 123–1). Because it is primarily a diagnostic instrument, it does not have a bridge. The telescope is shorter and has a 0° viewing angle, which provides a circumferential view of the urethral lumen as the mucosa in front of the urethroscope is distended by a distention medium. The 0° lens is essential for adequate urethroscopy. The urethroscope sheath is designed to maximize distention of the urethral lumen. Sheaths are available in 15F and 24F calibers. If tolerated, the larger sheath is useful because it provides the best view of the urethral lumen by providing more rapid fluid flow for maximal distention. It also allows easier visibility of any abnormalities such as urethral diverticula. The rigid cystoscope has three components: the telescope, the bridge, and the sheath (Fig. 123–2A through C). Each component serves a different function and is available with various options to facilitate its role under different circumstances. The telescope transmits light to the bladder cavity, as well as an image to the viewer. Telescopes designed for cystoscopy are available with several viewing angles, including 0° (straight), 30° (forward oblique), 70° (lateral), and 120° (retroview). The different angles facilitate the inspection of the entire bladder wall. Although the 0° lens is essential for adequate urethroscopy, it is insufficient for cystoscopy. The 30° lens provides the best view of the bladder base and posterior wall, and the 70° lens permits inspection of the anterior and lateral walls. The retroview of the 120° lens is not usually necessary for cystoscopy of the female bladder but can be useful for evaluating the urethral opening into the bladder. In diagnostic cystoscopy, the 30° telescope usually is sufficient, although a 70° telescope may be required in the presence of elevation of the urethrovesical junction, such as after colposuspension procedures. The angled telescopes have a field marker, which is a blackened notch on the outside of the visual field opposite the angle of the deflection that helps facilitate orientation. The cystoscope sheath provides a vehicle for introducing the telescope and distending media into the bladder cavity. Sheaths are available in various calibers, ranging from 17F to 28F for use in adults. When placed within the sheath, the telescope, which is a 15F instrument, only partially fills the lumen, leaving an irrigation working channel. The smallest sheath is better tolerated for diagnostic purposes, whereas usually at least a 19F sheath is required for placement of instruments into the irrigation working channel. The proximal end of the sheath has two working ports: one for introduction of the distending media and another for removal. The distal end of the cystoscope sheath is fenestrated to permit use of instrumentation in the angled field of view. It is also beveled, opposite the fenestra, to increase the comfort of the introduction of the cystoscope into the urethra. The bridge serves as a connector between the telescope and sheath and forms a water-tight seal. It also may have one or two ports for introduction of instruments into the irrigation working channel. The Albarran bridge is a variation with a deflector mechanism at the end of the inner sheath. When placed in the cystoscope sheath, the deflector mechanism is located at the distal end of the inner sheath within the fenestra of the outer sheath. In this location, elevation of the deflector mechanism assists the manipulation of instruments within the field of view. Unlike the rigid cystoscope, the flexible cystoscope combines the optical systems and irrigation working channel in a single unit (Fig. 123–2D). The coated tip is 15F to 18F in diameter and 6 to 7 cm in length; the working unit makes up half the length. The flexibility of the fibers permits incorporation of a distal tip-deflecting mechanism, controlled by a lever at the eyepiece that will deflect the tip 290° in a single plane. Any light source that provides adequate illumination via a fiberoptic cable is sufficient. A high-intensity xenon light source is often recommended for use in video monitoring or photography, but with recent innovations, the newest cameras require less light. Video recording and still-picture capabilities are very important for documentation, as well as teaching. Three types of distention media are available: nonconductive fluids, conductive fluids, and gases. Cystourethroscopy is feasible with carbon dioxide, but most practitioners prefer the use of water or saline to distend the bladder and urethra. A liquid medium prevents the carbon dioxide from bubbling and washes away blood or debris that can limit visualization. Moreover, the bladder volumes achieved using a liquid medium more accurately approximate physiologic volumes. Instrument care requires the removal of blood and debris from the equipment promptly to avoid accumulation in crevices and pitting of metal surfaces. The most common method of sterilization is immersion in a 2% activated glutaraldehyde solution (Cidex, or Surgifix, Inc, Arlington, Texas). Cystourethroscopic equipment should be soaked for 20 minutes and then transferred to a base of sterile water until ready for use. Operative instruments may be passed through operative channels in accordance with the size of the operative sheath. The most useful of these are a grasper, a biopsy forceps, and a cautery electrode (Fig. 123–3A through C). FIGURE 123–1 Components of the urethroscope. The 0° telescope (T) is shown at the top. Below are two sheaths (15F and 24F). FIGURE 123–2 Components of a rigid cystoscope. A. Above is the sheath (17F) with water intake valves on the right and left. In the center is a bridge with an operating channel that attaches to the above sheath. Lowermost is a telescope, which can range from 30° to 70°. In this case, the telescope has a 70° lens. B. This rigid cystoscopic system consists of a telescope (T), an operative sheath with a bridge and terminal deflector (d), and an operative sheath without the deflector. The deflector (d) is controlled by the wheel (W) device mounted onto the proximal portion of the sheath. C. Close-up of the deflector (d). Note how the deflector permits manipulation of the biopsy forceps. D. Unlike the rigid cystoscope, the flexible device combines optical, irrigation, and operating channels in a single unit. FIGURE 123–3 Components of operative hysteroscopic sheaths. A. The telescope is usually 0° or 30°. In this case, the telescope has a 12° lens. B. Accessory instruments that are passed via the channel and into the bladder include (from left to right) alligator grasping forceps, biopsy forceps, and a coagulating electrode. C. An injection needle has been placed through the channel, and a collagen implant (Contigen) (c) will be injected. (B from Cundiff GW, Bent AE: In Endoscopic Diagnosis of the Female Lower Urinary Tract. WB Saunders, UK London, 1999, with permission.) Indications for visualizing the anatomy of the female urethra and bladder include recurrent urinary tract infection, irritative bladder and urethral symptoms, hematuria, urogenital fistula, urethral or bladder diverticulum, complicated urinary stress incontinence, unresolved overactive bladder, suspected interstitial cystitis, calculus, suspected bladder or urethral cancer, obstructive voiding symptoms, suspected foreign body, assessment of ureteral function, and staging for cervical cancer. The procedure is performed in the office or ambulatory clinic. The patient is examined in the lithotomy position, and generally no analgesia is used. Topical anesthesia may be applied but usually is needed only on the cystoscopic sheath to allow it to slide along the tissues. The urethra is visualized using a 0° telescope with the infusion fluid (sterile water or saline) running briskly, by passing the instrument through the distal urethra and advancing it slowly to the bladder neck. The bladder is visualized by passing the 30° or 70° telescope with attached bridge and 17F sheath through the urethra in a smooth motion in a direction toward the umbilicus. The bladder is systematically examined at each hour of an imaginary clock, and then the trigone and ureters are visualized carefully (Fig. 123–4). The urethral mucosa is visualized as the instrument is passed through the urethra toward the bladder neck (Figs. 123–5 through 123–7). The effects of hold, cough, and strain maneuvers are observed at the bladder neck. The urethrovesical junction normally closes (Fig. 123–8). Voiding or urethral opening secondary to detrusor activity causes the urethra to open widely (Fig. 123–9). A similar picture is noted if the bladder neck is visualized in a patient with detrusor instability (Fig. 123–10). With the bladder relatively full and a finger compression beyond the end of the scope, the scope is slowly withdrawn as the infusing fluid distends the urethra. Periurethral glands (Fig. 123–11A through C) and exudate from the glands may be observed (Fig. 123–12). Other benign findings include inclusion cysts (Fig. 123–13A, B) and fronds and polyps (Fig. 123–14A through C). Pathologic changes include urethral prolapse (Fig. 123–15A, B), caruncle (Fig. 123–16), inflammation (Fig. 123–17A through C), diverticulum (Fig. 123–18A through C), fistula (Fig. 123–19), and an ectopic ureter opening at the bladder neck (Fig. 123–20). FIGURE 123–4 Cystoscopic evaluation of the bladder. The bladder cavity is evaluated by making 12 sweeps along each hour of the clock from the bladder dome to the urethrovesical junction. The 5 o’clock examination is being performed, so the light cord is at 11 o’clock, or 180° opposite the direction the lens is looking. (From Cundiff GW, Bent AE: In Endoscopic Diagnosis of the Female Lower Urinary Tract. WB Saunders, UK London, 1999, with permission.) FIGURE 123–5 Normal urethra. (From Cundiff GW, Bent AE: In Endoscopic Diagnosis of the Female Lower Urinary Tract. WB Saunders, UK London, 1999, with permission.) FIGURE 123–6 Coaptation of urethra. (From Cundiff GW, Bent AE: In Endoscopic Diagnosis of the Female Lower Urinary Tract. WB Saunders, UK London, 1999, with permission.) FIGURE 123–7 Urethral metaplasia. (From Cundiff GW, Bent AE: Endoscopic Diagnosis of the Female Lower Urinary Tract. WB Saunders, UK London, 1999, with permission.) FIGURE 123–8 Maneuvers at the bladder neck. A. Open urethrovesical junction. B.
Cystourethroscopy
Instrumentation
Indications and Techniques
Urethroscopy (Normal and Abnormal Findings)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Geoffrey W. Cundiff
Geoffrey W. Cundiff