Cystocele Repair Using the Defect-Directed Approach
Geoffrey W. Cundiff
INTRODUCTION
Providing optimal care for a cystocele, or prolapse of the anterior vaginal wall, begins with recognition of the heterogenous nature of pelvic organ prolapse, and a focus on the primary goal of intervention, relief of symptoms. Cystoceles frequently occur with concurrent prolapse of the posterior vaginal wall and/or the vaginal apex, and a durable repair requires attention to these support defects as well.
While prolapse is ubiquitous in parous women, it does not warrant treatment unless it is symptomatic. The symptoms commonly attributed to anterior prolapse include pelvic pressure, a sensation or visualization of protrusion, urinary dysfunction, and sexual dysfunction. While symptoms of protrusion are almost always due to prolapse, predicting which patients will have relief from urinary dysfunction and sexual dysfunction depends on a thorough understanding of the anatomy of support of the anterior wall as well as the differential diagnosis of these symptoms. Studies show that resolution of urinary symptoms is the most commonly stated goal for patients, regardless of stage of prolapse. The ability to perform daily activities, and sexual function goals are at least as important as resolution of prolapse symptoms and may be the reason for seeking care.
There are a variety of surgical techniques available to the surgeon treating cystocele, including the anterior colporrhaphy, anterior fascial reinforced repair (Chapter 35). Each of these approaches has strengths and limitations. The defect-directed repair, also known as the site-specific fascial repair, aims to maximize relief of symptoms without creating new functional symptoms, through recreating normal anatomy. The technique is based on Richardson’s observations at the time of cystocele repair and during cadaveric dissections, of discrete tears or breaks in the pubocervical fascia or vaginal muscularis. He advocated an anatomical repair limited to repair of these fascial tears or defects in the pubocervical fascia without attempts to narrow the vaginal caliber. This approach appears to improve the relief of protrusion symptoms due to prolapse. However, its reliance on native tissues that may be compromised in women with pelvic organ prolapse, may have a negative impact on its durability. Nevertheless, it is a good choice for a patient that desires a repair using native tissue, especially if she has no risk factors for recurrence.
PREOPERATIVE CONSIDERATIONS
Some surgeons advocate preoperative estrogen cream to promote a healthier mucosal epithelium in atrophic postmenopausal patients although histological studies do not support this hypothesis. A bowel preparation is not generally indicated preoperatively. Antibiotic prophylaxis with a second generation cephalosporin or metronidazole is recommended, although there is minimal data to show its efficacy. A risk assessment for deep venous thromboembolism prophylaxis is also recommended. The patient should be positioned in lithotomy or modified
lithotomy position. Either regional anesthesia or general anesthesia is appropriate. Submucosal infiltration with injectable lidocaine with epinephrine simplifies postoperative pain and assists dissection and hemostasis. A Foley catheter should be placed during the surgery to drain the bladder. Following is a brief description of the surgical procedure used (see also video: Cystocele Repair Using the Defect-directed Approach).
lithotomy position. Either regional anesthesia or general anesthesia is appropriate. Submucosal infiltration with injectable lidocaine with epinephrine simplifies postoperative pain and assists dissection and hemostasis. A Foley catheter should be placed during the surgery to drain the bladder. Following is a brief description of the surgical procedure used (see also video: Cystocele Repair Using the Defect-directed Approach).
SURGICAL TECHNIQUE
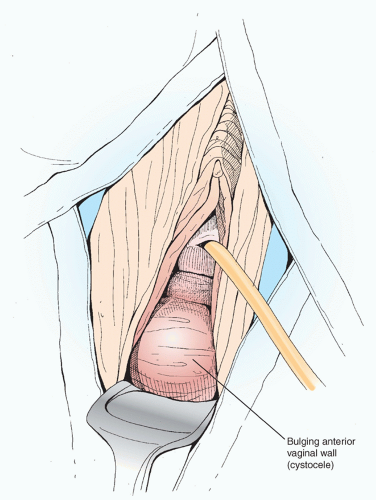
 Begin by defining the scope of the cystocele. Placement of a vagina retractor provides access to the anterior vaginal wall (Figure 33.1). The surgical approach begins with a longitudinal incision in the midline of the anterior vaginal wall (Figure 33.2). This incision begins just proximal to the external urethral meatus and is carried approximately to two-thirds of the vaginal length. The vaginal epithelium is then dissected off the underlying tissue in the plane between the mucosa and the vaginal muscularis or pubocervical fascia (Figure 33.3A). Finding this plane is essential to identifying the location of the rent in the pubocervical fascia. This dissection is facilitated by using sharp dissection combined with countertraction provided by Allis clamps, a self-retaining retractor, or by using a finger behind the vaginal mucosa (Figure 33.3B). Moreover, as the rent can occur in the midline of the pubocervical fascia or at its lateral attachments, the dissection should be carried laterally to the arcus tendineus fascia pelvis or white line, the normal attachment of the pubocervical fascia to the obturator internus muscle, and superiorly to the cervix or vaginal cuff (Figure 33.3C).
Begin by defining the scope of the cystocele. Placement of a vagina retractor provides access to the anterior vaginal wall (Figure 33.1). The surgical approach begins with a longitudinal incision in the midline of the anterior vaginal wall (Figure 33.2). This incision begins just proximal to the external urethral meatus and is carried approximately to two-thirds of the vaginal length. The vaginal epithelium is then dissected off the underlying tissue in the plane between the mucosa and the vaginal muscularis or pubocervical fascia (Figure 33.3A). Finding this plane is essential to identifying the location of the rent in the pubocervical fascia. This dissection is facilitated by using sharp dissection combined with countertraction provided by Allis clamps, a self-retaining retractor, or by using a finger behind the vaginal mucosa (Figure 33.3B). Moreover, as the rent can occur in the midline of the pubocervical fascia or at its lateral attachments, the dissection should be carried laterally to the arcus tendineus fascia pelvis or white line, the normal attachment of the pubocervical fascia to the obturator internus muscle, and superiorly to the cervix or vaginal cuff (Figure 33.3C). FIGURE 33.2 Mucosal incision; a longitudinal incision beginning just distal to the external urethral meatus. |
Once the dissection is complete, the surgeon must identify the location of the rent in the pubocervical fascia. The defect in the pubocervical fascia can occur in the midline, or through a separation of the pubocervical fascia from the white line on either side (Figure 33.4A




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree