Traditional Natural Cycle IVF∗. ╤If at risk of premature ovulation, use indomethacin. If premature ovulation occurs, OPU within 24 hours. E2 estradiol, LH luteinizing hormone, OPU oocyte pickup
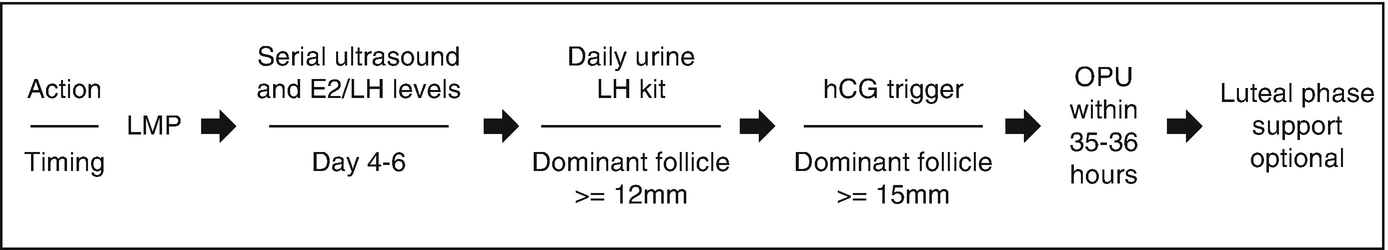
Modified Natural Cycle IVF with hCG Trigger∗
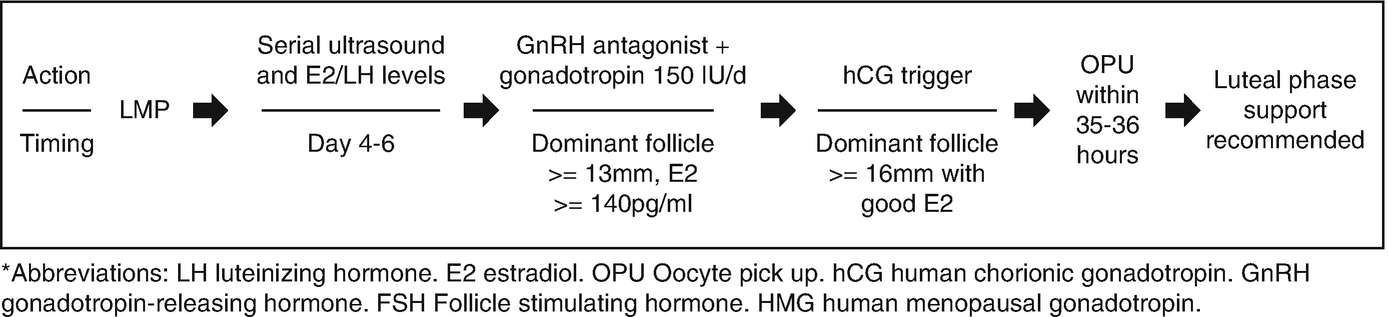
Modified Natural Cycle IVF with a GnRH Antagonist∗. ∗Abbreviations: LH luteinizing hormone, E2 estradiol, OPU Oocyte pick up, hCG human chorionic gonadotropin, GnRH gonadotropin-releasing hormone, FSH Follicle stimulating hormone, HMG human menopausal gonadotropin
9.3 Natural Cycle IVF Outcomes
In the early days of IVF, Edwards reported an ongoing pregnancy rate of 14.7% per oocyte retrieval and 19% per embryo transfer with natural cycles, which leads to a rate of 1 clinical pregnancy per 6.8 embryos [7]. More recently, a randomized controlled trial showed a clinical pregnancy rate of 14.9% per embryo transfer with natural cycle IVF, but the rate did not improve after three cycles [8]. In 2016, Sunkara found that it would take 4.8 natural cycles with fresh embryo transfer to achieve the pregnancy rates observed in one conventional cycle [9]. A prospective cohort study that looked at 844 natural cycles found that the ongoing pregnancy rate after 3 modified natural cycles was 20.8% with a cancellation rate of 17.7% [10]. The author comments that the occurrence of cancellation of oocyte retrieval, unsuccessful oocyte retrieval, and fertilization failure are recurrent events, and patients should receive counseling in such cases. When the patients were pushed toward nine cycles [11], the ongoing pregnancy rates approached 35.8%, but the dropout rate was significant at 47.8%. The dropout rate was noted to increase sharply after three cycles.
Given that women with POR, by definition, do not respond well to conventional stimulation, natural cycle IVF has been studied as a less expensive and more patient-friendly approach for reproductive assistance in this specific subpopulation. A randomized controlled trial comparing natural cycle to microdose flare high-dose FSH protocol in women with POR, defined as three or fewer follicles recruited or cycle cancelled because of no follicular activation, did not show a significant difference in pregnancy per cycle (6.1 vs 6.9%, respectively). However, implantation rate was significantly higher with natural cycle [7]. In 2009, Schimberni showed a similar pregnancy rate of 9.8% per cycle and 16.7% per embryo transfer in women with POR, defined as patients ≤ 44 years old with a previous cycle that was cancelled due to no follicular activation or only one follicle recruited [12]. In a general poor responder population, defined as ≤ 4 oocytes retrieved and/or E2 level <1000 pg/mL on day of hCG administration, Elizur reported a pregnancy rate of 9% [13]. In poor responders defined by an increased baseline FSH >10mIU/mL and possibly <7AFC, Papaleo found a pregnancy rate of 11.5% per cycle and 20% per embryo transfer [14].
In 2011, the ESHRE created a definition of poor ovarian response in an attempt to standardize the literature. In order to be diagnosed with poor ovarian response, women must meet two of the following three criteria: (1) advanced maternal age or any other risk factor for poor ovarian response, (2) a previous poor ovarian response, and (3) an abnormal ovarian reserve test [15]. When applying this definition, the outcomes appear to worsen. Kedem compared modified natural cycle to conventional IVF and, in poor responders per ESHRE definition, found that the live birth rate was less than 1%, meeting ASRM criteria for futility [16]. Lainas also found very low chances of live birth with modified natural cycle (MNC) but makes the comment that MNC may be more patient-friendly and cost-effective when anticipated live birth rates are low [17]. While Polyzos does not endorse natural cycle in Bologna-criteria poor responders, he does note that pregnancy rates approach 10% after four cycles. Interestingly, Shaulov showed divergent clinical pregnancy rates (CPR) with regard to age in poor responders. In 1503 MNC cycles, the CPR in those ≥36 years old with normal ovarian response was 26.26% per embryo transfer and with poor ovarian response was 6.25% per embryo transfer. However, the CPRs were not divergent between normal and poor ovarian responders ≤35 years old [18].
Lastly, more recent data question the relationship of gonadotropin dosing with both aneuploidy rates and oocyte quality. Baart showed that the proportion of abnormal embryos per patient significantly reduced after mild, versus high, dose stimulation protocols. She also noted that the percentage of mosaic embryos was increased in conventional cycle, and hypothesizes that this is due to an increased incidence of mitotic errors with high doses of gonadotropins [19]. She interestingly comments that the long GnRH agonist protocol shuts down the mechanisms of early follicular recruitment, while milder protocols maintain this mechanism. Sekhon looked at 1122 cycles and noted that patients who required a prolonged stimulation had an elevated risk of aneuploidy with an increasing gonadotropin dosage [20]. Finally, Wu looked at 1088 cycles and found no association with total gonadotropin dosage and aneuploidy rates [21]. With regard to potential oocyte quality, Baker found that as total gonadotropin dose increases, pregnancy rates decrease [22].
To conclude and well stated by Inge, it still only takes one oocyte/embryo to produce a baby, irrespective of level of stimulation. Then the goal is still to find and identify the right oocyte/embryo [7].
9.4 Patient Population
Classically, natural cycle IVF has been thought of either as the historical initial approach to IVF or as a similarly effective, cheaper, and more patient-friendly approach than conventional stimulation for women with POR due to either poor ovarian response, DOR, or ARA. As more data are gathered on this method in different patient populations, clarity has been gained on populations that would benefit the most from its use.
Natural cycle IVF may be an appealing option for those patients who wish to avoid the use of medications for ovarian stimulation. It can also be an option for those opposed to the creation of excess embryos. Natural cycle IVF may also be the safest option in those who are at very high risk of ovarian hyperstimulation syndrome.
With regard to poor ovarian response, both Gordon and Ho suggest that natural cycle is best suited for ovulatory women with normal ovarian reserve testing and normal ovarian response to stimulation [23, 24]. Ho further comments that natural cycle may be a better second-line option in poor ovarian responders after they have failed conventional ovarian stimulation [24]. Datta comments that conventional IVF does not appear to be superior to natural cycle IVF in women with poor ovarian response [6]. Shaulov draws a line at older women with POR, who show very poor outcomes with modified natural cycle IVF, and rather states that MNC-IVF is a reasonable option for both normal and poor ovarian responders ≤ 35 years old and normal ovarian responders ≥36 years old [18]. Kadoch suggests that natural cycle can be considered as a first-line therapy in young poor ovarian responders [25]. Meanwhile, Papathanasiou does not believe there are enough data to make a final conclusion on the place of natural cycle in women with poor ovarian response [26], and Lainas rejects its use in women with POR [17].
Finally, women with poor ovarian response may have elevated basal levels of follicle-stimulating hormone. Chapters in this book will discuss the relationship of elevated basal FSH and IVF cycle outcome. In these cases, alternative protocols, such as luteal phase mild stimulation or long GnRH agonist suppression with estrogen priming and mild stimulation protocols, may be of benefit.
9.5 Conclusion
Natural cycle IVF involves various approaches. Natural cycle IVF may be an option for those patients who wish to avoid the use of medications for ovarian stimulation, those opposing to the creation of excess embryos, and, lastly, in those who are at very high risk of ovarian hyperstimulation syndrome. The women with expected POR or those with DOR may also show some benefits as compared to conventional IVF especially in women younger than 36 years of age with reliable menstrual cycles. Some women with ARA may also benefit. These approaches may require multiple oocyte retrieval cycles. More data are needed to compare its efficacy as compared to other stimulation protocols suggested for women with expected POR such as those with DOR and ARA.

Full access? Get Clinical Tree


