Chapter 643 Cutaneous Nevi
Nevus skin lesions are characterized histopathologically by collections of well-differentiated cell types normally found in the skin. Vascular nevi are described in Chapter 642. Melanocytic nevi are subdivided into 2 broad categories: those that appear after birth (acquired nevi) and those that are present at birth (congenital nevi).
Acquired Melanocytic Nevus
Prognosis and Treatment
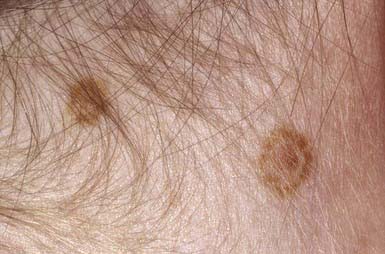
Acquired pigmented nevi are benign, but a very small percentage undergoes malignant transformation. Suspicious changes are indications for excision and histopathologic evaluation; they include rapid increase in size; development of satellite lesions; variegation of color, particularly with shades of red, brown, gray, black, and blue; pigmentary incontinence; notching or irregularity of the borders; changes in texture such as scaling, erosion, ulceration, and induration; and regional lymphadenopathy. Most of these changes are due to irritation, infection, or maturation; darkening and gradual increase in size and elevation normally occur during adolescence and should not be cause for concern. Two common benign changes are clonal nevi (fried-egg moles) and rim nevi. A clonal nevus is light brown with a dark raised center representing a clonal change of a subset of nevus cells within the lesion. Rim nevi are flat and light brown with dark brown rims. They are seen primarily in the scalp (Fig. 643-1). Consideration should be given to the presence of risk factors for development of melanoma and the patient’s parents’ wishes about removal of the nevus. If doubt remains about the benign nature of a nevus, excision is a safe and simple outpatient procedure that may be justified to allay anxiety.