Figure 19-1
Systemic lupus erythematosus Figures 19-1 and 19-2 illustrate cutaneous involvement of systemic lupus erythematosus (SLE) in the classic butterfly pattern on the face. This macular and intensely erythematous eruption is frequently aggravated by sun exposure and may flare with other symptoms of systemic disease.

Figure 19-2
This autoimmune disease of unknown etiology affects almost every organ system. The most common findings in the child with SLE are fever, arthralgias, and arthritis. In addition, pleuritis, pericarditis, and central nervous system involvement are frequently seen in children with SLE. Lupus nephritis develops in the vast majority of affected children and may eventually cause renal failure.

Figure 19-3
Systemic lupus erythematosus These figures illustrate additional cutaneous features of SLE. The lesions on the back (Fig. 19-3) and the hands (Fig. 19-4) are intensely erythematous macules and slightly edematous papules and plaques. Childhood SLE occurs most frequently during adolescence and is more common among African-Americans and among girls.

Figure 19-5
Systemic lupus erythematosus Figure 19-5 shows the temporary alopecia that is also a hallmark of SLE. The single most reliable laboratory test for SLE is antinuclear antibody which will be positive in almost every case of childhood SLE. Other laboratory criteria include leukopenia, thrombocytopenia, and the presence of antinative DNA antibodies.
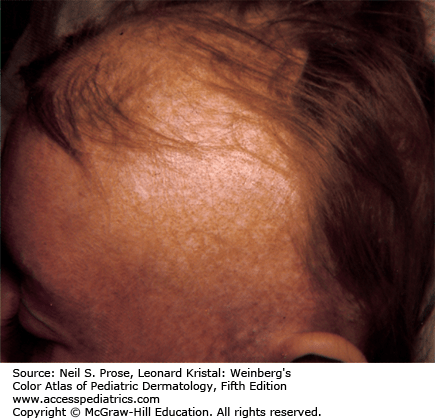
Figure 19-6
Involvement of the distal fingers is a common occurrence in children with SLE. Findings include telangiectasia of the nail folds, splinter hemorrhages, and digital infarcts as shown in Fig. 19-6.

Figure 19-7
Systemic lupus erythematosus vasculitis Cutaneous vasculitis occurs commonly in patients with SLE. The vasculitis may lead to ulceration as shown in Fig. 19-7.
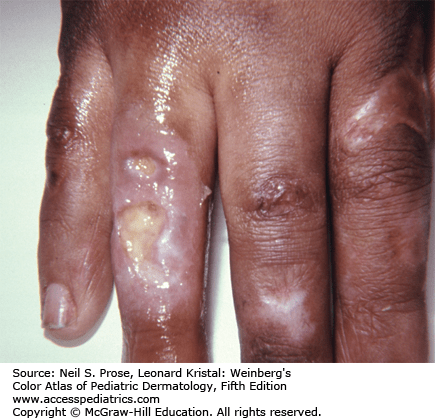
Figure 19-8
Neonatal lupus erythematosus This condition is primarily due to the transplacental passage mainly of anti-Ro (anti-SS-A) antibodies from mother to infant. Maternal anti-La (anti-SS-B) and anti-RNP antibodies may be implicated. The mother may herself suffer from a form of connective tissue disease or may be completely asymptomatic.

Figure 19-9
The infants pictured in Figs. 19-8 and 19-9 were born with these atrophic and telangiectatic plaques on the face. Symmetrical involvement of the skin around the eyes is one common pattern. The skin lesions, which are slightly more common in girls, tend to resolve without scarring. Nonfluorinated topical steroids and avoidance of the sun are the only treatments that may be required.

Figure 19-10
Neonatal lupus erythematosus Figure 19-11 shows the atrophic telangiectatic changes that are most often seen on the temple and scalp, and which may lead to permanent alopecia.

Figure 19-11
A frequent complication of neonatal lupus is congenital heart block, which may be found in utero. This situation is potentially life threatening and may sometimes require implantation of a pacemaker. Although neonatal lupus is self-limited, there are reports of affected infants going on to develop connective tissue disease during adolescence.

Figure 19-12
Discoid lupus erythematosus Figures 19-12 and 19-13 show the characteristic plaques of discoid lupus erythematosus. There is a violaceous hue at the border and central atrophy with scarring. Similar involvement in the scalp can cause permanent alopecia.

Figure 19-15
Illustrated in Fig. 19-15 is a plaque of discoid lupus erythematosus involving the pinna of the ear. Lesions are commonly found in this location, and also within the conchal bowl of the ear.

Figure 19-16
Dermatomyositis This collagen vascular disease is characterized by a combination of symmetrical proximal upper and lower extremity muscle weakness and cutaneous disease. Early symptoms of muscle involvement include general malaise, difficulty in playing or climbing stairs, myalgias, and muscle tenderness.

Figure 19-17
Figures 19-16 and 19-17 show symmetrical, intense erythema and edema of the face. The violaceous color of the periorbital rash is sometimes described as heliotrope in hue; the edema is so intense that it makes the face look puffy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





